Translate this page into:
Volumetric bone mineral density and serum 25-hydroxyvitamin D status in the UK dwelling Arab, Caucasian, and South Asian women
Address for correspondence: Dr. Khulood Hussein, Department of Physiology, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia. Mobile: +966505358188. E-mail: Khussein@kau.edu.sa
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
Little is known about ethnic differences in bone geometry, nor their association with 25-hydroxyvitamin D (25(OH)D), especially among ethnicities living in the same country. The purpose of this preliminary study was to investigate differences in bone geometry at the radius and tibia, as well as in 25(OH)D status, between Arab (A), South Asian (SA), and Caucasian (C) premenopausal women residing in the UK. The potential association between 25(OH)D concentration and indices of bone geometry was also assessed.
Methods:
Fifty-seven healthy premenopausal women (17 A, 18 SA, and 22 C), ranging in age from 18 to 51 years, underwent assessment of their volumetric bone mineral density and 25(OH)D concentration. Ethnic differences were assessed using ANOVA. Spearman’s rho was used to analyze associations between 25(OH)D and pQCT bone variables.
Results:
At the 4% radius, Arab women had a lower BMC, as well as a smaller total bone area and trabecular area than did Caucasian women. At the 4% tibia, Arab women had a lower total vBMD than did South Asian women. Serum 25(OH)D among Arab (36.5(22.4SD)) and South Asian (31.4 (16.8SD)) women was significantly lower than in Caucasian women (81.9(20.0SD)) (P < 0.05). There were no statistically significant correlations between 25(OH)D and pQCT bone variables in any ethnic group.
Conclusions:
This study suggests a possible need for attention to bone health in premenopausal Arab women as well as improvement in Vitamin D status in Arab and South Asian populations.
Keywords
25-hydroxyvitamin D
Arab
Bone mineral density
ethnicity
pQCT
premenopausal women
South Asian

Introduction
Vitamin D deficiency is a major health problem globally, although it has not been declared a health emergency by international health authorities.[1] This deficiency is a cause for concern among women in Arab countries despite the abundance of sunlight for most of the year. A Saudi study reported that 80% of healthy women living in Jeddah exhibited Vitamin D deficiency (25(OH)D <50.0 nmol/L), attributed to obesity, low sun exposure, low Vitamin D intake, and older age.[2] Reduced sun exposure may occur due to the overly hot climate and clothing covering the skin. This is compounded by a lack of food fortification with calcium and Vitamin D, and a low consumption of naturally rich sources of Vitamin D, such as oily fish, leading to Vitamin D deficiency. There are little published data on the 25(OH)D status of Arab populations living in high latitude Western countries, who are also at high risk of deficiency due to low sun exposure to the skin stemming from dress style and the additional factor of latitude as well as little Vitamin D in the diet. Low 25(OH)D has been reported in Arab children living in Germany and in Arab men and women in the US.[3-5] More research is now required into 25(OH)D status in Arab populations living in other Western, high latitude countries.
Vitamin D deficiency is a known risk factor for poor bone health. The previous studies have confirmed that young healthy Saudi Arab females have low areal bone mineral density (aBMD), likely due in part to insufficient calcium intake and insufficient sun exposure.[6] Research has also highlighted the elevated prevalence of osteoporosis in the Saudi female population.[7] Some studies have assessed bone health of Arab women living in the Western world. For example, in the United States (US), Saudi females were shown to have lower weight-matched Z scores at the spine, femoral neck, and Ward’s triangle compared to their US counterparts, which the authors suggested were likely due to increased numbers of pregnancies and long duration of lactation alongside Vitamin D deficiency.[8] In terms of other Middle Eastern countries, studies have found that the Qatari 60–69-year-old female population also have lower total femur BMD, compared to Caucasian, Kuwaiti, Lebanese, and Saudi women, but 40–59-year-old Qatari women have higher values compared to the same ethnic groups.[9] Another study found no differences in aBMD between Kuwaiti and Caucasian women at the lumbar spine and proximal femur.[10]
However, most studies of Arab women have not looked in detail at other aspects of bone geometry beyond aBMD, nor have they looked at women of a younger age, despite the potential benefit of early identification and intervention in this group. There is also a need for more studies in Arab women living in the Western world to assess in greater detail the differences in cortical and trabecular bone structure that exists compared with other ethnic groups. Similarly, more data are required on bone health in South Asian women, particularly those dwelling in Western countries who are known to have a high risk for Vitamin D deficiency as well as a low calcium intake, for the same reasons as those listed above for Arab women.[11]
Indeed, recent work suggests high rates of Vitamin D deficiency in Western dwelling South Asian women, of both postmenopausal and premenopausal status.[12-15] Few studies have assessed bone health in Western dwelling South Asians, but the previous studies found that variations in aBMD between Caucasian and South Asian premenopausal women could be explained simply by differences in bone size.[16,17] However, one study, using peripheral quantitative computed tomography (pQCT) in postmenopausal women, identified poorer bone strength in women of South Asian heritage, evidenced by a 20% reduction in the polar strength-strain index (SSIp) and a 40% reduction in predicted fracture load (under bending), compared to Caucasian women.[13] Similarly, another pQCT study reported a smaller radial cross-sectional area and lower volumetric bone mineral content (BMC), volumetric BMD (vBMD), cortical thickness, and cortical area in South Asian premenopausal women compared to same age European women, differences which could not be accounted for by ethnic differences in body size.[17] However, Roy et al. reported similar radial vBMD in premenopausal South Asian women compared with their Caucasian peers, demonstrating inconsistencies in the published literature.[16]
To date, few studies have looked in detail at other aspects of bone health beyond aBMD in South Asian women, with none assessing tibial pQCT in premenopausal women of this ethnic group and none assessing either radial or tibial pQCT in any age group in Arab women. It is crucial to be aware of bone geometry in South Asian and Arab premenopausal women to recognize risk factors for fracture in these groups, as well as to optimize diagnosis and treatment for osteoporosis in later life. The present study assesses ethnic differences in pQCT derived bone variables in Western dwelling Arab (A), South Asian (SA), and European Caucasian (C) premenopausal women. It also investigates serum 25(OH)D status in these ethnic groups and examines whether there is a link between pQCT-derived bone variables and 25(OH)D status.
Methods
Study population
The original Vitamin D, Food Intake, Nutrition, and Exposure to Sunlight in South England (D-FINES) study ran from 2008 to 2010 and included data from 373 women (n = 279 Caucasian women: 144 post-menopausal and 135 pre-menopausal, and n = 94 South Asian women: 44 postmenopausal and 50 premenopausal) to investigate seasonal variation in 25(OH)D (Ethical Approval Number: University of Surrey EC/2008/19/SBMS, National Health Service (NHS) Research Ethics Committee (REC) 10/H/1109/25). Details of this cohort have been published in detail elsewhere.[13] The original cohort was reinvited in summer 2012 to participate in further investigations, including remeasurement of 25(OH)D status, anthropometrics, and pQCT measurement of the radius and tibia. Study reinvitation letters were sent to all 375 women and a total of 117 responses were received (75 postmenopausal and 43 premenopausal). Forty-two premenopausal healthy females were recruited to the new study (n = 22 Caucasian and n = 18 South Asian). Data for postmenopausal women have been published previously.[13]
In summer 2013, 17 premenopausal Arab women were recruited from local universities (London and South of England) and underwent exactly the same measurements and tests as the 22 Caucasian and 18 South Asian women had in 2012. Most of the Arab women were from Saudi Arabia but were living in the UK for educational reasons, having lived in the UK for at least 2 years before the study. Ethical approval was given by the University of Surrey Research Ethics Committee (UEC/2012/006/SBMS). Written and informed consent was given by all participating women, and all researches were carried out in accordance with the Declaration of Helsinki. Ethnicity was self-reported.
Study measures and methodology
Serum concentrations of 25OHD were measured by the Supra-Regional Assay Laboratory, Manchester, as previously described.[18] Briefly, following extraction and purification, serum 25(OH)D2 and 25(OH)D3 were measured separately by straight phase HPLC (Waters Associates, Milford, MA) using a Hewlett-Packard Zorbax-Sil Column (Hicrom, Reading, Berkshire, UK) eluted with hexane: propan2ol (98:2) run at 2 mL/min and quantified by UV absorbance at 265 nm and corrected for recovery. Sensitivity was 5 nmol/L and interassay variation was 6%. The laboratory was accredited to ISO standards 9001:2008 and ISO 13285:2003 followed by CPA certification (0865) and participated successfully in the Vitamin D quality assurance program (DEQAS).
Bone indices were measured using a Stratec Medizintechnik GmbH XCT2000L bone densitometer scanner. Radiation regulations at both the national and local level were followed, and all investigators had relevant radiation training before operating the scanner. Details of the scanning process have been previously published but briefly, pQCT measurements were taken at two sites of the non-dominant radius (the 4% distal radius and the 66% diaphyseal radius) and three sites of the non-dominant tibia (the 4% distal tibia, 14% diaphyseal tibia, and 38% mid-shaft tibia).[13]
Predicted fracture load was calculated by the software using the following equation:
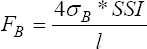
Where, FB = Fracture load [N]; σB = Ultimate load = 180 Mpa; and l = Distance between supports.
The strength strain index was calculated as:
Where, CD = Measured cortical density (mg/cm2) and ND = Normal physiological density (1200 mg/cm3) (Source: Stratec manual 6/11/9 Man62e.doc).
The total amount of radiation for each scan (either radius or tibia) was <2 micro-Sieverts (μSv). The pQCT machine underwent weekly calibration using a quality control phantom.
Statistical analysis
All statistical analyses were conducted using SPSS 23 (SPSS Inc., Chicago, US). Ethnic differences in pQCT bone indices and serum 25(OH)D were assessed using one-way analysis of variance (ANOVA). Analysis of covariance (ANCOVA) was also performed on any pQCT variable which showed statistically significant ethnic differences during ANOVA testing, to control for the possible confounding effects of age, BMI, and height. We did this as two ANCOVA models, the first for age and BMI, the second for age and height. We did not put BMI and height in the same model due to the known strong correlation between these two variables. Associations between 25(OH)D and pQCT bone variables were undertaken using Spearman’s rho correlation due to 25(OH)D not being normally distributed. Partial correlations, controlling for key confounders, were not undertaken as no results from the Spearman’s rho analyses were statistically significant. Bonferroni correction was used to adjust the initial P value cutoff (P ≤ 0.05) to account for multiple testing.
Results
Participant baseline characteristics
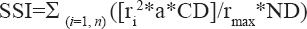
Fifty-seven women, including n = 22 Caucasians, n = 18 South Asians, and n = 17 Arabs, took part in the study. Results are presented as mean (SD) unless otherwise stated. The Arab women were significantly younger (by 11–15 years) than the South Asians and Caucasian women (A: 26 (5) years; SA: 41(8) years; and C: 37 (5) years; P < 0.001). Caucasian women were significantly taller (by 7 cm) than Arab and South Asian SA women (C: 166 (6) cm; A: 160 (6) cm; and SA: 160 (5); P < 0.001). However, weight and BMI did not vary to a statistically significant extent between the ethnic groups [Table 1], the Arab and South Asian groups were classified as overweight on average (BMI 26−29 kg/m2), with the mean BMI in the Caucasian group being at the top of the normal range (18–25 kg/m2).
Differences in pQCT bone indices between ethnic women groups
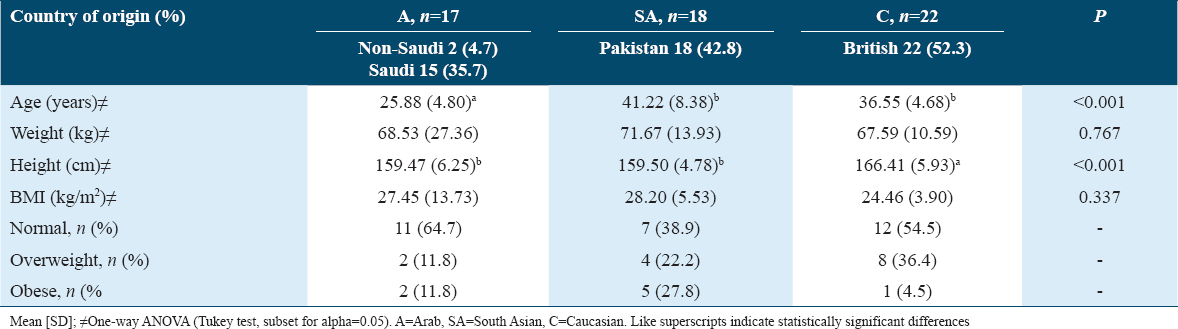
Table 2 shows the results for pQCT bone indices and ANOVA results at the 4% and 66% radius among the three ethnic groups. After Bonferroni adjustment for multiple testing, using a revised cutoff for P of ≤ 0.002 (21 tests for radius), only ethnic differences in BMC, total area, and trabecular area at the 4% radius remained statistically significant. The Caucasian women had higher BMC, total area, and trabecular area than Arab and South Asian women, but Tukey’s post hoc tests confirmed that the only statistically significant differences were those observed between Arab and Caucasians. There were no statistically significant ethnic differences for any variables at the 66% radius. ANCOVA showed that, after adjusting for age and BMI, the ethnic difference for 4% radius BMC (P = 0.001), total area (P = 0.001), and trabecular area (P = 0.001) maintained its statistical significance. Similarly, after adjusting for age and height, the ethnic difference for 4% radius total area (P = 0.001) and trabecular area (P = 0.001), but not BMC (P = 0.004), remained statistically significant.
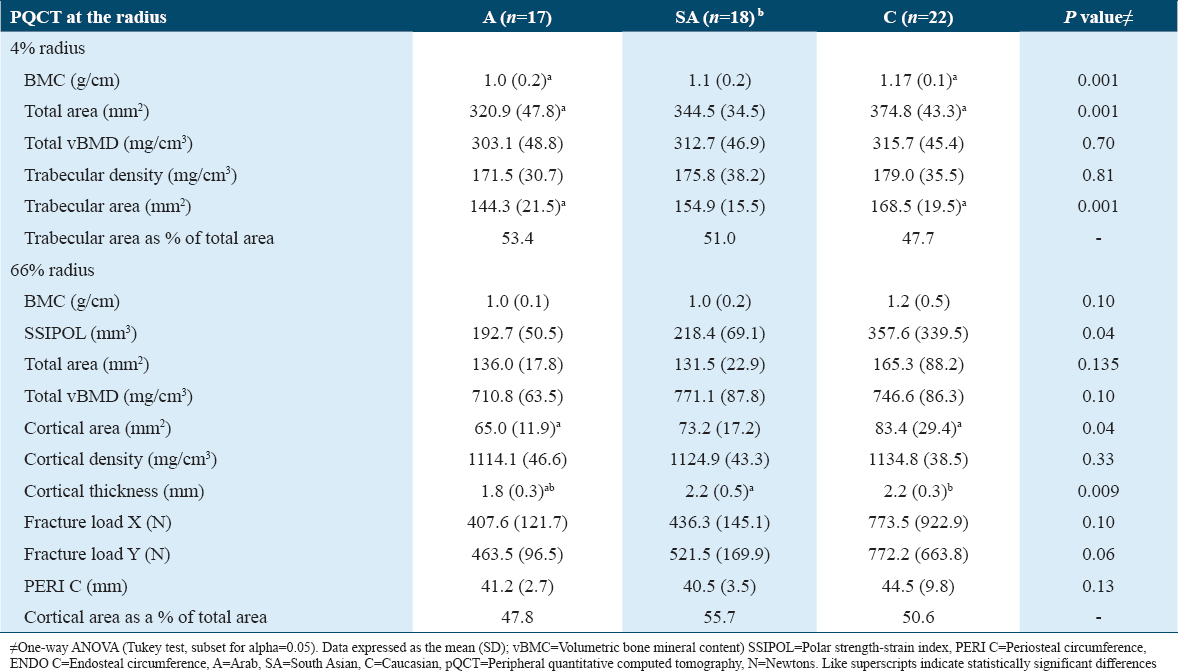
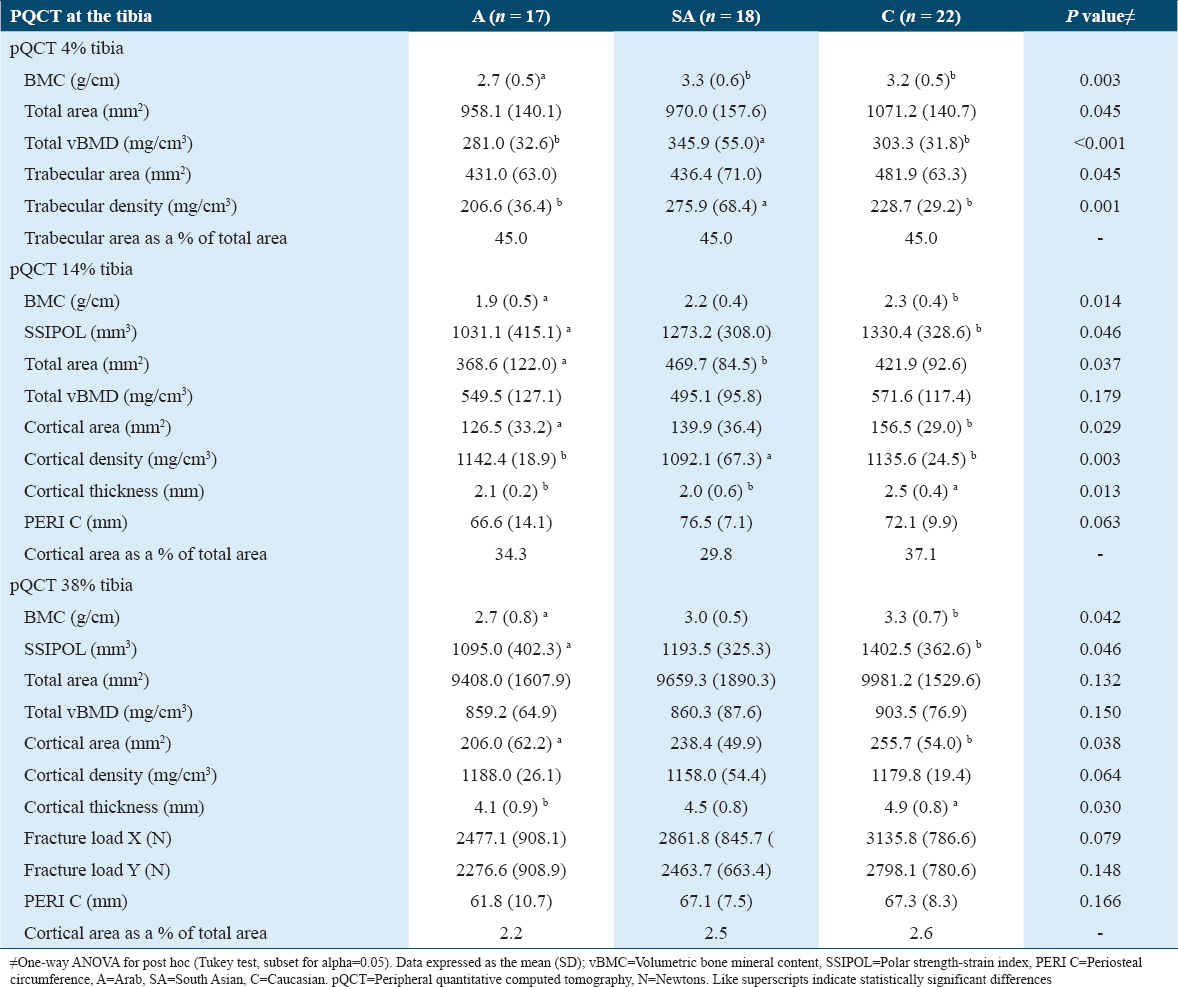
Table 3 illustrates results for the tibial pQCT bone indices (4%, 14%, and 38% sites) and ANOVA results among the three ethnic groups. After Bonferroni adjustment for multiple testing, using a revised cutoff for P of ≤0.002 (25 tests for tibia), only ethnic differences in total vBMD at the 4% tibia remained statistically significant, with Tukey’s post hoc tests showing a statistically significant difference in total vBMD between the Arab and South Asian women only (Arabs had only 82% of the total vBMD of South Asians). ANCOVA confirmed that the ethnic difference in total vBMD remained statistically significant when BMI and age were controlled for P = 0.001, n = 15 A, n = 13 SA, and n = 21 C as well as when height and age were controlled for P = 0.002, n = 15A, n = 13 SA, and n = 21 C.
25(OH)D concentration
In terms of percentage of women under different 25(OH)D cutoff points, 33% of Arabs, 29% of South Asians, and 0% of Caucasians had 25(OH)D concentrations <25 nmol/L, with 73% of Arabs, 88% of South Asians, and 0% of Caucasians falling below the 50 nmol/L level. Finally, 93% of Arabs, 94% of South Asians, and 42% of Caucasians had 25(OH)D concentrations <75 nmol/L, and 6.7% (n = 1) of Arabs, 6.0% (n = 1) of South Asians, and 58.0% of Caucasians had 25(OH)D ≥75 nmol/L. South Asians women had the lowest level of 25(OH)D (31.4 (16.8) nmol/L, n = 17), followed by Arab women (36.5 (22.4) nmol/L, n = 15), with both groups being classified on average as insufficient (<50 nmol/L). The highest 25(OH)D levels were in the Caucasian women who were classified as sufficient (≥50 nmol/L) on average (mean 25(OH)D 81.9 (20.0) nmol/L, n =19). One-way ANOVA showed a statistically significant difference in 25(OH)D between the three groups (P < 0.001). Tukey’s post hoc tests showed that Caucasian women had significantly greater 25(OH)D levels than both their Arab and South Asian counterparts (P < 0.05) by 45.4 nmol/L and 50.5 nmol/L, respectively, but there were no other statistically significant group differences.
Association between pQCT indices and 25(OH)D within ethnic groups
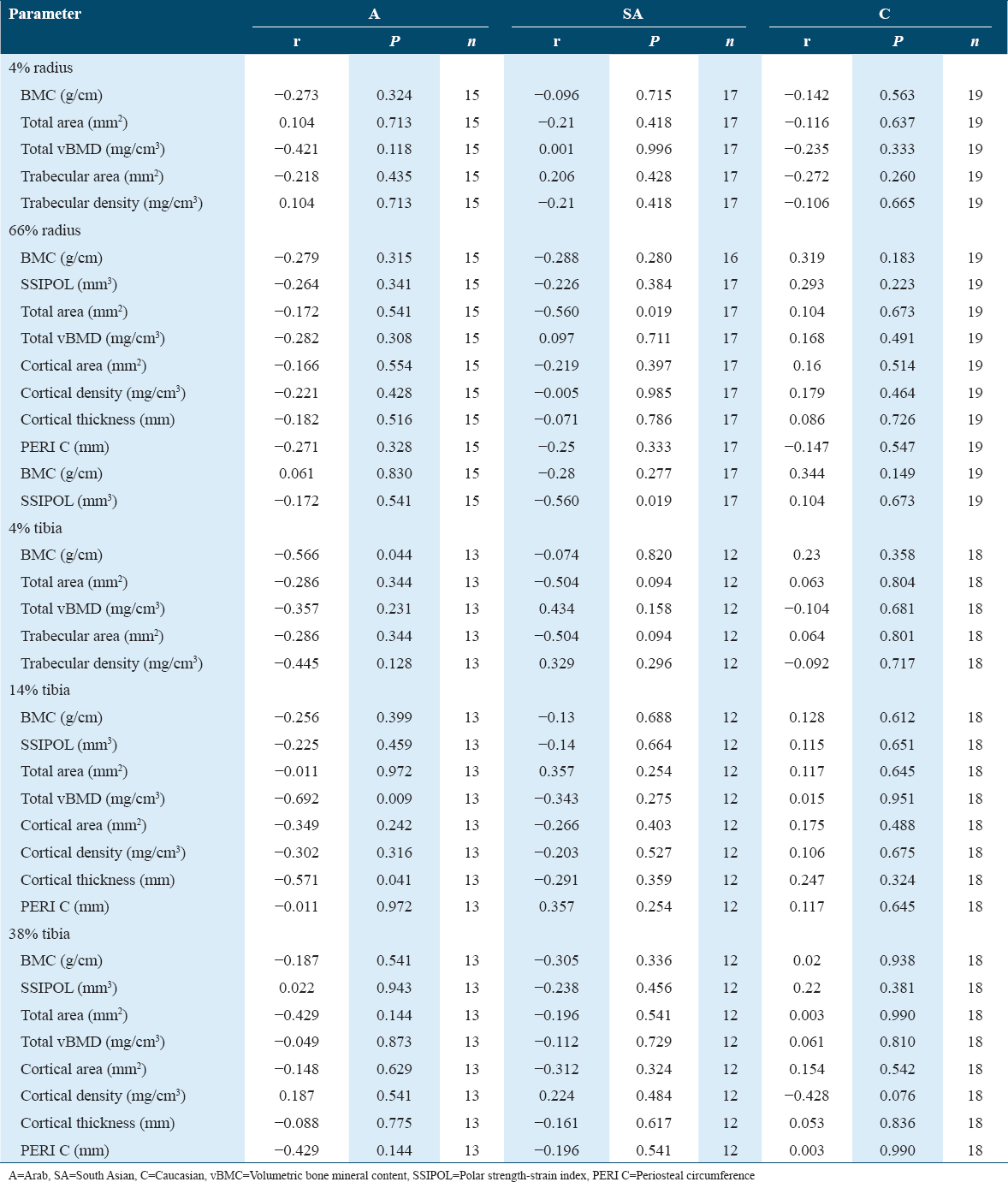
Table 4 shows the full details of the Spearman’s rho correlations between all pQCT indices and 25(OH)D in each ethnic group. After Bonferroni adjustment for multiple testing, using a revised cutoff for P of ≤0.0005 (108 tests), there were no statistically significant correlations between 25(OH)D and any bone parameter at either the radius or tibia, within any ethnic group.
Discussion
To summarize, this study found that premenopausal Arab women had a smaller BMC, total area, and trabecular area, compared with Caucasian women at the 4% radius, as well as a lower total vBMD than South Asian women at the 4% tibia. There were no ethnic differences in any of the bone indices at the 14% or 38% tibia sites or at the 66% radius site. For 25(OH)D status, Arab and South Asian women had lower 25(OH)D concentrations than their Caucasian counterparts, with Caucasian women having 40–50 nmol/L higher 25(OH)D levels, a 2.3–2.6 times or 29–33% greater than Arab and South Asian women with Vitamin D deficiency (25(OH)D <25 nmol/L). There was no relationship in this study between 25(OH)D and bone indices, for any bone parameter, in any of the ethnic groups.
At the 4% radius, our finding in Arab women of a lower BMC, total area, and trabecular area, compared with Caucasian women, is novel as, to the author’s knowledge, there have been no published pQCT data for Arab women of any age. Total and trabecular areas, as well as BMC, were 85% of that of Caucasian women. These ethnic differences remained, after controlling for age, height, and BMI, suggesting that these potential confounders did not explain these results. The one exception was when controlling for age and height, the ethnic difference in BMC was no longer statistically significant, suggesting that differences in skeletal size may explain the lower radial BMC in Arab women. It can be concluded that we found that Arab women have smaller radial size than Caucasian women, and this explains the lower BMC observed. Particularly, there are no differences in density which would render the Arab women at increased fracture risk, although a smaller skeletal size will in itself reduce bone strength and may increase fracture risk.
No ethnic difference for total radial bone density between any of the three groups, which concurs with the results of Ward et al. (2007), who noted no difference in this parameter between South Asian and Caucasian premenopausal women.[17] However, unlike the previous study, South Asian women in the present study did not have higher trabecular density than Caucasian women.[17] This may be because the previous study had a larger sample size and their finding was reached only after controlling for a variety of factors including 25(OH)D status, something not done in this study. Furthermore, the present findings do not support the study by Zengin et al. who studied Black, South Asian, and Caucasian males and who found smaller radial bone size at the 4% radius, as well as lower cortical thickness and cortical area at the 50% radius in South Asian men compared with Caucasian men.[19] It could be that some ethnic differences are gender specific, but the differences between studies may also be due to the older age (around 60 years) of the men.[19] Finally, this present work concurs with that of the DXA study, in that smaller bone size in Arab women was found compared with Caucasian women.[8]
At the 4% tibia, we found a biologically meaningful result, with Arab women having a lower total vBMD than South Asian women (Arab was 82% of South Asian). This result is not likely to be a result of any differences in BMI, height (skeletal size), or age as these variables were controlled for in a subsequent ANCOVA analysis and the result remained statistically significant. The current findings contradict that of a previous study by Ghannam et al. in that no statistically significant difference in the vBMD of Arab and Caucasian women was found.[8] The discrepancy between these two studies could be due to differing methodologies. The present study used measured vBMD, which is a measure of bone density that is independent of bone size, whereas Ghannam et al. study measured aBMD, which appears lower if skeletal size is smaller, suggesting that their findings may be a function of the smaller bone size of the Arab women compared with Caucasian women.[8] However, these differences could also reflect the difference in sample size between the two studies.
In terms of explaining the reduced tibial vBMD in Arab, compared with South Asian women, lifestyle could be a contributing factor, particularly since Arab women were commonly international University students, whereas the South Asian women were not. Many of the South Asian women were second generation migrants to the UK, and so their childhood diet and activity levels are likely to differ from those who were born and raised in an Arab country.
The finding of a lower tibial vBMD in Arab women is important, as if it is also lower at clinically relevant sites (e.g., hip and spine) then this may increase the risk of osteoporotic fracture in Arab women relative to South Asian women. A high resolution pQCT (HR-pQCT) study found that Caucasian postmenopausal women with previous fragility fracture had a 3% lower distal tibial vBMD than those without previous fragility fracture.[19] Although the data are not directly comparable, this does suggest that the present finding of a 7% lower vBMD in Arab than in South Asian women may be clinically relevant, in that Arab women may be at higher risk of fragility fractures than South Asian women in later life.
The present results showing a higher 25(OH)D status in Caucasian women, as compared to their South Asian and Arab peers, agree with the previous studies that have found that Western dwelling South Asians are at high risk of vitamin deficiency and that their Vitamin D status is significantly lower than that of European Caucasians.[13,20] The low 25(OH)D status found in the Arab women in the present study supports other work showing lower 25(OH)D in Arab children in Germany and in Arab men and women in the US.[5,16,17] Equally, the findings of the present study are in line with work showing that young Saudi females are more Vitamin D deficient compared to non-Saudi groups.[21]
A major explanation for the lower 25(OH)D concentration in South Asian and Arab women is the lack of sunlight exposure, which stems from traditional cultural norms and beliefs. Women in these cultures may fear getting tan or having skin damage from the effects of sunlight. Furthermore, for modesty reasons, both Arab and South Asian women cover most of the skin when they go out of the house, which will limit endogenous production of Vitamin D in the skin. Indeed, previous work by the D-FINES researchers found increased UVB exposure in Caucasian compared with South Asian premenopausal women and deliberate avoidance of sun exposure is known among South Asian women living in Western countries.[13,21]
Another explanation is that Arab and South Asian cultures are limited in terms of Vitamin D content in traditional foods. There is a lack of research comparing dietary differences between Arab, South Asian, and Caucasian women, but one can speculate that Caucasian women may tend to eat more Vitamin D-rich sources of food (e.g., oily fish and eggs) than South Asian women (who were mainly of Pakistani origin, so do not traditionally consume a lot of fish) and Arab women (who also do not eat a diet high in oily fish and eggs).
No statistically significant association was found between any bone parameter and 25(OH)D status, at either the radius or the tibia, in any of the ethnic groups, even those groups who had some degree of Vitamin D deficiency (Arab and South Asian women). The lack of a correlation seen in this study in Arab women between 25(OH)D status and total bone density agrees with the results of a study of Saudi women living in Riyadh by Hussain et al. (2014), where no significant correlations between spine or total femoral aBMD and serum 25(OH) D were found.[22] It also agrees with the lack of correlation between 25(OH)D and spine or hip aBMD, as reported by Ghannam et al. (1999).[8] Alkenizan et al. (2017) suggested differences between such studies could be due to geographic differences in climate, environment, and local customs.[23] However, the current findings do not agree with the findings of a weak association between some HR-pQCT variables and 25(OH)D in a Caucasian population, as well as between 25(OH)D status and hip aBMD in South Asians living in South Africa.[24,25] The results are very inconsistent in the literature, and the link between 25(OH)D and bone indices may vary by a wide range of factors.
Overall, premenopausal Arab women may be at higher fragility fracture risk in later life, with some indicators of poorer bone geometry at the 4% radius and tibia sites, compared to other ethnic groups. Further research is now required into the bone health of Arab women living in western countries, including the UK, using a larger sample size and a more representative Arab population. Many South Asian and Arab women have been found to be deficient in 25(OH)D, and there is a clear need for strategies to improve 25(OH)D status in these groups in the UK. Strategies to increase access to Vitamin D food sources could include food fortification, especially if applied to commonly consumed items such as rice and bread. The promotion of Vitamin D supplements could also be considered, and where cultural and religious requirements permit, increased consumption of naturally Vitamin D containing foods (e.g., oily fish and eggs).
This study is the first to investigate differences in pQCT assessed bone variables among Arab premenopausal women. Its approach is also novel in its comparison of three ethnic groups – Arabs, South Asians, and Caucasians – living in the same country. One limitation is related to the sample size. Although the sample size in each group was relatively small, the number of women was similar across the three groups. The inclusion criteria for the South Asian and Arab groups were individuals who had been in the UK for more than 2 years, so they were recently exposed to the same environmental factors (e.g., sunlight availability) as the Caucasian women. However, it is worth noting that the Arab women had not lived in the UK for more than 4 years (the duration of their university course) and being international university students, they probably came from a more affluent background than their South Asian and Caucasian peers. The Arab women were mostly from Saudi Arabia, and the South Asian women were mostly of Pakistani heritage (first- and second- generation immigrants), so they may not be representative of other Arab or South Asian cultural backgrounds. In addition, most of the South Asian women spoke fluent English, and lived in areas of the country with a low to moderate index of multiple deprivation, so they may not represent the whole UK South Asian female population. Similarly, the Arab women are not likely to be representative of all Arab women living in the UK, having only lived in the UK for a few years, being of a specific age range, of affluent status and able to speak English fluently. More research is needed into the bone health of the broader UK Arab female population.
Another limitation of the study is that the measurements of the bone scans and 25(OH)D status for Arab women were not carried out in the same year as for the South Asian and Caucasian participants; however, the data collection was conducted in the same season of the year. Finally, the data were from summer, so the recorded 25(OH)D status may actually be an underestimate of the true scale of Vitamin D deficiency seen in the Arab and South Asian groups, which are likely to be even more severe in winter and spring.
Conclusions
This study is novel in its focus on premenopausal women of three ethnic groups living in the UK. It adds to the findings of overall lower 25(OH)D status and related bone health in Arab and South Asian women. Specifically, Arab women had lower BMC and smaller total area and trabecular area than Caucasian women at the 4% radius. They also had a lower total vBMD than South Asian women at the 4% tibia, which may be detrimental to bone strength. South Asian and Arab women had reduced 25(OH)D concentrations compared to Caucasian women and a third were deficient (<25 nmol/L). There was no correlation between 25(OH)D and bone indices. Our findings regarding lower tibial vBMD in Arab women suggest a detriment to bone health and warrant further investigation with a larger sample size, and within a more representative group of Western dwelling Arab women. The low 25(OH)D status in South Asian and Arab women is a particular cause for public health concern and approaches are urgently needed to tackle this problem.
Acknowledgments
The author would like to thank all the women who agreed to participate in this study.
References
- Vitamin D status in relation to obesity, bone mineral density, bone turnover markers and vitamin D receptor genotypes in healthy Saudi pre-and postmenopausal women. Osteoporos Int. 2011;22:463-75.
- [Google Scholar]
- Higher prevalence of vitamin D deficiency is associated with immigrant background among children and adolescents in Germany. J Nutr. 2008;138:1482-90.
- [Google Scholar]
- Serum 25-hydroxy vitamin d and insulin resistance, metabolic syndrome, and glucose intolerance among Arab Americans. Diabetes Care. 2010;33:1373-5.
- [Google Scholar]
- Severe vitamin D deficiency in Arab-American women living in Dearborn, Michigan. Endocr Pract. 2009;15:35-40.
- [Google Scholar]
- Low bone mineral density among young healthy adult Saudi women. Prevalence and associated factors in the age group of 20 to 36 years. Saudi Med J. 2016;37:1225-33.
- [Google Scholar]
- Genetic influence of vitamin D receptor gene polymorphisms on osteoporosis risk. Int J Health Sci(Qassim). 2020;14:22-8.
- [Google Scholar]
- Bone mineral density of the spine and femur in healthy Saudi females:Relation to vitamin D status, pregnancy, and lactation. Calcif Tissue Int. 1999;65:23-8.
- [Google Scholar]
- Bone density measured by dual energy X-ray absorptiometry in Qatari women. Maturitas. 2005;52:319-27.
- [Google Scholar]
- Bone density measured by dual-energy X-ray absorptiometry in healthy Kuwaiti women. Calcif Tissue Int. 2001;68:225-9.
- [Google Scholar]
- Nutrient intakes of an adult Pakistani, European and African-Caribbean community in Inner city Britain. J Hum Nutr Diet. 2003;16:327-37.
- [Google Scholar]
- Sunlight and dietary contributions to the seasonal vitamin D status of cohorts of healthy postmenopausal women living at northerly latitudes:A major cause for concern? Osteoporos Int. 2011;22:2461-72.
- [Google Scholar]
- Vitamin D deficiency in UK South Asian women of childbearing age:A comparative longitudinal investigation with UK Caucasian women. Osteoporos Int. 2013;24:477-88.
- [Google Scholar]
- Vitamin D deficiency in western dwelling South Asian populations:An unrecognized epidemic. Proc Nutr Soc. 2020;79:259-71.
- [Google Scholar]
- Vitamin D status among immigrant mothers from Pakistan, Turkey and Somalia and their infants attending child health clinics in Norway. Br J Nutr. 2009;101:1052-8.
- [Google Scholar]
- Differences in peak bone mass in women of European and South Asian origin can be explained by differences in body size. Osteoporos Int. 2005;16:1254-62.
- [Google Scholar]
- Forearm bone geometry and mineral content in UK women of European and South-Asian origin. Bone. 2007;41:117-21.
- [Google Scholar]
- Observations from the UK Supra-regional assay service laboratory for the measurement of vitamin D metabolites. J Steroid Biochem Mol Biol. 2007;103:477-9.
- [Google Scholar]
- Ethnic differences in bone geometry between white, black and South Asian men in the UK. Bone. 2016;91:180-5.
- [Google Scholar]
- Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency:A position statement of the European Calcified Tissue Society. Eur J Endocrinol. 2019;180:P23-54.
- [Google Scholar]
- Vitamin D deficiency amongst minority ethnic groups in the UK:A cross sectional study. Int J Cardiol. 2013;167:2172-6.
- [Google Scholar]
- Increasing trends and significance of hypovitaminosis D:A population-based study in the Kingdom of Saudi Arabia. Arch Osteoporos. 2014;9:190.
- [Google Scholar]
- The relationship between 25(OH) D levels (Vitamin D) and bone mineral density (BMD) in a Saudi population in a community-based setting. PLoS One. 2017;12:e0169122.
- [Google Scholar]
- The relationship between serum 25(OH)D and bone density and microarchitecture as measured by HR-pQCT. Osteoporos Int. 2015;26:2375-80.
- [Google Scholar]
- The association between body composition, 25(OH)D, and PTH and bone mineral density in black African and Asian Indian population groups. J Clin Endocrinol Metab. 2014;99:2146-54.
- [Google Scholar]






