Translate this page into:
Prevalence, Etiology, and Fatality Rates of Childhood Heart Failure in Nigeria: A Systematic Review and Meta-analysis
Address for correspondence: Mohammed Baba Abdulkadir, Department of Paediatrics, University of Ilorin/ University of Ilorin Teaching Hospital, Ilorin, Kwara State, Nigeria. E-mail: docmohng@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
The objectives of the study were to describe the burden, etiology, and fatality rates of heart failure in Nigerian children.
Methods:
We searched PubMed database, Google scholar, TRIP database, EMBASE, African Index Medicus, and reference lists of selected articles for studies on burden, etiology, and fatality rates of heart failure in children in Nigeria published from 1977 to 2016. Two researchers reviewed the papers independently. Ten studies were selected that included 14,921 children and 1353 with heart failure.
Results:
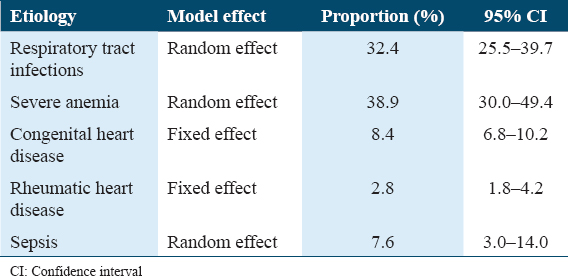
The overall prevalence of heart failure using all the studies reviewed was 8.3% (95% CI: 4.9–12.6). The prevalence was 13.4% (95% CI: 10.9–16.3) in studies that excluded neonates and 4.5% (95% CI: 2.8–6.5) in studies that included neonates. The most common causes of heart failure were severe anemia (38.9%, 95% CI: 30.0–49.4), respiratory tract infections (32.4%, 95% CI: 25.5–39.7), congenital heart disease (8.4%, 95% CI: 6.8–10.2), and sepsis (7.6%, 95% CI: 3.0–14.0). The overall fatality rate was 16.0% (95% CI: 9.0 – 24.6) and was higher in studies that include neonates.
Conclusion:
Heart failure is common in children hospitalized in Nigeria. Its etiology is largely from non-cardiac conditions associated with severe hypoxia and mortality rates are high in children in Nigeria.
Keywords
Etiology
burden
fatality rates
heart failure
Introduction
Congestive cardiac failure (CCF) occurs when the heart cannot deliver adequate blood to meet the metabolic needs of the body.[1] Globally, it is a common complication of several cardiac and non-cardiac disorders in children. Population-based data on the incidence of pediatric heart failure in sub-Saharan Africa are non-existent with available descriptions of the burden arising largely from hospital-based cross-sectional studies. It is responsible for between 10% and 33% of admissions into emergency pediatric units in Europe.[2-4] In Nigeria, it accounts for between 2.7% and 15.5% of children admitted into emergency pediatric units.[5-7]
The etiology of pediatric heart failure is diverse globally. In the developed world, congenital heart diseases and cardiomyopathies are generally the most common causes of heart failure among children.[8,9] This contrasts with the developing countries where conditions characterized by hypoxia, such as severe anemia, pneumonia, and asphyxia, are the most common causes.[10,11]
Children with heart failure suffer increased mortality. Data from the United States of America estimate that it is responsible for the deaths of 11,000–14,000 children annually with mortality rates among children with heart failure ranging between 6.9% and 8.0%. Much higher mortality rates have been recorded in hospitalized African children with heart failure. Considering the added morbidity and risk of mortality posed by heart failure, it is important to define its common causes in routine clinical practice. This will guide decisions of clinicians regarding effective management of the underlying conditions. Most studies on etiology and outcome of heart failure in Nigeria are limited by small sample sizes and limited geographical coverage.
Thus, this study was designed with the objectives of reviewing the burden of heart failure in children in Nigeria, its etiology and the fatality rates of children with heart failure over a 40-year period from 1977 to 2016.
Methods
An extensive search of existing literature was conducted using predetermined inclusion and exclusion criteria for the determination of eligibility of studies, data outcome, and the quality of the study method. The search was conducted in September 2019.
Search methods
A comprehensive literature search of the following databases: PubMed, Google Scholar, Trip database, EMBASE, and African Index Medicus were conducted using the search terms “heart failure,” “Children,” and “Nigeria.” A manual search for additional studies was performed using references cited in original study articles and reviews. Contact was established with well-known researchers on the study topic in Nigeria for possible studies that could have been missed. A hand search of local journals was also conducted. The search was limited to studies published in English language. The search was conducted independently by two researchers (MBA and RMI). Discrepancies in the studies obtained between both authors were resolved by discussion. All studies were included into an endnote database.
Eligibility criteria
Inclusion criteria were studies conducted in Nigeria that included children aged 0–18 years with a diagnosis of heart failure and were conducted between 1977 and 2016 (both years inclusive). Studies included, had to have relevant information on one or more of the following: Prevalence of heart failure, etiology of the heart failure, or case fatality/outcome in patients with heart failure.
Studies were excluded if the number of children with heart failure was <20, if they were conducted in a restricted subgroup of patients with heart failure (for example, heart failure among only children with congenital heart disease) and if the study population consisted of children and adults in which the pediatric data could not be separated. Studies involving multiple countries in which the Nigerian data could not be extracted, case reports and case series articles were excluded. Duplicate studies were removed. Each of the studies was assessed for eligibility by both authors based on the inclusion and exclusion criteria.
Data were extracted from these studies on number of children with heart failure, total number of children admitted into the unit/clinic/hospital over the study period, time period over which the children were admitted, geographical region in Nigeria where the study was conducted, number of children with each defined cause of heart failure, and number of deaths among children with heart failure. Data were extracted using a data collection tool designed by the authors using Microsoft Excel®.
Data analyses
Data analysis was conducted using Microsoft Excel® and RevMan 5® software packages. The studies were categorized based on the inclusion of exclusion of neonates within the study population. Variables were described as frequency, proportions, ratios, and rates. Frequencies for the various causes of heart failure were added up within the specified time periods and proportions (including 95% confidence intervals) of the individual conditions generated. These proportions were used in subsequent analyses. The various data obtained were displayed in standard tables depicting the burden of heart failure, frequency of the major etiologic conditions, and mortality.
Study quality
Quality of included studies was determined using the checklist by Downs and Black.[12] Studies that scored ≤14 points were ranked as “poor;” 15–19 points as “fair;” and 20–25 points as “good.”[12,13]
Results
We identified 335 studies from the initial search of PubMed, Google Scholar, translating research into practice (TRIP), and African Index Medicus databases [Figure 1]. An additional number of six studies were found using other search strategies as detailed in methods and Figure 1. Of these, 10 studies met the inclusion and exclusion criteria and were included in the review.[5-7,11,14-19]

- Study flow diagram
Using the Down and Black checklist, six studies were rated as “poor” and four studies rated as “fair.” There were no studies that were rated as “good.”
Concerning the three major thematic areas of this review, seven studies provided data on incidence of childhood heart failure among pediatric admissions, all the studies had described the major disease conditions causing heart failure and eight studies covered the outcome of pediatric heart failure.[5,6,11,14,16-18] None of the studies included adolescents aged 15–18 years of age. Two studies included apparently the same data from the same site; however, they were both included as they provided additional data (one reported mortality, while the other reported spectrum of congenital heart disease).[14,15] To avoid duplication of participants, only one study was used where both studies reported the particular data.
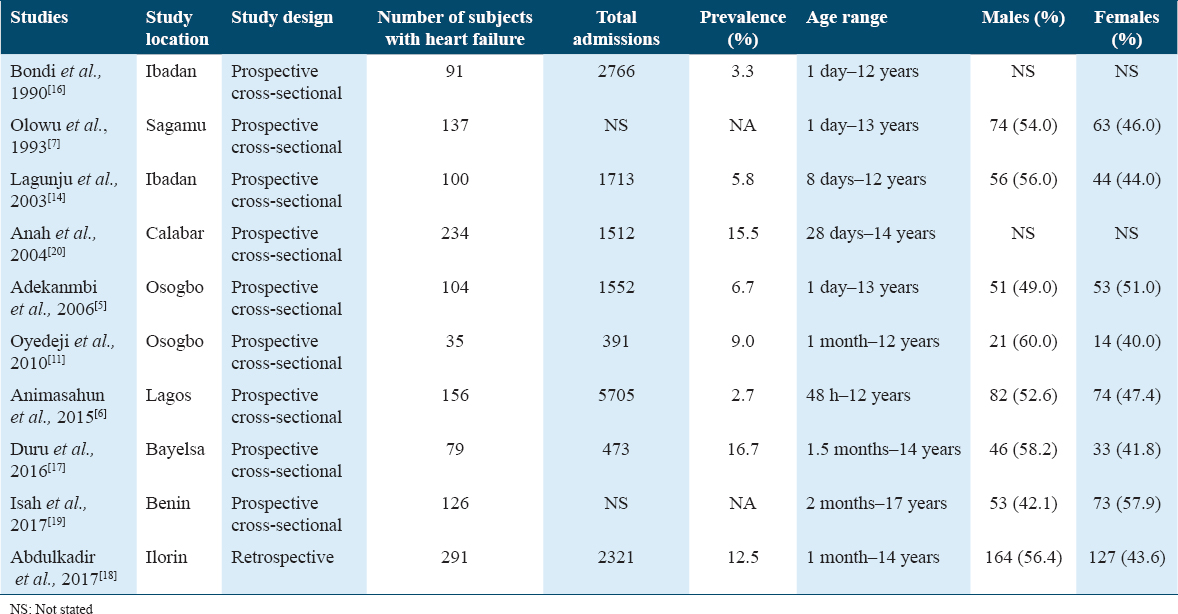
The studies had a combined population of 1119 children with heart failure. The geographic spread of the studies in Nigeria is depicted in Figure 2 with the majority of the reviewed studies conducted in the Southwest geopolitical zone of Nigeria.
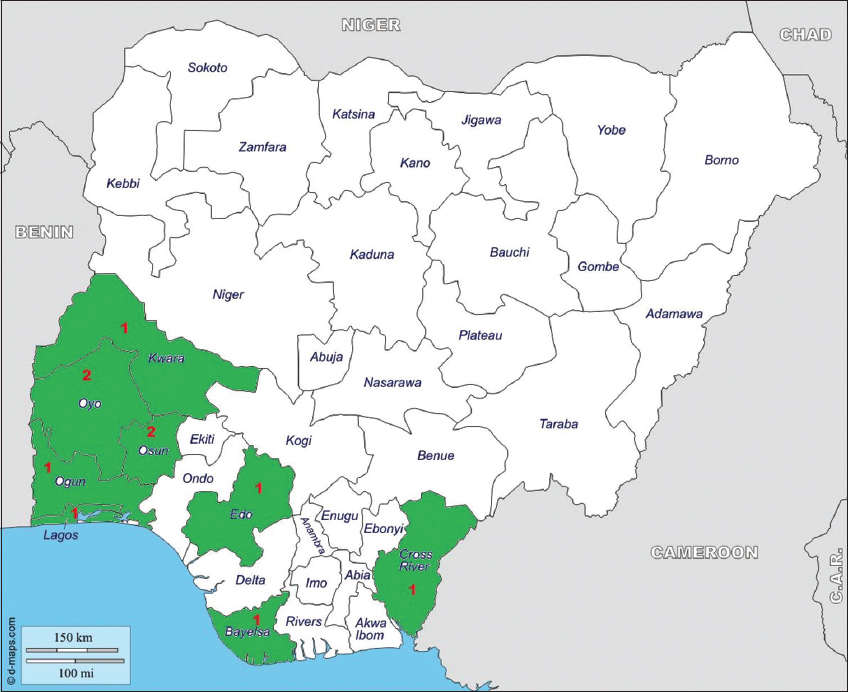
- States in which studies in review were conducted (colored) including number of studies
Burden of pediatric heart failure
Eight of the 10 studies reported data on the burden of heart failure among pediatric admissions. The incidence of heart failure ranged from a low of 2.7/100 admissions in Ibadan, Southwest Nigeria (2015) to a high of 16.7/100 admissions reported by Duru et al.[17] in Okolobiri, South-South Nigeria. Five studies reported the mean age of the children with all between 2 and 3 years of age. There was a slight male predominance in most of the studies, except the studies by Adekanmbi et al.[5] and Isah et al.[19] who reported a marginal female predominance [Table 1]. As heterogeneity across the various studies was quite substantial (I2 = 98.4, P < 0.001), we used a random effect model in determining overall prevalence. The prevalence of heart failure in the 14,921 children aged <14 years (inclusive of neonates) was 8.3% (95% CI: 4.9–12.6) using the random effects model [Table 2]. The derived scatterplot is shown in Figure 3.
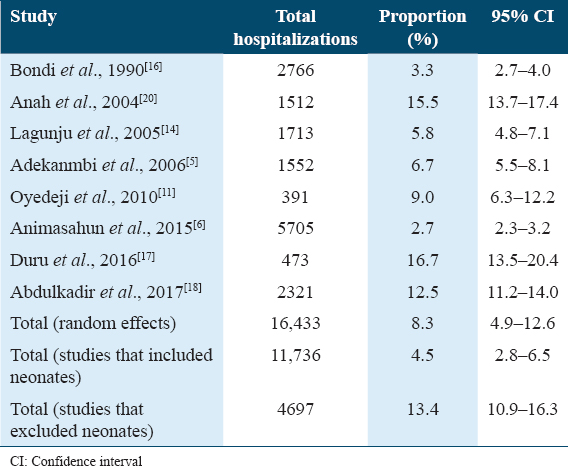
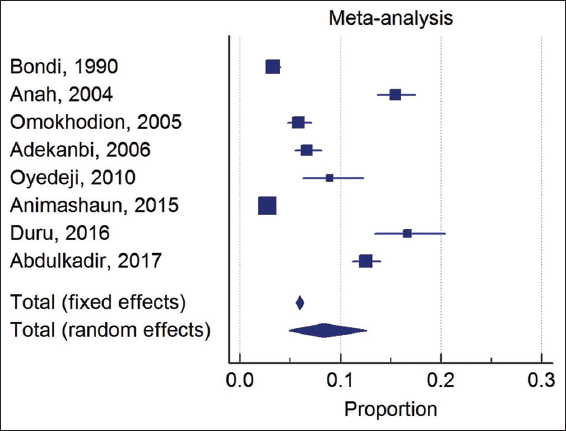
- Forest plot of proportion of children hospitalized that had heart failure across all studies
Further analysis was conducted by separating studies based on inclusion (Bondi et al., Lagunju et al., Adekanmbi et al., and Animasahun et al.)[5,6,14,16] and exclusion (Anah et al., Oyedeji et al., Duru et al., and Abdulkadir et al.)[11,17,18,20] of neonates in the study population. Heterogeneity was reduced in the children aged from above 1 month to 14 years (excluding neonates) with I2 = 83.0 (P = 0.003) [Table 2]. Using a random effect model, the prevalence of heart failure in this group of children (3185 children across the included studies) was 13.4% (95% CI: 10.9–6.3). For studies that included neonates in which there were 11,736 children admitted, substantial heterogeneity still existed (I2 = 95.4, P < 0.001) and using a random effect model, the prevalence of heart failure was 4.5% (95% CI: 2.8–6.5) [Table 2].
Etiology of heart failure
Severe anemia was the leading cause of heart failure in most of the studies reviewed [Table 3]. Lagunju et al.,[14] Animasahun et al.,[6] Bondi et al.,[16] and Olowu et al.[7] all from Southwest Nigeria reported respiratory tract infections (RTIs) as the predominant cause of heart failure [Table 4]. Severe anemia was responsible for heart failure in between 26.4% and 73.1% of subjects in the individual studies, while the contribution to burden of heart failure by RTI in the studies reviewed ranged from a low of 17.5% (Anah et al.)[20] to a high of 41.4% (Isah et al.).[19] Of the cardiac causes, ventricular septal defect was the single most frequent congenital heart disease causing heart failure, while rheumatic heart disease was the most common acquired heart disease causing heart failure [Table 3].

Overall severe anemia was the most common cause of heart failure in the meta-analyses being responsible for 38.9% (95% CI: 30.0–49.4) followed by respiratory tract infections (32.4%, 95% CI: 25.5–39.7). Others are shown in Table 4.
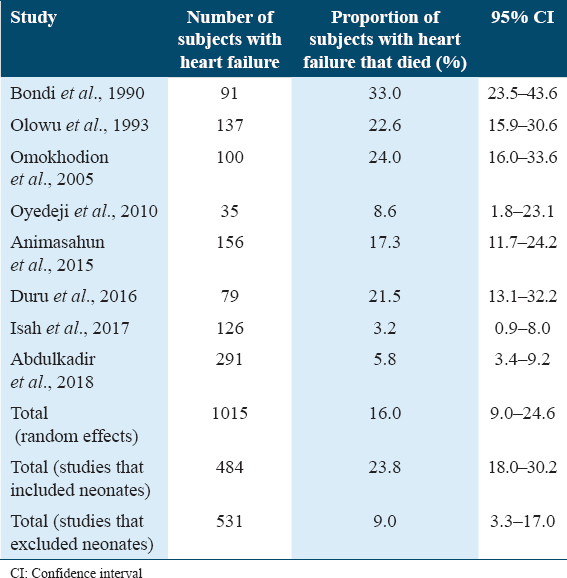
Mortality rate of subjects with heart failure
Of the studies reviewed, eight examined mortality in pediatric heart failure. Overall case fatality rates among children with heart failure ranged from a low of 3.2% reported by Isah et al.[19] (2017) in Benin to a high of 33.0% reported by Bondi et al.[16] in 1990. Others are shown in Table 5.
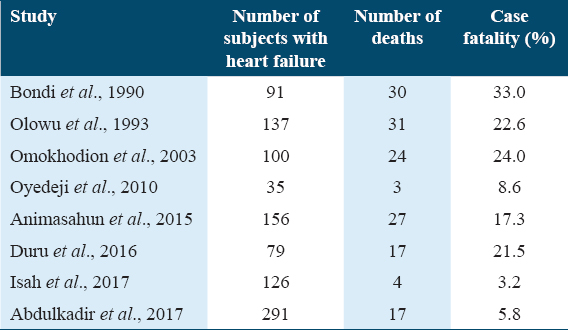
Meta-analysis was conducted using the eight studies that reported mortality data on the fatality rate attributable to heart failure among the children admitted. Merging the data across the eight studies, there were 153 deaths reported among the 1015 children with heart failure. There was significant heterogeneity in the heart failure mortality data across the studies with I2 = 91.3, p < 0.001, thus, a random effects model was used in determining case fatality rates. Fatality rate across the studies from the meta-analysis was 16.0% (95% CI: 9.0–24.6) [Table 6]. The studies were further subdivided based on inclusion of neonates with four studies including neonates. The four studies (Bondi et al., Omokhodion et al., Olowu et al., and Animasahun et al.)[6,7,15,16] that included neonates reported data on 484 children with heart failure. Heterogeneity was reduced, albeit significant, in this subgroup with I2 = 61.3, P = 0.052, thus, random effects model was used to estimate the effect size. Fatality rate for heart failure was 23.8% (95% CI: 18.0–30.2) [Table 6]. Fatality rate for heart failure in studies that excluded neonates (Isah et al., Oyedeji et al., Duru et al., and Abdulkadir et al.)[11,17-19] was 9.0% (95% CI: 3.3–17.0) [Table 6].
Discussion
This is the first systematic review and meta-analysis on burden, etiology, and fatality rates of childhood heart failure in Nigerian children. Data on heart failure in Nigeria are largely limited to small studies from a few tertiary hospitals. At present, no national database for childhood heart failure exists, though a few registries for pediatric cardiac disease are being developed.
The burden of heart failure in this review clearly varies depending on the population studied. Studies that include neonates generally had a lower proportion of admitted children having heart failure. The overall burden of 75/1000 pediatric hospital admissions is quite large when compared with other studies outside Nigeria. Ogengo et al.[21] in Kenya in 2013 reported heart failure as being present in about 1/1000 children admitted in a busy tertiary hospital. Defining epidemiology of heart failure in children in Nigeria is challenging as population-based studies are difficult to conduct considering the cost, lack of facilities, and specialized manpower. Hospital-based studies as a source of epidemiologic data, while easier to conduct, are fraught with many confounders such as hospital size, location, type of care, diagnostic criteria, and profile of causes.[3,21,22] Furthermore, difficulties in defining population of “catchment area” for hospitals make it difficult generalizing findings to the population. Nevertheless, this type of data helps health institutions plan allocation for resources in impacting maximally of relevant health conditions.[22]
The etiology of pediatric heart failure is vast consisting of cardiac (congenital and acquired) and non-cardiac causes. While congenital heart disease and cardiomyopathies predominate as causes of heart failure in developed countries, most studies in the developing tropical countries have identified non-cardiac causes such as severe anemia, respiratory tract infections, and rheumatic heart disease as the most common causes.[2,5-7,10,11,14-19,21] This study identified the “high-output” cardiac failure associated with severe anemia as the most common form in Nigerian children. Anemia causes heart failure by a complex series of mechanisms involving reduced tissue oxygenation, acidosis, systemic vasodilatation, increased salt and water retention, tachycardia, and pulmonary edema.[1,23] Rapid drops in hemoglobin will quickly lead to cardiac decompensation.[1] While, generally considered an uncommon cause of heart failure in the developed world, conditions such as severe malaria, sepsis, iron deficiency, and sickle cell anemia make it fairly common in Nigeria, and other countries in sub-Saharan Africa.[5,14,18,21]
Respiratory tract infections were the second most common cause of heart failure in this meta-analysis. Ogengo in Kenya reported a similar finding where infections (particularly respiratory infections) were the commonest cause of heart failure.[21] Heart failure in pneumonia appears to arise from a multitude of factors. Factors implicated include hypoxia, pulmonary hypertension, myocarditis, release of myocardial depressant factor from the lungs, altered heart-lung mechanics, and changes in systemic vascular resistance.[24-26]
Congenital heart disease was responsible for between 6.8% and 10.2% of all heart failure in this review, with the most common being ventricular septal defects. This is similar to the findings by Ogengo et al. in a study in a tertiary hospital that reported congenital heart disease being responsible for 13.3% of heart failure cases.[21] This is in contrast to the United States of America where a large database review reported that congenital heart disease accounted for 62% of heart failure cases among infants.[27] Similarly, in Europe, slightly more than half of the pediatric heart failure cases were due to congenital heart disease.[3,4] Amoah and Kallen in Ghana reported that about two-fifths of heart failure cases among children were caused by congenital heart disease in a study conducted a cardiac surgical referral hospital.[28] These differences highlight the challenge in describing the contributions to etiology of heart failure as it varies with location, population studied, and type of hospital, among many other variables.
Similar to adult studies, the presence of heart failure in children has been associated with increased risk of mortality.[11,17,29,30] Fatality rates in this review ranged between 3.2% and 33% in Nigeria over the review period. Overall, mortality rates were between 9.0 and 24.6% and fatality rates were higher in studies that excluded neonates compared to those with neonates included. This is slightly higher than 7.7% reported by Ogengo et al. in Kenya.[21] Rossano et al. in a large retrospective review described a lower mortality rate of 7.4% among over 49,000 children <18 years admitted that had heart failure related hospitalizations.[29] The mortality rate from this review is undoubtedly alarming, considering that most of these deaths in this review resulted from readily preventable and treatable conditions such as severe anemia (from malaria and sepsis) and respiratory tract infections, in contrast to the USA study by Rossano et al.[29] and the European study by Massin et al.[3] where majority of the deaths resulted from difficult to treat/untreatable conditions, such as complex congenital heart disease, acute renal failure, arrhythmias, pulmonary hypertension, and cardiomyopathies. Thus, we postulate that weak health systems in Nigeria, poor care seeking behavior, large burden of infectious diseases, and lack of manpower may be contributory to the poorer survival of children with heart failure in Nigeria.
Limitations
Studies in the review were all conducted in tertiary hospitals and, as such, the review may suffer from bias of including very ill children who are likely to be referred to these institutions. A lack of population-based studies limits the generalizability of the findings reported in this review to the general population. Furthermore, the studies were mostly from South Nigeria with only one study from the north, which has been shown to differ considerably in climate, culture, social status, and care-seeking behavior. Nevertheless, the two studies from North Nigeria were fairly large and may have minimized the effect of this potential bias.
Conclusion
This review has documented a nationwide view of the burden of heart failure as seen in children in health facilities in Nigeria and has identified primarily non-cardiac problems of severe anemia and respiratory tract infections as the leading contributors to heart failure in Nigeria. Furthermore, mortality from heart failure in children is remarkably high, particularly considering the causes of death in these children who are largely preventable and readily treatable conditions.
Acknowledgment
The authors do acknowledge the researchers in Nigeria that generated the data that formed the source for this review. We acknowledge the support of the Cardiovascular Research Training (CaRT) Institute program of New York University/University of Ghana School of public health (NIH/Fogarty International Centre funded program; Grant number - 5D43TW009140-05) and Prof Charles Agyemang for the training given to MBA on writing systematic reviews.
Funding and Support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ Contributions
All authors have qualified to be authors by their contributions to the manuscript. MBA, RMI, and AI conceptualized the study. BMA and RMI conducted the systematic search. All authors participated in the execution of the study. MBA, RMI, AI, HDS, BO, and KA performed the data analysis and interpretation of the data. All authors participated in the preparation of the manuscript. The correspondence author did the final draft of this paper. All authors read and approved the final manuscript and agree to take responsibility for the contents of this paper.
References
- Heart failure. In: Kliegman RM, Stanton BF, St-Geme J, Schor N, Behrman RE, eds. Nelson Textbook of Pediatrics (20th ed). Philadelphia, PA: Elsevier/Saunders; 2016. p. :2282-8.
- [Google Scholar]
- Heart failure in children:Part I:History, etiology, and pathophysiology. Circ Heart Fail. 2009;2:63-70.
- [Google Scholar]
- Epidemiology of heart failure in a tertiary pediatric center. Clin Cardiol. 2008;31:388-91.
- [Google Scholar]
- Congestive heart failure in childhood. An epidemiologic study. Herz. 2005;30:652-62.
- [Google Scholar]
- Current trends in the prevalence and aetiology of childhood congestive cardiac failure in Sagamu. J Trop Pediatr. 2007;53:103-6.
- [Google Scholar]
- Congestive cardiac failure among Nigerian children;Pattern and outcome. Int Cardiovasc Res J. 2015;9:164-8.
- [Google Scholar]
- Etiological peculiarities in pediatric heart failure. Maedica (Bucur). 2015;10:371-5.
- [Google Scholar]
- Etiological spectrum of heart failure in pediatric population. Indian J Pediatr. 2015;82:482.
- [Google Scholar]
- The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377-84.
- [Google Scholar]
- Systematic literature review on the incidence and prevalence of heart failure in children and adolescents. Pediatr Cardiol. 2018;39:415-36.
- [Google Scholar]
- Pediatric heart failure among emergency room admissions in a Tertiary health centre in Southern Nigeria. Niger J Cardiol. 2016;13:62-6.
- [Google Scholar]
- Aetiology and outcome of childhood heart failure in an emergency paediatric unit in North Central Nigeria. Port Harcourt Med J. 2017;11:161-5.
- [Google Scholar]
- Usefulness of amino terminal pro-B-type natriuretic peptide in evaluating children with cardiac failure. Cardiovasc Diagn Ther. 2017;7:380-8.
- [Google Scholar]
- Heart Failure among paediatric emergencies in Calabar, South Eastern Nigeria. Mary Slessor J Med. 2004;4:58-62.
- [Google Scholar]
- Pattern of congestive heart failure in a Kenyan paediatric population. Cardiovasc J Afr. 2013;24:117-20.
- [Google Scholar]
- Potential uses and limitations of hospital data in epidemiologic research. Am J Public Health Nations Health. 1965;55:658-67.
- [Google Scholar]
- Pneumonia complicated by congestive heart failure in Nigerian children. East Afr Med J. 2012;89:322-6.
- [Google Scholar]
- Role of brain natriuretic peptide assay in identifying children with pneumonia complicated by congestive cardiac failure. Ann Health Res. 2018;4:182-8.
- [Google Scholar]
- Comparison of the epidemiology and co-morbidities of heart failure in the pediatric and adult populations:A retrospective, cross-sectional study. BMC Cardiovasc Disord. 2006;6:23.
- [Google Scholar]
- Aetiology of heart failure as seen from a national cardiac referral centre in Africa. Cardiology. 2000;93:11-8.
- [Google Scholar]
- Prevalence, morbidity, and mortality of heart failure-related hospitalizations in children in the United States:A population-based study. J Card Fail. 2012;18:459-70.
- [Google Scholar]







