Translate this page into:
Management of axillary hidradenitis suppurativa: A case report
Address for correspondence: Dr. Saad M. Alqahtani, Department of Surgery, College of Medicine, Majmaah University, Al-Majmaah 11952, Saudi Arabia. E-mail: sm.alqahtani@mu.edu.sa
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Hidradenitis suppurativa is a rare, chronic, and recurrent skin disease that affects the pilosebaceous-apocrine unit. Its diagnosis is challenging and it usually manifests in advanced stages due to a lack of knowledge about this entity. To date, there are no standardized therapeutic protocols available for its management. We present a case of a 22-year-old woman with the left axillary hidradenitis suppurativa and underwent surgical treatment successfully. This report emphasizes the importance of educational programs among primary care professionals and public awareness campaigns about this disease, which is under-reported in our community, to avoid physical and psychological complications.
Keywords
Acne inversa
hidradenitis suppurativa
primary health-care center
Saudi Arabia
Introduction
Hidradenitis suppurativa (HS), also called acne inversa, is a chronic inflammatory skin condition with an estimated prevalence of 0.00033–4.10%.[1] HS is diagnosed based on three clinical criteria — distinctive lesions, a propensity for development in flexural sites, and recurrence. The lesions develop as non-inflamed lesions, progressing to deep-seated painful nodules with abscesses, sinus tracts, fistulae, or scars.[1]
HS typically manifests after puberty and is usually present at the axillary, inguinal, perineal, and submammary areas. It has also been documented to occur on the buttocks, back, mons pubis, postauricular region, and scalp.[1]
The pathogenesis of HS is not fully understood; however, the disease is thought to be initiated by follicular hyperkeratosis, followed by dilatation, follicular rupture, and inflammation. Tumor necrosis factor alpha (TNF-a) and interleukin-17 (IL-17) cytokines, and genetic predisposition also play a role in its pathogenesis.[1] HS has been thought to be characterized by autosomal dominant inheritance. Furthermore, a link has been discovered between a subset of HS and g-secretase complex gene mutations.[2] The effect of sex hormones on the pathogenesis of HS remains unclear. HS is also believed to have a distinct skin microbiome. However, the role of microbiome dysbiosis in HS remains an area that is actively researched.[1,3]
HS is a debilitating disease that negatively affects the patient’s quality of life, both socially and psychologically. Longstanding HS can lead to fibrosis, scarring, contractures, lymphatic obstruction, and in rare cases, squamous cell carcinoma.[4]
Several skin diseases, such as inflamed epidermoid cysts, bacterial folliculitis, and furunculosis, can mimic HS. However, HS is diagnosed and treated over a longer period, as it often presents with characteristic recurrence.[2]
The diagnosis of HS is challenging and it presents with a variety of clinical manifestations. Therefore, the establishment of a one-size-fits-all therapeutic algorithm or protocol is impractical. In addition, HS requires a multidisciplinary team approach to tailor appropriate management.[4,5] The present case involved a 22-year-old woman with delayed presentation of the left axillary HS who successfully underwent surgical management.
Case Presentation
A 22-year-old non-smoking woman presented to the surgical clinic with a 1-year history of intermittent discharge from a left axillary wound. The patient’s medical, surgical, and family histories were unremarkable. She reported that the wound exhibited intermittent discharge that had turbid appearance was mixed with bloody material and was triggered by menstruation. The patient had a long history of deodorant use. Initially, the patient was referred to a primary health-care center (PHCC) and was prescribed different courses of antibiotics including amoxicillin + clavulanate; however, she did not show signs of improvement. She had normal vital signs and a body mass index of 20 kg/m2. Local examination revealed a small, superficial wound with a sinus in the left axilla [Figure 1] along with numerous palpable axillary lymph nodes. Based on the clinical findings, a diagnosis of HS (stage II) was established.

- Stage II axillary hidradenitis suppurativa
Ultrasonography revealed a 4 × 2 mm superficial collection near the left axilla. Furthermore, two left axillary lymph nodes with normal echotexture and preserved hilum were observed, measuring 2 × 0.7 and 1.3 × 0.4 cm, respectively.
A swab was obtained from the wound discharge and the results revealed the presence of Staphylococcus aureus. Accordingly, ciprofloxacin was prescribed based on culture and sensitivity results. At follow-up, there was no improvement and surgical intervention was planned. During the procedure, an elliptical incision was made, followed by complete excision of the affected area and then primary closure. We opted for this procedure because of the limited area involved. On day 1 following surgery, the patient was discharged with a 1-week course of oral ciprofloxacin. The final histopathological results confirmed the diagnosis of HS. The patient underwent follow-up for 1 year with no recurrence [Figure 2].

- The affected area following surgery
Discussion
HS is a chronic and recurrent skin disease of unknown etiology, which can result in depression and social isolation in extreme cases. It is more common at the age of 20–30 years, with a female predilection,[4] which is consistent with our patient.
Coexisting morbidities (e.g., diabetes mellitus, metabolic syndromes, cardiovascular disease, hypertension, hypertriglyceridemia, obesity, depression, Crohn’s disease, psoriasis, and spondyloarthropathy), lifestyle habits (e.g., smoking), and family history are all well-known factors associated with HS.[1] However, none of these factors were identified in the present case. Stress, menstruation, excessive sweating, and weight gain are documented triggers of HS.[1] Our patient’s condition was exacerbated by stress and menstruation.
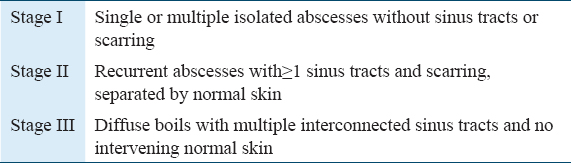
There are various systems used for the classification of HS. The Hurley staging system is one of them and it categorizes HS into three clinical stages [Table 1].[1] Our patient was diagnosed as Stage II, which is characterized by recurrent abscesses with one or more sinus tracts and scarring separated by normal skin.
HS is usually diagnosed clinically, and to date, no specific investigation has been established that would aid in rapid and non-invasive diagnosis of HS. Hence, a high degree of clinical suspicion is required. In our study, the patient was misdiagnosed for over a year. Shirah et al. reported that 50% of patients in their study were misdiagnosed for a long time. In addition, they were treated only by health-care practitioners and not referred to the appropriate specialty.[4] Kim et al. reported 80 patients with HS, of whom 71% were diagnosed more than 1 year after disease onset.[6] Meanwhile, board-certified family physicians possess more knowledge about HS than general practitioners at PHCCs.[7] Overall, these findings highlight the necessity of cultivating adequate and comprehensive knowledge of HS, particularly at the PHCC level. In addition, it emphasizes the importance of awareness program in the Saudi community. This will allow for early diagnosis and prompt referral to an appropriate specialty thereby minimizing morbidity.
Numerous therapeutic options, both medical and surgical, have been used for HS because of variations in disease presentation, chronicity, and severity. Furthermore, the patient’s preferences and impact of prior treatments must be considered when selecting a treatment plan.[8]
In general, conservative treatment is effective in early-stage disease, whereas surgery is advised in the presence of abscesses, fistulae, sinus tracts, or scars.[2] In addition, surgical intervention is recommended in unresponsive cases.[2] Certain lifestyle changes, such as smoking cessation and weight loss, have the potential to be beneficial in the management of HS. In addition, avoiding stress, heat, excessive sweating, tight clothing, and deodorants are helpful.[8] Medical treatment includes topical and systemic antibiotics, oral glucocorticoids, isotretinoin, infliximab, and cyclosporine.[8-10]
Due to advances in the understanding of the pathogenesis of HS, adalimumab, a TNF inhibitor, has recently been discovered as an effective biological agent in the treatment of HS. Furthermore, newer biological agents that target multiple cytokines are also currently undergoing clinical trials.[10]
However, surgery remains an excellent option for the local control of HS. Different surgical techniques, such as deroofing, incision and drainage, wide radical excision with primary closure, secondary intention healing, skin grafts, or flaps are used. The last two techniques are recommended for larger wounds and in complicated, severe disease[8,10,11] Other modalities, such as hormonal agents, lasers, and radiotherapy are also used.[10,12]
The use of wide excision with primary closure is controversial. Favorable outcomes have been reported with primary closure,[5,9] similar to our case. However, others argue that this strategy should be avoided because of high recurrence rates.[9] According to a recent study, there is no agreement on the best wound closure technique in such cases.[13]
Notably, wide excision with secondary intention healing is associated with low recurrence rates.[9] Ather et al. reported three cases of HS that failed to respond to conservative treatment. Subsequently, the patients underwent a surgical intervention. The authors recommended wide local excision with secondary intention healing as the optimal technique in most cases.[8]
Following wide excision, the use of biological agents such as infliximab has been shown to minimize the recurrence rate of HS. It also improved the disease-free interval in such patients.[13]
There are few reports of HS from Saudi Arabia.[4,7,14,15] In 2017, Shirah et al. reported 627 patients with HS who were treated with fusidic acid with promising results.[14] A retrospective cohort study involving 1369 patients with HS was conducted by the same authors. The vast majority (n = 974, 71.1%) were treated conservatively, with a recurrence rate of 12.5% (122 patients). The remaining patients were treated surgically (n = 395, 28.9%). Among the 395 patients treated surgically, 281 (71.1%) underwent complete excision, while 114 (28.9%) underwent incision and drainage. There were no recurrences associated with either technique.[4] Eleven patients with Down syndrome and HS were enrolled in a local observational study. Eight patients with axillary HS (six with Stage I and two with Stage II) were treated conservatively.[15] Finally, our case enriches current literature by adding a datapoint to the treatment of Stage II HS.
Conclusion
Since HS is a challenging disease to diagnose, with the risk of complications, well-established educational programs are essential at the level of PHCCs to refer patients promptly to the relevant specialists. Misdiagnosis can result in psychological, cosmetic, and physical consequences. We advocate for a larger case series in this avenue, comparing different treatments and outcomes in HS. In addition, a closer examination of the inadequacies of PHCCs in the diagnosis of HS and the formulation of detailed solutions that address these lacunae would also greatly aid in the future treatment of HS.
Author’s Declaration Statement
Declaration of patient consent
Written consent was taken from the presented patient.
Data availability statement
All data are available in the manuscript.
Conflicts of interest
The author reports no conflicts of interest.
Source of funding
None.
Ethical approval
Not applicable.
Acknowledgment
We would like to acknowledge the valuable input of Dr.Yousef Alalawi in reviewing this manuscript. Also, we would like to thank Deanship of Scientific Research at Majmaah University for supporting this work under Project Number R-2022-147.
References
- Hidradenitis suppurativa:Epidemiology, clinical presentation, and pathogenesis. J Am Acad Dermatol. 2020;82:1045-58.
- [Google Scholar]
- Hidradenitis suppurativa:A systematic review and meta-analysis of therapeutic interventions. Indian J Dermatol Venereol Leprol. 2019;85:248-57.
- [Google Scholar]
- Hidradenitis suppurativa:An update on epidemiology, phenotypes, diagnosis, pathogenesis, comorbidities and quality of life. J Eur Acad Dermatol Venereol. 2021;35:50-61.
- [Google Scholar]
- The clinical pattern of axillary hidradenitis suppurativa among Saudi Arabians:Mode of presentation and treatment challenges. J Cutan Aesthet Surg. 2017;10:95-100.
- [Google Scholar]
- Hidradenitis suppurative:Our experience with a surgical case management team. Actas Dermosifiliogr (Engl Ed). 2020;111:408-12.
- [Google Scholar]
- Clinical features and patient outcomes of hidradenitis suppurativa:A cross-sectional retrospective study. J Cutan Med Surg. 2016;20:52-7.
- [Google Scholar]
- Knowledge about and determinants for diagnosing hidradenitis suppurativa by ministry of health primary healthcare physicians in Jeddah city 2019:An analytical cross-sectional study. J Family Med Prim Care. 2020;9:1448-52.
- [Google Scholar]
- Surgical treatment of hidradenitis suppurativa:Case series and review of the literature. Int Wound J. 2006;3:159-69.
- [Google Scholar]
- Hidradenitis suppurativa:Surgical and other management techniques. Dermatol Surg. 2012;38:517-36.
- [Google Scholar]
- Hidradenitis suppurativa:Current and emerging treatments. J Am Acad Dermatol. 2020;82:1061-82.
- [Google Scholar]
- Current and future treatment of hidradenitis suppurativa. Br J Dermatol. 2020;183:e178-87.
- [Google Scholar]
- North American clinical management guidelines for hidradenitis suppurativa:A publication from the United States and Canadian hidradenitis suppurativa foundations:Part I:Diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81:76-90.
- [Google Scholar]
- Integrated multidisciplinary approach to hidradenitis suppurativa in clinical practice. Int J Womens Dermatol. 2020;6:164-8.
- [Google Scholar]
- Effective modified conservative tissue preserving protocol to treat Stage I axillary hidradenitis suppurativa:A prospective cohort study of 627 patients with five years follow-up. J Dermatolog Treat. 2017;28:458-63.
- [Google Scholar]
- Hidradenitis suppurativa in down syndrome:A case series. Pediatr Dermatol. 2017;34:461-4.
- [Google Scholar]







