Translate this page into:
Assessment of diastasis recti abdominis: Clinimetric properties of four measuring instruments
Address for correspondence: Ezeigwe Anne Uruchi, Department of Physiotherapy, Enugu State University Teaching Hospital, Parklane, Enugu State, Nigeria. Phone: +2348097740032. E-mail: auezeigwe@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
ABSTRACT
Objective:
The aim of the study was to determine the intra- and inter-rater reliability of palpation technique, digital calipers, and diastometer, as well as their concurrent validity against ultrasound imaging.
Methods:
Ninety consenting parous women (20–45 years), recruited from a postnatal clinic in Enugu, Nigeria, participated in this observational study. Two physiotherapists and a sonographer measured their inter rectus distance at the level of the umbilicus, 4.5 cm above and below it, respectively, using each of the four modalities. The intra-rater measurements were taken at a week’s interval. Data were analyzed with descriptive and inferential statistics of intraclass correlation coefficient and paired samples T-test, at an alpha level set at P < 0.05.
Results:
It showed the palpation technique (r = 0.749–0.967 and 0.658–0.917), digital calipers (r=0.750–0.955 and 0.685–0.904), and diastometer (r=0.762–0.958 and 0.471–0.902) demonstrated good inter- and intra-rater reliability. The concurrent validity of the palpation technique, digital calipers, and diastometer against the USI was poor at all three reference points.
Conclusion:
Palpation technique, digital calipers, and diastometer are reliable tools but not valid substitutes to ultrasound imaging for the clinical measurement of diastasis rectus abdominis.
Keywords
Diastometer
digital calipers
inter-rectus distance
palpation
ultrasound imaging
Introduction
Significant anatomical and physiological changes occur during pregnancy which enables the woman to accommodate, nourish, and cater for the growing fetus. These changes which are hormone mediated, together with sustained increase in intra-abdominal pressure from the growing fetus, facilitate the stretching and flaccidity of the linea alba-a tendinous raphe between the paired rectus abdominis muscles in the anterior abdominal walls causing elongation of the muscles with resultant increase in the distance between its medial borders.[1] The distance between the paired rectus abdominis muscle is referred to as inter-rectus distance (IRD), while an increased IRD, due to abnormally excessive separation between both components of the muscle along the linea alba, is termed diastasis recti abdominis (DRA), rectus abdominis diastasis, or divarication of rectus abdominis muscles.[2,3]
The most common anatomical location for DRA in females is at the level of the umbilicus, although it may extend to the supra/infra-umbilical regions,[4] involving different sites along the linea alba.[4-7]
Several treatment options are available for the management of DRA but physiotherapy has been the most widely utilized conservative measure of DRA management with its effectiveness reported in several studies.[8-12] To facilitate physiotherapeutic intervention, successful diagnosis, and evaluation of outcome measures are dependent on the use of valid and reliable assessment techniques. Therefore, sound clinimetric properties are necessary pre-requisite for the choice of measuring instruments. Available methods for measuring DRA in Physiotherapy and in most health-care practices include the use of calipers, tape measure, computed tomography, magnetic resonance, ultrasound, and the traditional finger width (palpation) method.[4,8,13-21]
These measurement methods are used cross-culturally with each possessing its benefits and limitations. The gold standard instrument for the measurement of IRD is the conventional ultrasound imaging (USI), because it compares favorably to intraoperative surgical compass measurements,[22] while producing consistent results between days.[23] Moreover, it provides a measure of IRD on a continuous scale, increasing its responsiveness. However, its cost is astronomical and requires extensive examiner training and clinical mastery.[24] Furthermore, its availability and accessibility to physiotherapists in developing countries are not guaranteed.
Palpation method, the predominantly used measure in clinical diagnosis,[25] involves the use of fingers to feel the medial borders of the rectus abdominis muscles. Diagnosis is made based on the number of fingers that fit between the medial borders of the rectus abdominis muscles. However, there are no standard guidelines on the positioning of the palpating fingers relative to its distance from the umbilicus as well as the starting position of the client. Nevertheless, this technique is easy to carry out and requires no specialist training. The digital calipers involve placing the inside measurement jaws where the palpating fingers are located at the medial borders of both rectus abdominis muscle bellies, with the values read from the screen. This instrument has the advantage of clarity because of the liquid crystal display screen and has no need for recalibration. However, its utilization of alkaline cell batteries may be an encumbrance, as well as its sensitivity to weather changes.
The most recent innovation for IRD measurement is the diastometer, invented in 2015 by Tupler.[26] It has two components, a distance-measuring component adapted to measure the DRA distance and a depth-measuring component adapted to measure the depth of DRA. Measurement is done by wearing this device as a belt around the abdomen, ensuring that the reference point, a red dot positioned at the center of the measuring strip aligns with the umbilicus. The values are obtained by sliding the indicator loops into the position, marked by the palpating fingers, and are read off from the location of the indication loops with respect to the indicia on the tape.[26] The depth of the IRD is determined by depressing the clad forefinger finger sock component gently into the abdomen with the lower measurement visible on the finger sock determining the depth. This dual property of the diastometer makes it unique among the instruments under review. Despite accreditations to its effectiveness in the assessment of DRA, there are no empirically proven documentations on its validity and reliability, relative to other standardized measurement tools. Previously, some authors have reported validity and reliability results for other measuring tools, including calipers,[17,27,28] palpation technique,[29,30] and ultrasound.[22,23,31] However, considering variations in their study designs and findings, there is still a need to further evaluate the clinimetric properties of these measurement tools, especially in a different geographical location. Furthermore, investigating each instrument’s concurrent validity against the gold standard (USI) is a surefire way of proving their clinical utility. Thus, this study is designed to determine the construct validity of the diastometer, inter- and intra-rater reliability of the diastometer, calipers, and palpation techniques as well as the concurrent validity of all three against conventional USI.
Methods
This study which utilized a methodological design, a variant of observational study designs, was carried out at the Department of Physiotherapy, Enugu State University teaching Hospital Park Lane (ESUTHP) Enugu, Nigeria. Participants included purposively selected parous women (20–45 years of age) who have experienced 1–4 childbirths and presented for postpartum checkup or routine infant immunization at the above-named hospital during the period of this study (April–July 2019). The exclusion criteria included: (1) A history of recent abdominal surgery as the scars may obscure the lines alba, (2) neck and low back pain of ≥3-month duration which may limit the appropriate performance of the testing procedures which involved a head tilt and supine lying position, respectively, and (3) pregnancy which may alter study findings due to hormonal changes.
For a significant Pearson product moment correlation at a 0.05 level of significance, a power of 0.90, and a medium effect size of 0.30, 92 participants were needed for this study.[32]
To control for subject attrition, 97 participants were recruited but only 90 successfully completed this study.
Ethical approval was obtained from both the Research Ethics Committee College of medicine, University of Nigeria, Enugu campus, and the Research, Education, and Training Committee (RET) of ESUTHP, Enugu, Nigeria. All participants gave written informed consent before participation in the study.
Study procedures
Each participant underwent IRD measurements from three different abdominal locations, using each of the study instruments (USI, palpation technique, digital calipers, and diastometer), respectively. With participants adopting a comfortable supine position on the examination couch, three reference points were measured out with a tape measure and marked with a water-soluble marker. These points include 4.5 cm above the umbilicus, at the umbilicus, and 4.5 cm below the umbilicus. These locations have previously been used to measure IRD in the previous studies.[17,33-36]
Each of the measurements was taken by two physiotherapists with 2 and 14 years of clinical experiences, respectively, except for the ultrasound measurement which was taken by a single sonographer (8 years of clinical experience). Each rater was blinded to the measurement results of the other. For the purpose of assessing the intra-rater reliability of the palpation technique, digital calipers, and diastometer measurements, each of the procedures was repeated 1 week after the initial measurement. To prevent cross-contamination of infections, the instruments and participant’s anterior abdominal wall were cleaned with cotton wool and methylated spirit pre and post each assessment.
Ultrasound measurement
Using a Toshiba Diagnostic Ultrasound with 7.5 mHz linear probe (Model UIPS-510A), the sonographer performed the USI measurements while the participant assumed a supine lying position with knees and hips flexed at 90 degrees each. The sonographer instructed them to perform a head lift which involved some degrees of trunk flexion while fixing the eyes on the umbilicus. The transducer was then placed at each marked location, the medial borders of the rectus abdominis muscles were captured and the distance between both marked using the onscreen cursor.
Palpation technique measurement
A starting position similar to the ultrasound measurement was adopted for this technique. Using the tips of the four fingers, the physiotherapist palpated the medial borders of the rectus abdominis muscles, along the linea alba. On close identification of these borders, the physiotherapist inserted her fingers (as many as could fit) between both borders to determine the IRD width. We were challenged with estimating finger breadth values in standard SI units, considering that there was a paucity of empirical data on standard finger breadth measurements of Africans. Thus, we conducted a pilot study which assessed the breath of the index and middle fingers of 50 adults (22 males, 28 females), using a flexible measuring tape. The average values were 1.4 cm and 1.6cm for the index and middle fingers, respectively. These average values were used to estimate the IRD during the palpation technique of assessment in this study.
Digital calipers measurement
The starting position was the same as for the ultrasound measurement. The rater placed the inside measurement jaws of the digital calipers (RoHS model) at the locations of the medial borders of the participant’s rectus abdominis muscles, as palpated with the fingers. The jaws were then adjusted to observe IRD width.
Diastometer measurement
Again, the starting position was the same as with all the other measurement techniques. However, the distance-measuring component of the diastometer was worn as a belt encircling each participant’s torso. The diastometer’s reference point, which is a red dot, was positioned at the center of the measuring strip in alignment with each participant’s umbilicus. The values were obtained by sliding the indicator loops into the position marked by the rater’s fingers. The value was then read of with respect to the indicia on the tape. The depth of the IRD was subsequently determined using the finger sock component of the diastometer. This was done by gently depressing the finger sock-clad forefinger into the abdomen at the various reference points. The lower measurement visible on the finger sock was the depth of the IRD at that point on the abdomen.
Data analysis
Statistical analyses were performed in SPSS for windows version 21.0. Descriptive statistics of mean and standard deviation were used to summarize data. To determine the intra and inter-rater reliability, two-way random effects models of intraclass correlations (ICC2:1 and ICC2:2) with 95% confidence interval were used. ICC scores of <0.40 were considered poor; 0.40–0.59 fair/moderate; 0.60–0.74 good, and greater than 0.75 excellent.[37]
The standard errors of measurement were calculated. The concurrent validity of the palpation technique, digital calipers, and diastometer as compared to USI was computed with two-way random effects model of intraclass correlations (ICC2:2) and statistical difference checked with paired samples t-test with statistical significance set at P<0.05.
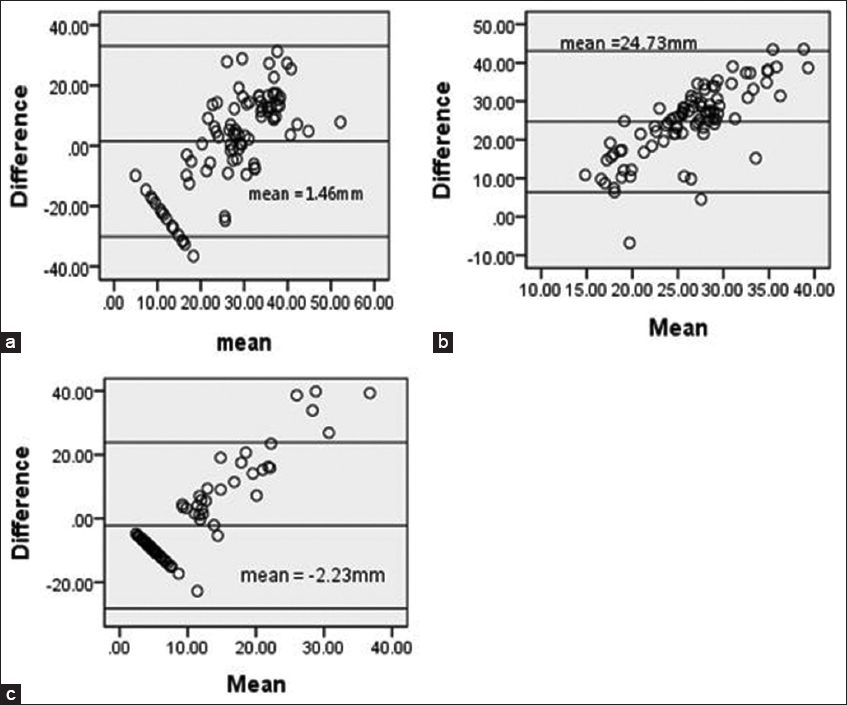
To graphically determine the degree of agreement between USI, palpation, digital calipers, and diastometer measurements of IRD, a Bland-Altman plot was constructed.
Results
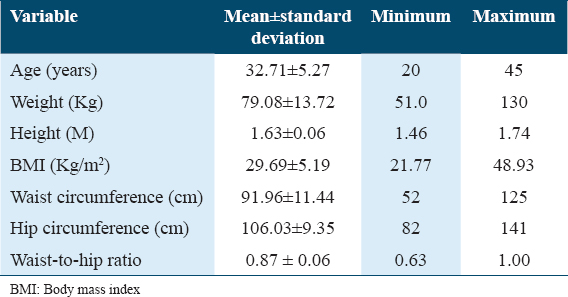
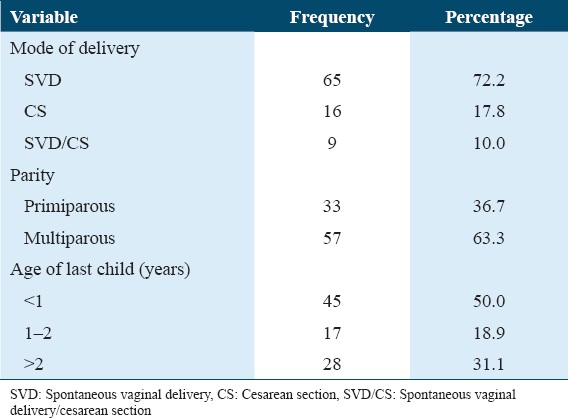
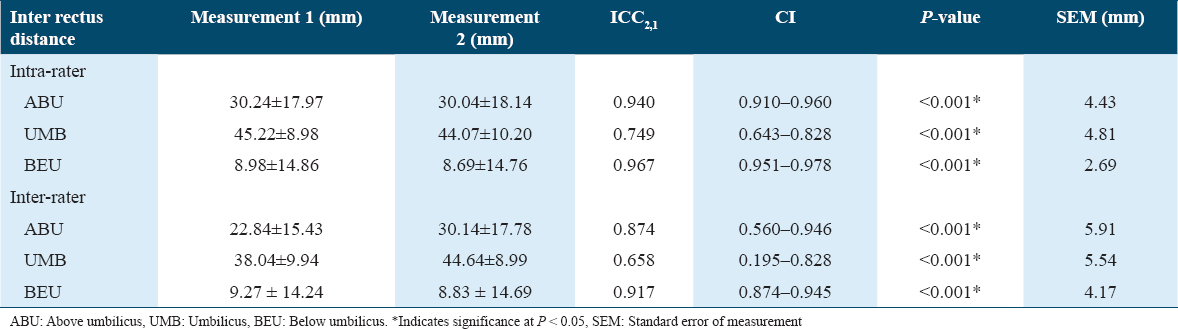
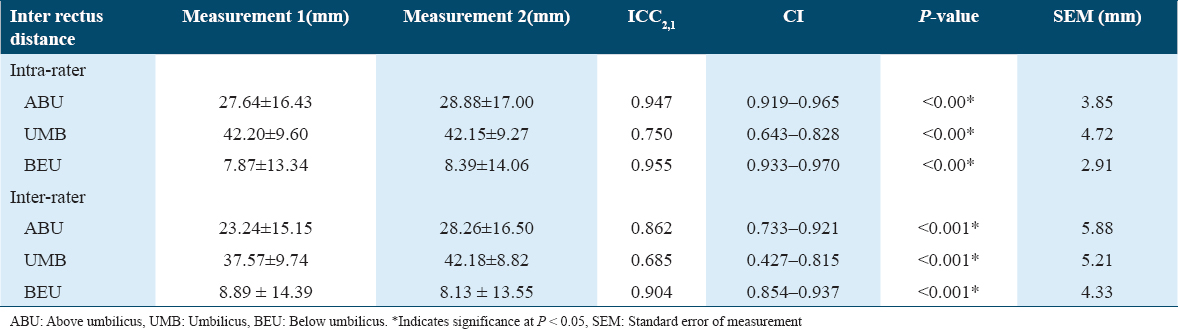
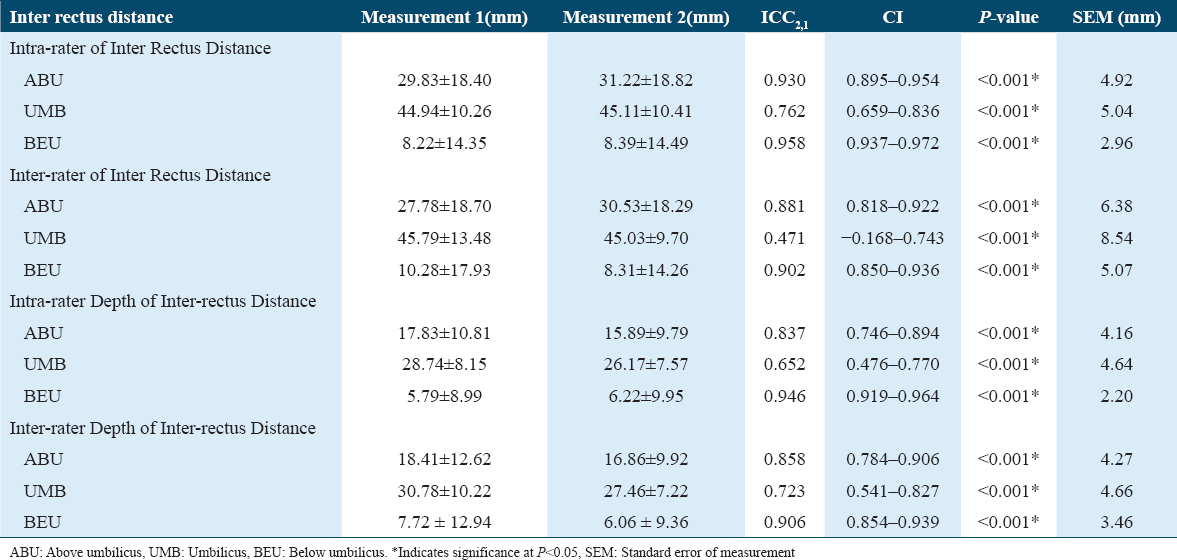
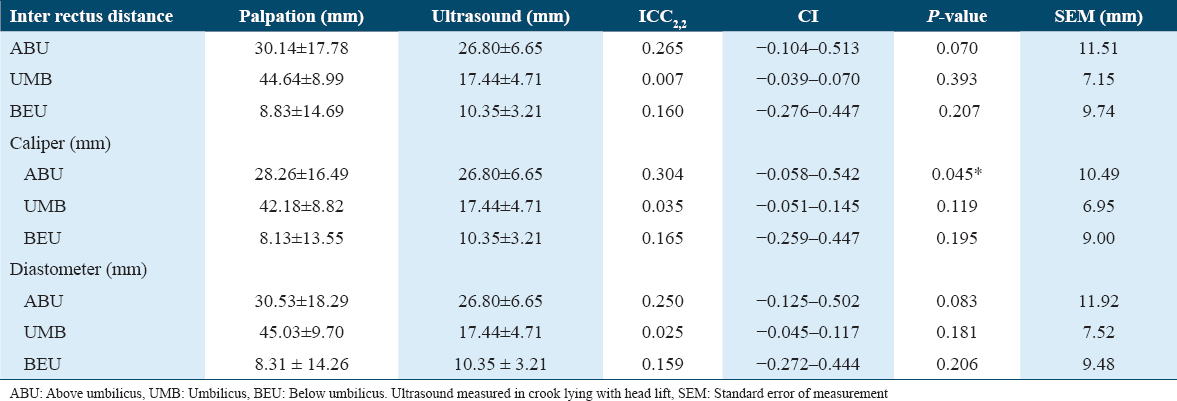
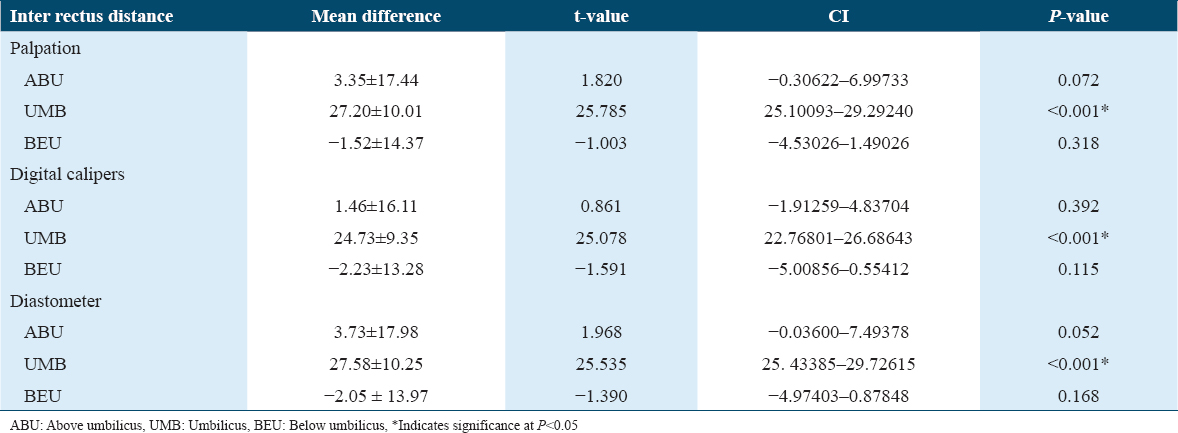
The mean age of the participants was 32.71 ± 5.27 [Table 1] while the majority of the women had spontaneous vaginal deliveries (72.2%), were multiparous (63.3%), and within <1-year postpartum duration (50%) as shown in Table 2. The intra and inter-rater reliability of palpation technique for measurement of IRD are presented in Table 3. The intra-rater reliability was excellent at the three points of measurement (ICC2.1: 0.749–0.967) while the inter-rater reliability was good at the umbilicus (ICC2.2: 0.658) and excellent above and below the umbilicus (ICC2.2: 0.874 and 0.917), respectively. The digital calipers technique for measurement of IRD has excellent intra-rater reliability at the three points of measurement (ICC2.1: 0.750–0.955). It has good (ICC 2.2: 0.685) to excellent (ICC2.2: 0.862–0.904) inter-rater reliability as shown in Table 4. The intra-rater reliability for measuring IRD with the diastometer was excellent at all three reference points (ICC2.1: 0.762–0.958), while the depth showed good (ICC2.1: 0.652) at the umbilicus but was excellent (ICC2.1: 0.837 and 0.946) above and below the umbilicus, respectively. The inter-rater reliability of the diastometer for measurement of IRD was fair/moderate (ICC2.2: 0.471) at the umbilicus and excellent (ICC2.2: 0.881 and 0.902) above and below the umbilicus, respectively. It also showed good to excellent (ICC2.2: 0.723–0.906) for depth as shown in Table 5. Table 6 presents the concurrent validity of palpation, digital calipers, and diastometer against USI in IRD measurement. The palpation (ICC2.2: 0.007–0.256), digital calipers (ICC 2.2: 0.035–0.304), and diastometer (ICC2.2: 0.159–0.250) showed poor levels of agreement between the IRD values measured with USI at the three reference points. Comparisons of IRD measurements with palpation, digital calipers, diastometer, and USI showed significant difference (P = 0.000) at the level of the umbilicus only as shown in Table 7. Bland-Altman plot showed a poor level of agreement at all reference points Figures 1-3.
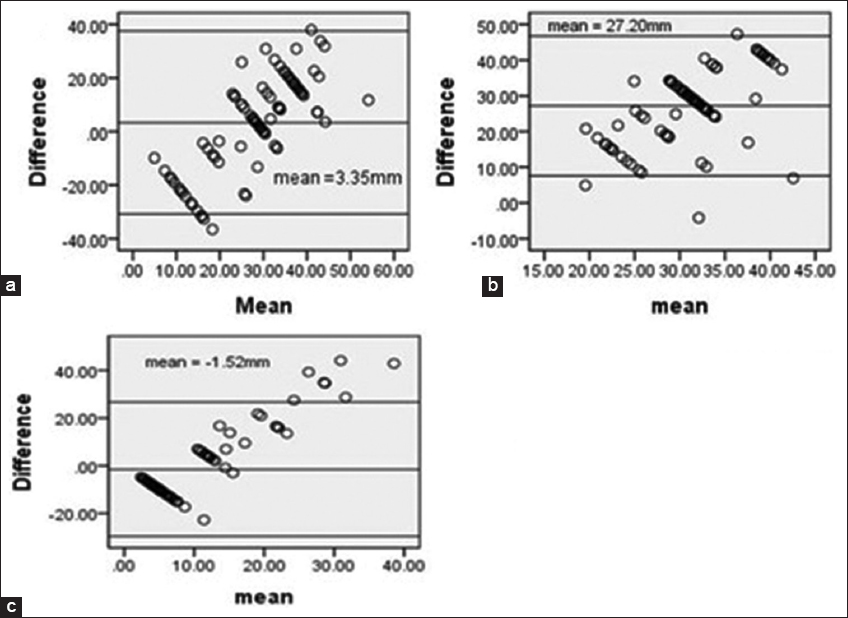
- Bland Altman plots of IRD (mm), comparing palpation technique and USI measurements (a) above the umbilicus, (b) at the umbilicus, and (c) below the umbilicus
- Bland Altman plots of IRD (mm), comparing calipers technique and USI measurements. (a) Above the umbilicus, (b) at the umbilicus, and (c) below the umbilicus
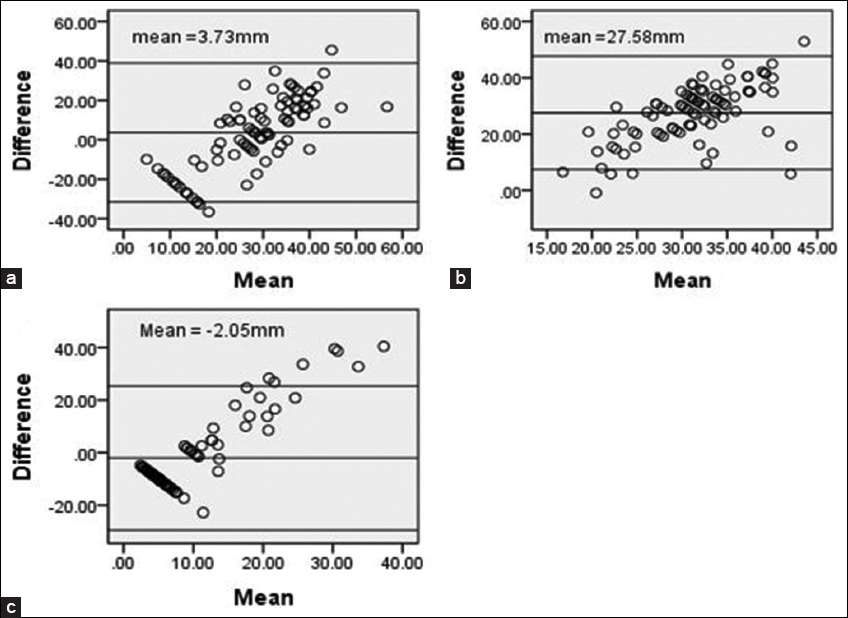
- Bland Altman plots of IRD (mm) comparing diastometer and USI measurements. (a) Above the umbilicus, (b) at the umbilicus, and (c) below the umbilicus
Discussion
This study investigated the intra- and inter-rater reliability of measures in the diagnosis of DRA i.e. palpation, digital calipers, and diastometer as well as their concurrent validity against USI. Most of the participants were overweight, multiparous women who delivered through spontaneous vagina delivery.
Reliability and Validity of the Palpation Technique:
This study showed that the palpation technique of measuring DRA has excellent intra- and inter-rater reliability. This infers that the palpation technique is a consistent measure for DRA across raters and for a single rater. There were concerns about differences in finger widths, thick abdominal subcutaneous fat, and flaccidity. However, the study findings showed excellent intra- and inter-rater reliability of this technique. These findings corroborate,[30] which similarly showed good intra-rater but moderate inter-rater reliability of this technique. On the contrary, Bursch[29] reported poor inter-rater reliability of this technique among four raters who measured IRD of postpartum women within <4-day post-delivery. The differences in the study findings may be attributed to the number of raters per study as well as their finger anthropometric characteristics.
The IRD values obtained with the palpation technique showed no agreement with the USI values. There were also significant variations between their recorded values. These findings suggest that the palpation technique cannot be considered a valid modality for DRA measurement, relative to the gold standard USI. This is supported by a prior study[29] which reported a similar outcome, showing poor validity of the palpation technique. Interestingly, another study[38] claimed that this technique has good concurrent validity. These variations are hardly surprising given that the measurement system of the palpation technique and USI differ considerably. It should be noted that USI measurement is on a continuous scale in millimeters while the palpation technique is based on finger width estimations.
Reliability and validity of the digital calipers
This study demonstrated good to excellent intra-rater and inter-rater reliability for the digital calipers. This evidence presents digital calipers as a reliable clinical tool for assessing DRA within and across raters. This finding concurs with the previous studies[17,27-39] which showed excellent intra-rater reliability, with high inter-rater reliability demonstrated in.[17,40]
The concurrent validity outcomes of the digital calipers showed no variations across the three measurement points. It recorded poor agreement with USI findings at all three reference points. This is in agreement with[40] but at variance with studies[31,38,39] which reported that it has good concurrent validity when used for DRA measurements above the umbilicus and below the umbilicus.[38] This lack of agreement between the digital calipers and USI may be attributed to the inherent weakness of the calipers as it cannot delineate body structures but the USI can, as different body structures reflect sound waves differently.
Reliability and validity of the diastometer
This study showed that the diastometer has good to excellent intra- and inter-rater reliability IRD assessment. The diastometer is a novel instrument for measuring IRD. At present, there is a paucity of related data on its clinimetric properties to fuel further discussion of the present study findings. This gap in knowledge about this instrument is one this study aimed to fill, further adding to its novelty. Nevertheless, its structure and mechanism of operation may give it an edge over other modalities because of its ability to measure diastasis depth. Relative to its function of measuring diastasis depth, this study also showed good to excellent intra-rater reliability for the diastometer. Its inter-rater reliability for assessing diastasis depth was moderate to excellent. In consideration of the above, the diastometer is seemingly a reliable tool for measuring IRD and depth within or across raters. These findings support the claims of its inventor[26] that it can be used for self-evaluation by patients without recourse to the clinician. Furthermore, the reliability of the depth component makes it clinically useful for both assessment and management of DRA.
This study revealed poor concurrent validity of the diastometer against USI at all the reference points. This suggests that this modality cannot be used as a replacement of the gold standard USI. Its use as a stand-alone assessment tool may be problematic as the diagnosis would require USI confirmation. USI is considered to possess a high level of accuracy even when compared to intraoperative surgical compass.[22]
Conclusion
The palpation, calipers, and diastometer techniques are reliable measures of DRA but not valid substitutes to USI for the assessment of DRA. The use of these instruments for clinical assessment of DRA should be recommended, particularly in scenarios where USI is neither accessible nor affordable.
Authors’ Declaration Statements
Ethics approval and consent to participate
Ethical approval was obtained from Research Ethics Committee College of medicine, University of Nigeria, Enugu campus and the Research, Education and Training Committee (RET) of ESUTHP, Enugu, Nigeria. All participants gave written informed consent before participation in the study.
Consent for publication
The authors jointly approved the publication of this manuscript.
Availability of data and material
Data and materials will be provided on request.
Competing interests
No conflicts of interest.
Funding statement
No financial sponsorship.
Authors’ contributions
Ojukwu Chidiebele Petronilla: conception, design, analysis and interpretation of data.
Ezeigwe Anne Uruchi: conception, design, data collection and drafting of article
Ezeigwe Chukwudi Francis: conception, interpretation of data and drafting of article.
Ugwuonye Chioma Linda: data collection and drafting of article.
Final approval of the version to be published was approved by all authors.
Acknowledgment
We wish to acknowledge the study center and all participants.
References
- Diastasis recti abdominis-a review of treatment methods. Ginekol Pol. 2018;89:97-101.
- [Google Scholar]
- The relationships between inter-recti distance measured by ultrasound imaging and abdominal muscle function in postpartum women:A 6-month follow-up study. J Orthop Sports Phys Ther. 2011;41:435-43.
- [Google Scholar]
- Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods:A systematic review. Physiotherapy. 2014;100:1-8.
- [Google Scholar]
- Diastasis recti abdominis:A survey of women's health specialists for current physical therapy clinical practice for postpartum women. J Womens Health Phys Ther. 2012;36:131-42.
- [Google Scholar]
- Prevalence of diastasis recti abdominis in the population of young multiparous adults in Turkey. Ginekol Pol. 2011;82:817-21.
- [Google Scholar]
- Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther. 2015;20:200-5.
- [Google Scholar]
- Prevalence of diastasis of rectus abdominis muscle in immediate post-partum women of urban and rural areas. Eur J Pharm Med Res. 2016;3:460-2.
- [Google Scholar]
- Abdominal exercise with bracing, a therapeutic efficacy in reducing diastasis-recti among postpartal females. Int J Physiother Res. 2015;3:999-1005.
- [Google Scholar]
- Efficacy of tupler technique on reducing post natal diastasis recti:A controlled study. Curr J Appl Sci Technol. 2016;12:1-8.
- [Google Scholar]
- How to treat diastasis recti abdominis with physical therapy:A case report. J Dis. 2016;3:16-20.
- [Google Scholar]
- Effects of abdominal exercises on reduction of diastasis recti in postnatal women. Int J Health Sci Res. 2016;6:182-91.
- [Google Scholar]
- The effects of a 6 week dynamic core stability plank exercise program compared to a traditional supine core stability strengthening program on diastasis recti abdominis closure, pain, oswestry disability index (ODI) and pelvic floor disability index scores (PFDI) Phys Ther Rehabil. 2016;3:3.
- [Google Scholar]
- Diastasis recti abdominis (DRA):Review of risk factors, diagnostic methods, conservative and surgical treatment. Clin Exp Obstet Gynecol. 2022;49:111.
- [Google Scholar]
- The normal width of the linea alba in nulliparous women. Clin Anat. 2009;22:706-11.
- [Google Scholar]
- Analysis of the abdominal musculo-aponeurotic anatomy in rectus diastasis:Comparison of CT scanning and preoperative clinical assessment with direct measurement intraoperatively. Hernia. 2014;18:465-71.
- [Google Scholar]
- The effects of an exercise program on diastasis recti abdominis in pregnant women. J Womens Health Phys Ther. 2005;29:11-6.
- [Google Scholar]
- Ultrasound imaging in postpartum women with diastasis recti:Intrarater between-session reliability. J Orthop Sports Phys Ther. 2015;45:713-8.
- [Google Scholar]
- Pelvic floor muscle function, pelvic floor dysfunction and diastasis recti abdominis:Prospective cohort study. Neurourol Urodyn. 2017;36:716-21.
- [Google Scholar]
- Measurement methods to assess diastasis of the rectus abdominis muscle (DRAM):A systematic review of their measurement properties and meta-analytic reliability generalisation. Man Ther. 2016;21:41-53.
- [Google Scholar]
- Prevalence, potential risk factors and sequelae of diastasis recti abdominis. Orv Hetil. 2017;158:454-60.
- [Google Scholar]
- Ultrasonography for measuring rectus abdominis muscles diastasis. Acta Cir Bras. 2007;22:182-6.
- [Google Scholar]
- Test-retest and intrarater reliability of 2-dimensional ultrasound measurements of distance between rectus abdominis in women. J Orthop Sports Phys Ther. 2012;42:940-6.
- [Google Scholar]
- Diastasis recti abdominis in pregnancy and postpartum periods. Risk factors, functional implications and resolution. Curr Womens Health Rev. 2015;11:59-67.
- [Google Scholar]
- 2015. Apparatus and Method for Detecting Diastasis Recti-US Patent APP. Available from: https://patents.google.com/patent/us20150105697a1/en
- Intra-rater reliability of rectus abdominis diastasis measurement using dial calipers. Aust J Physiother. 1997;43:109-14.
- [Google Scholar]
- Natural resolution of rectus abdominis diastasis. Two single case studies. Aust J Physiother. 2000;46:301-7.
- [Google Scholar]
- Interrater reliability of diastasis recti abdominis measurement. Phys Ther. 1987;67:1077-9.
- [Google Scholar]
- Reliability of the inter-rectus distance measured by palpation. Comparison of palpation and ultrasound measurements. Man Ther. 2013;18:294-8.
- [Google Scholar]
- Diastasis of rectus abdominis in the immediate puerperium:Correlation between imaging diagnosis and clinical examination. Arch Gynecol Obstet. 2013;288:299-303.
- [Google Scholar]
- Statistical Power Analysis for the Behavioral Sciences (2nd ed). Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988.
- Structure and function of the abdominal muscles in primigravid subjects during pregnancy and the immediate postbirth period. Phys Ther. 1996;76:750-62.
- [Google Scholar]
- Incidence of diastasis recti abdominis during the childbearing year. Phys Ther. 1988;68:1082-6.
- [Google Scholar]
- Predictors of inter-recti distance in cadavers. J Womens Health Phys Ther. 2012;36:125-30.
- [Google Scholar]
- Diastasis rectus abdominis and lumbo-pelvic pain and dysfunction-are they related? J Womens Health Phys Ther. 2009;33:15-22.
- [Google Scholar]
- Foundations of Clinical Research:Application to Practice (3rd ed). Upper Saddle River, N. J: Pearson/Prentice Hall; 2009.
- Establishing measurement properties in the assessment of inter-recti distance of the abdominal muscles in a postnatal women. Musculoskelet Sci Pract. 2020;49:102202.
- [Google Scholar]
- Concurrent validity of calipers and ultrasound imaging to measure interrecti distance. J Orthop Sports Phys Ther. 2013;43:495-503.
- [Google Scholar]
- The digital Caliper's interrater reliability in measuring the interrecti distance and its accuracy in diagnosing the diastasis of rectus abdominis muscle in the third trimester of pregnancy. J Chiropr Med. 2020;19:136-44.
- [Google Scholar]







