Translate this page into:
Primary cutaneous CD8-positive T-cell lymphoma-granulomatous mycosis fungoides: A rare case report
Address for correspondence: Dr. Divya Shetty, Department of Pathology, Dr. D.Y. Patil Medical College, Hospital and Medical Research Centre, Navi Mumbai, Maharashtra, India. E-mail: divya_shetty61@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
ABSTRACT
Granulomatous mycosis fungoides (GMF) is a rare subtype of T-cell cutaneous lymphoma. Due to the lack of distinct clinical features, GMF may pose a diagnostic challenge, which results in diagnostic delay. The diagnosis is based on histopathological and immunohistochemical findings. Herein, we present an 82-year-old male with itchy lesions over the scalp, face, forearms, trunk, and bilateral lower limbs for 6 months. Histologically, it was a CD8-positive GMF. GMF is a rare subtype of mycosis fungoides with <100 cases in the literature, and most of these cases showed a CD4-positive phenotype. CD8-positive GMF is extremely rare. We observed that it commonly affects elderly females. The patients often present with nodules and do not carry an adverse prognosis.
Keywords
CD8-positive
granulomatous mycosis fungoides
granulomatous slack skin
mycosis fungoides
Introduction
Mycosis fungoides (MF) is the most common type of cutaneous T-cell lymphoma (CTCL). It accounts for around 50% of the cases and a worldwide incidence of about five–six cases/million person-years.[1] There are several clinical variants of MF each of which has its characteristic pathomorphological features. Similarly, there are pathologic/immunophenotypic variants of MF, which correspond to distinct clinical features.
Granulomatous mycosis fungoides (GMF) is an uncommon histopathological variant of MF. It is characterized by the presence of granulomatous reactions within and around the atypical lymphocytic infiltrate.[2,3] <100 cases of GMF have been reported in the literature, and most of these cases are CD4-positive.[4-6] CD8-positive GMF is extremely rare, and information on its clinicopathological features is limited. We present a CD8-positive GMF in an 82-year-old male and compare our case with other similar cases from the literature to elaborate on the clinical and histomorphological features of this entity.
Case Report
An 82-year-old married male, a retired security guard by profession, came to our dermatology outpatient department with chief complaints of itchy lesions over the scalp, face, forearms, trunk, and bilateral lower limbs for 6 months. The lesion was initially pea-sized and present over the right forearm which was itchy and slowly increased to its current size. Over a period of 6 months, newer lesions appeared over the same sites. Existing lesions over the right forearm and left nasolabial fold developed raw areas. Treatment from a local doctor showed no improvement. The patient’s medical history is significant for diabetes mellitus for 6 years and he is on oral hypoglycemic agents but with poor blood sugar control. There was no history of arthralgia, radiation, or chemical exposure, no swellings in any part of the body, and no bleeding from any orifice. The patient has no history of addictions.
On examination, well-defined multiple erythematous non-tender firm nodules, measuring approximately 2×2 cm, were present on the scalp, face, trunk, abdomen, thighs, and lower legs. Two well-defined erythematous nodules were present near the left nasolabial fold, one of which showed a well-defined ulcer with undermined borders and pale granulation tissue, measuring approximately 3×3 cm. One well-defined ulcerated plaque, measuring approximately 4×5 cm with a few surrounding satellite nodules was present on the right forearm [Figure 1]. A provisional clinical diagnosis of squamous cell carcinoma, MF, tuberculoid leprosy, prurigo nodularis was suspected.

- Multiple ulcerated nodules over the face and leg
A superficial biopsy was taken from the right forearm and sent to the histopathology department. Histopathological evaluation revealed skin with focal ulceration and atrophy. The dermis showed multiple ill-defined non-caseating granulomatous lesions comprising epithelioid cells, lymphocytes, Langhans, and foreign body types of giant cells with foamy histiocytes. A repeat wedge biopsy was sent from the same site which showed skin with focally ulcerated and atrophied epidermis. The dermis and the subcutaneous tissue showed multiple foci of well-formed granulomas comprising epithelioid cells, multinucleated giant cells, interspersed lymphocytes, and eosinophils [Figure 2]. Furthermore, many large Reed-Sternberg-like cells were seen. The immunohistochemistry staining shows diffuse and strong positivity of CD3 which indicates the T-cell origin of the lesion. It also shows positivity in both CD4 and CD8 stains. The cells are negative for CD20, which rules out the B-cell origin of this lesion [Figure 3]. Hence, the diagnosis of CD8-positive GMF was given.
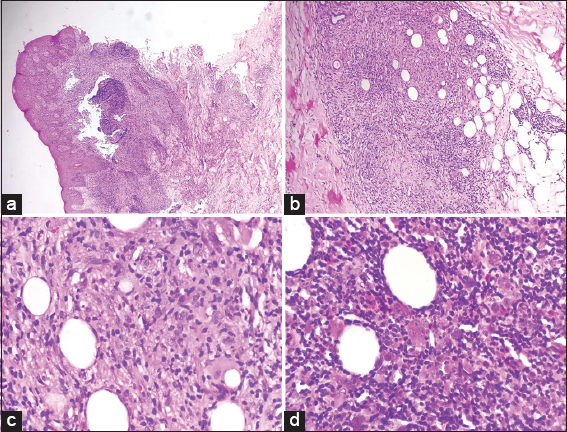
- (a) Granulomas in the dermis and subcutaneous tissue with epidermal sparing (Hematoxylin and Eosin stain, 40×); (b) non-necrotising granuloma (Hematoxylin and Eosin stain, 100×); (c) epithelioid cells and few giant cells (Hematoxylin and Eosin stain, 400×); D) atypical cells and giant cells with lymphoid infiltrate (Hematoxylin and Eosin stain, 400×)
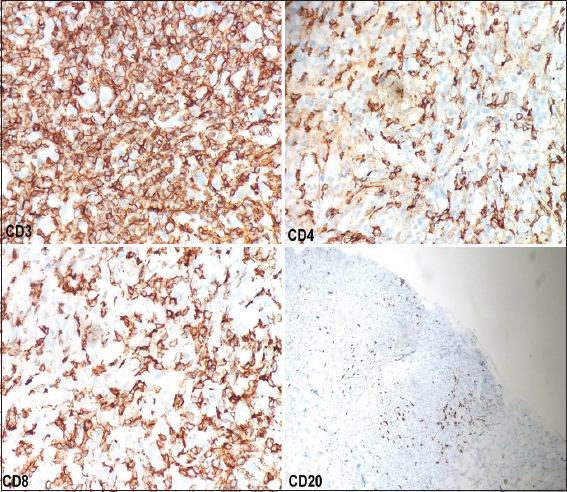
- Immunohistochemistry shows diffuse and strong positive for CD3, CD4, and CD8 but negative for CD20
Discussion
GMF is an epidermotropic primary CTCL. It is a rare histopathological variant of MF and accounts for around 4% of MF.[2] This variant was first described by Ackerman and Flaxman[7] in 1970, in a patient with tumor-stage MF with giant cells within the dermal infiltrate.
It is more common in males between the 5th and 6th decades of life. It has a characteristic evolution that begins typically as slowly progressive dermatitis-like patches and plaques and if left untreated evolves to nodules and eventual systemic dissemination.[2,4] The patch/plaque stage of the disease is the result of intraepidermal and superficial dermal infiltration by small to medium-sized malignant T cells with characteristic cerebriform nuclear contours, whereas the more advanced stages develop as a consequence of exclusively dermal involvement by non-epidermotropic, often cytologically more atypical malignant T cells.[8]
The presence of a granulomatous reaction is a well-known and not uncommon phenomenon in association with nodal lymphoma, especially Hodgkin lymphoma, and malignant T-cell lymphoma. In contrast, primary cutaneous lymphoma accompanied by the granulomatous reaction is rare, and a previous report revealed that only 1.8% of all primary cutaneous lymphomas displayed granulomatous features.[4] It is defined as the presence of granulomas representing at least 25% of the dermal infiltrate.[4] Granuloma formation has been reported in various types of primary cutaneous lymphomas such as Sézary syndrome, cutaneous anaplastic large cell lymphoma, subcutaneous panniculitis-like T-cell lymphoma, and primary cutaneous B-cell lymphoma. However, there are reports in the literature about forms that also mimic annular granuloma, lipoid necrobiosis, granulomatous rosacea, and granulomatous panniculitis. More than one pattern may coexist in the same patient.[9]
The etiopathogenic mechanism of granuloma formation is unknown. It was suggested that the granulomatous reaction occurs due to the secretion of chemotactic factors by neoplastic cells.[9] Some authors believe that the granuloma represents a host’s attempt to stop the lymphoma, thus indicating a good prognosis.
GMF is histopathologically characterized by the presence of variable granulomatous inflammation, which may take the forms of interstitial, tuberculoid/sarcoidal, or palisading granulomata reminiscent of granuloma annulare or necrobiosis lipoidica. Multinucleated giant cells, usually of the foreign body type (Langerhans and Touton giant cells have been described as well) with or without focal elastophagocytosis.[2]
Granulomatous slack skin (GSS) is a subtype of MF which also shows the presence of granulomas (elastolytic-type) in association with a dense dermal lymphomatous component that extends into the subcutis. Histopathologically, atypical T-cell infiltrates, often associated with epidermotropism or folliculotropism, non-caseating granulomas comprising of histiocytes and multinucleated giant cells that may contain ingested elastic fibers or engulfed lymphocytes (emperipolesis). Despite rare cases showing overlapping features, GMF can be differentiated from GSS clinically by the absence of bulky skin lesions and histologically by the lack of extensive elastolysis/elastophagocytosis and dense infiltrate with deep subcutaneous involvement.[2,8]
The diagnosis of GMF depends exclusively on the histopathological findings, as it lacks a distinctive clinical feature. It may present with an extensive granulomatous inflammatory infiltrate which may result in a misdiagnosis of granulomatous dermatitis, and the diagnosis of lymphoma may be postponed. Immunohistochemically, the atypical lymphocytes of GMF express CD3, CD4, and CD5, but lack CD20 expression.[2,8] The clonal T-cell receptor gene rearrangement test is important in this case as it confirms the monoclonality of T-cells, aiding in the accurate diagnosis of GMF and differentiating it from reactive conditions.
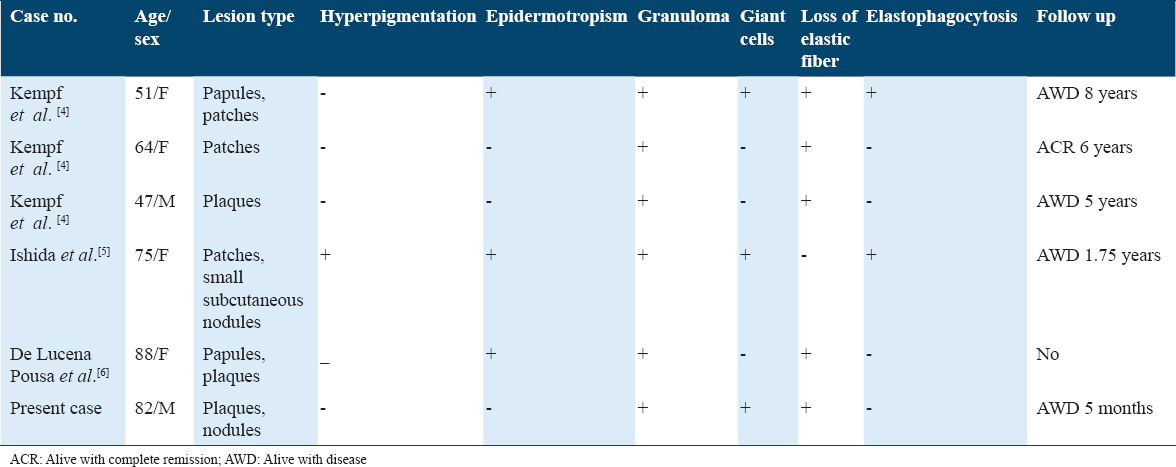
To the best of our knowledge, CD8-positive GMF is extremely rare. To date, six cases have been reported, including the current case [Table 1].[4-6] On comparing these cases we observed that only the elderly were affected >50 years and a female predilection was seen with a male: female ratio of 1:2. The majority (66.7%) had nodules/papules at the time of presentation. Hyperpigmentation was only observed by Ishida et al.[5] The most common histomorphological finding was the presence of granulomas, loss of elastic fibers, and absence of elastophagocytosis. Epidermotropism and giant cells were present in 50% of the cases. Six cases are too few to allow meaningful comment on the prognosis. However, the longest follow-up of these cases was 8 years and none showed an adverse prognosis.
Conclusion
In conclusion, this report describes a CD8-positive GMF. Our findings suggest that it is a disease of the elderly females. It presents at a later stage (nodule) and typically lacks abnormal pigmentation. The characteristic histomorphological features are the presence of non-necrotizing granulomas with a lack of elastic fibers, and elastophagocytosis. They are not associated with an adverse prognosis.
Author’s Declaration Statements
Ethics approval
Ethics committee approval was not required for this case report, as the patient’s information was anonymized, and no identifiable data were included. The case was reviewed and anonymized in accordance with institutional guidelines on the use of medical records for educational purposes.
Declaration of patient consent
The authors certify that they have obtained consent from the patient for images and other clinical information to be reported in the journal.
Financial support and sponsorship
Nil.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of interests
The authors declare that they have no conflict of interest.
Source of funding
Not funded.
References
- Granulomatous mycosis fungoides with hypohidrosis mimicking lepromatous leprosy. Indian J Dermatol Venereol Leprol. 2010;76:686-90.
- [Google Scholar]
- Granulomatous mycosis fungoides and granulomatous slack skin:A multicenter study of the Cutaneous Lymphoma Histopathology Task Force Group of the European Organization for Research and Treatment of Cancer (EORTC) Arch Dermatol. 2008;144:1609.
- [Google Scholar]
- CD8+ mycosis fungoides with esophageal involvement:A case report. Oncol Lett. 2013;5:73-5.
- [Google Scholar]
- Granulomatous mycosis fungoides--a diagnostic challenge. An Bras Dermatol. 2015;90:554-6.
- [Google Scholar]
- Cutaneous lymphomas showing prominent granulomatous component:Clinicopathological features in a series of 16 cases. J Eur Acad Dermatol. Venereol. 2009;23:639-47.
- [Google Scholar]







