Translate this page into:
A case series of autologous platelet-rich plasma injection in treating chronic ulcers conducted in Saudi Arabia
* Address for correspondence: Sinan F. Tabanjeh, Kahel Specialized Centre, Riyadh, Saudi Arabia. E-mail: sinantabanjeh@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
This is a case series study of 14 cases of chronic unhealed ulcers involving patients of 19–85 years, aimed to demonstrate the positive therapeutic outcomes of using autologous platelet rich plasma (PRP) in diabetic foot ulcer (DFU) and other chronic wound healing.
Methods:
This is a formal consecutive clinical case series. Patients with chronic unhealed ulcers were enrolled from the amputation prevention clinic by an interdisciplinary team includes podiatrist, general surgeon, orthopedic, vascular surgeon, and wound care nurses at Kahel Specialized Centre, a specialized center for managing foot and ankle diseases, located in Riyadh, Saudi Arabia. Those patients who presented with chronic wounds and showed no significant wound reduction despite following the standard wound care protocol were included in the study. There were no specific predetermined exclusion criteria when considering patients for treatment with this modality.
Results:
In this case series, majority (80%) of the patients were above 50 years of age, and 10 (66.7%) patients were male and 5 (33.3%) were female. Of all the cases presented to the amputation prevention clinic, majority (73.3%) reported suffering from type 2 diabetes mellitus (DM) and also, one reported type 1 DM [6.7%]). All the cases of DFU received a combination of hydrogel and autologous PRP treatment and were put of suitable offloading devices, except one case received a combination of Cadexomer iodine, hydrogel and PRP treatment. In the present case series involving 3–14 weeks of the treatment duration, only 2–3 doses of autologous PRP provided complete healing and or maximum wound closure.
Conclusion:
Autologous PRP therapy is efficacious in facilitating, enhancing wound healing and aids in complete wound closure. This case series was limited in term of the sample size which is the number patients enrolled for the study, hence, the study finding remain inconclusive to some extent and hence, further study is required with greater number of sample size. The strength of this study is that it is the first study in Saudi Arabia and gulf region, to report the beneficial effect of PRP in chronic unhealed ulcers including diabetic ulcers.
Keywords
Chronic wounds
diabetes mellitus
diabetes mellitus complications
diabetic foot ulcer
platelet-rich plasma
Introduction
Diabetes mellitus (DM) is a major public health outcry, as it is increasing at rapid pace.[1] Its global prevalence grew from 108 million in 1980–422 million in 2014,[2,3] and according to global surveys on diabetes, the global diabetes prevalence in 2019 was estimated to be 463 million people, rising to 578 million by 2030 and 700 million by 2045.[4,5] In Saudi Arabia, one out of every four Saudi adults suffer from DM.[6] More than 44% of patients with 55 years old and older in Saudi Arabia had long-term complication related to severe or uncontrolled DM.[7] A gathering body of evidences indicate that nearly 25% of patients suffering from diabetes develop diabetic foot complications during their lifetime,[8,9] and the lifetime risk of foot ulcers has been found between 15% and 25% which may go up to 34%.[10]
The annual risk of diabetic foot ulcer (DFU) in diabetes patients has been reported to be around 2–2.8%, which may go up to 17–60% in the next 3 years, in patients with past medical history of foot ulcer.[11,12] In Saudi Arabia, the majority of lower limb amputations is attributed to DFU and it was reported to be the cause of amputation in 49.6% of cases during the past two decades[13] which is expected to increase further in the years to come.[14,15] A study from Saudi Arabia showed that diabetic foot was prevalent in 3.3% of 62,681 diabetic patients; with 2.05% suffered foot ulcer and 1.06% had amputation.[16] Age, diabetic duration, smoking, obesity, hypertension (HTN), osteomyelitis, poor ankle-brachial index, and high neutrophil/lymphocyte ratio were strongly linked to the development of DFU.[17,18] Moreover, according to a study, patients’ age and duration of diabetes increase the risk of diabetic foot complications by as high as 50%.[19] The previous history of DFU or amputation, insulin intake, gender, neuropathy, and foot deformity has been reported as independent risk factors of DFU indicating a multifactorial etiopathogenesis.[12] In the developed, DFUs accrue over 12–15% of total estimated cost of diabetes which increases up to 40% in the developing countries.[20] It is a common and major complication of both the type1 and type 2 DM, representing a major healthcare burden with significant morbidity.[21,22] Around half of the patients of DM would eventually develop DFU and it is also the cause of non-traumatic lower limb amputation in a majority of patients who have developed DFU.[23,24] DFU involves different degrees of neuropathy and angiopathy that affect the foot causing the destruction of tissues, infection, and ulceration.[17,25,26] There are several risk factors which are tied to diabetic foot occurrences including poor metabolic control, duration of diabetes, foot deformities, peripheral vasculopathy, older age, and poor knowledge of diabetics.[17] Among diabetics, years of poorly controlled hyperglycemia lead to multiple, primarily vascular, complications that affect small vessels (microvascular), large vessels (macrovascular), or both which only causes DFU but also nephropathy, retinopathy, and neuropathy including atherosclerotic disorders affecting cardiovascular system.[27]
There are several ulcer classification systems which have been adopted and were designed based on parameters such as extent of infection, neuropathy, ischemia, depth of penetration or extent of tissue loss, the presence of osteomyelitis or gangrene, and location.[28,29] Wagner classification is one of the most widely accepted and simple wound classification system designed so far for assessing DFUs and lesions.[28,30-32] Wagner classification ranges from grade “0” to “5.” According to the Wagner classification, Grade “0”: skin intact but bony deformities lead to “foot at risk;” Grade “1:” Superficial ulcer; Grade “2:” Deeper, full thickness extension; Grade “3”: Deep abscess formation or osteomyelitis; Grade “4:” Partial Gangrene of forefoot; and Grade “5:” Extensive Gangrene. A recent study reported that classification of diabetic foot patients and initiation of treatment plans based on their Wagner’s grade have helped lower rate of amputation and deaths. In addition, it lays emphasis on a multichannel management and exceptional attention to diabetes and lifestyle control which would significantly improve long-term outcomes.[31] However, this classification system, also, has some down sides which are its limitation to address two key parameters: Ischemia and infection.[30,33]
Alvarsson et al.[34] reported that up to 88% of all lower leg amputation is related to diabetic foot ulcer. The goal of the DFU treatment is to obtain ulcer closure as expeditiously as possible.[9,33] According to a study, in Saudi Arabia, mean prevalence of DFU has been reported to be 11.85% (4.7–19%), while another study reported it to be 1.8% between 2009 and 2010.[35] According to another study from Saudi Arabia, overall health-care expenditure in treating DFU was very high, with hospital admissions and surgical procedures added greatly to the total cost of treating DFU.[36] Accepted therapeutic objectives and standards of care for DFU include ulcer debridement, pressure relief at the area ulcerated, appropriate wound management (e.g., moist wound healing), infection management, ischemia management, medical management of comorbidities, and surgical management as needed,[37] However, in recent years, great progress has been made in the techniques of wound healing, of which autologous platelet-rich gel therapy has attracted the most attention.[38]
Platelet-rich plasma (PRP) is referred to as a portion of the plasma fraction of autologous blood having a platelet concentration above baseline. It is basically a platelet-enriched plasma, platelet-rich concentrate, autologous platelet gel, and platelet release.[39-41] PRP serves as a tissue sealant which initiates wound healing by releasing growth factors which may also reduce inflammation by suppressing cytokine release.[42,43] PRP has also been demonstrated to have some antimicrobial properties against microorganisms, such as Escherichia coli, MRSA, Candida albicans, and Cryptococcus neoformans.[44] PRP has been reported as an attractive choice in management of chronic non-healing diabetic ulcers if adequate blood supply and proper offloading has been provided.[45-48] PRP administration has been reported to have several benefits which include economical advantage, ease of administration as it does not require complex equipment or training. Moreover, it is primary of autologous origin, concerns of disease transmission or immunogenic reactions substantially less or nil. Thus, of late, platelet-enriched materials have become highly prescribed in the last decade and constitute a growing focus of experimental and clinical study in the context of wound healing and tissue regeneration.[49] The topical application of PRP for DFUs has resulted in superior healing rates and lower complication rates compared to controls.[50] In a randomized controlled trial, autologous PRP improved ulcer healing rate, shortened healing time, without an increase in the incidence of adverse events.[51]
Hence, this clinical case series of 14 cases of patients with unhealded chronic ulcers was aimed to investigate the positive therapeutic outcomes of using PRP in hastening the healing of chronic ulcers and also to highlight PRP as an adjunct therapy to standard of care in the treatment of diabetic wound and other chronic ulcers.
Methods
This is a formal, consecutive clinical case series of 14 cases of patients suffering from diabetic and other chronic unhealed wounds.
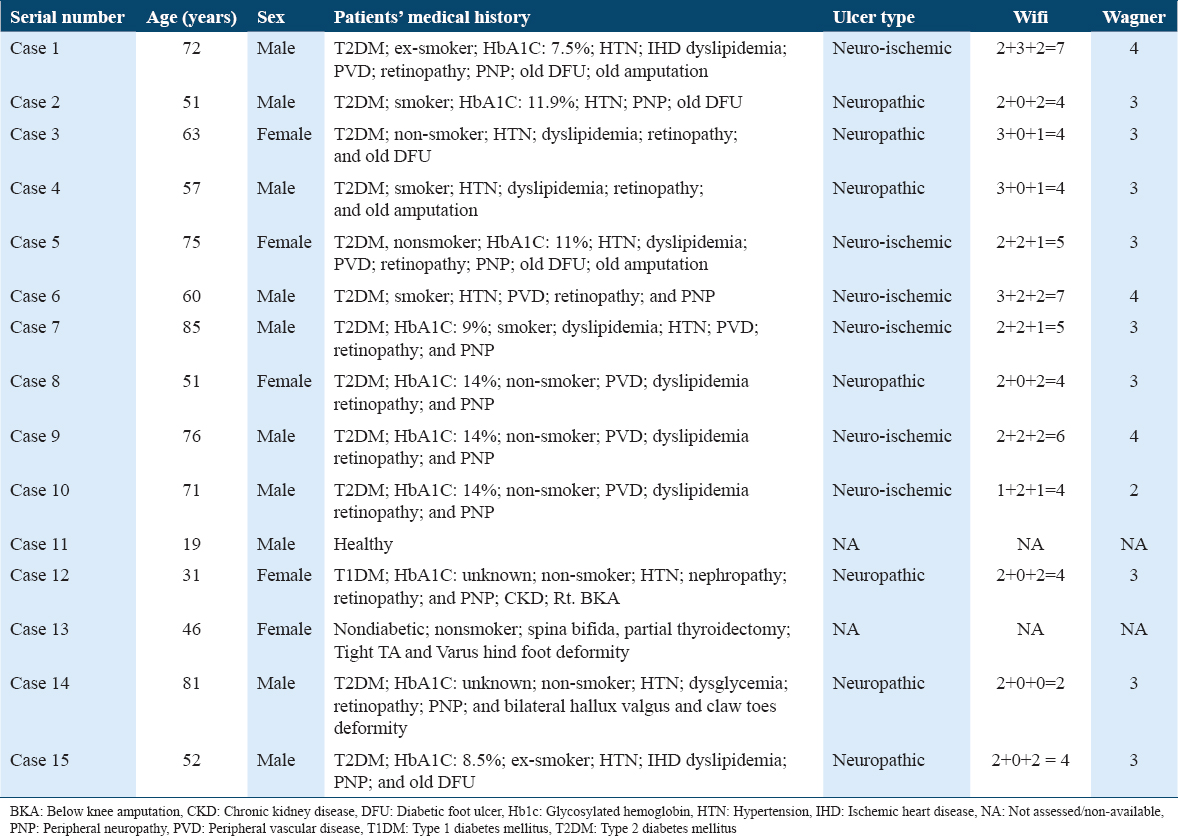
Patients with chronic unhealed ulcers were enrolled from the amputation prevention clinic by an interdisciplinary team includes podiatrist, general surgeon, orthopedic, vascular surgeon, and wound care nurses at Kahel Specialized Centre, a specialized center for managing foot and ankle diseases, located in Riyadh, Saudi Arabia [Table 1]. Those patients who presented with chronic wounds and showed no significant wound reduction despite following the standard wound care protocol for a minimum of 6 weeks were included in the study. There were no specific predetermined exclusion criteria when considering patients for treatment with this modality. Written informed consent was obtained from all patients for anonymized patient information to be published in this article. A general consent form to publish patient information was obtained from all the patients before the study. At the time of informed consent being obtained from each participant, digital photographs were taken of the reference wound. The CARE guidelines, a checklist to standardize reporting of case reports was followed and the study conducted in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
In this treatment plan of chronic ulcers, standard of care treatment was continued in addition to injection of PRP therapy. We followed the standards of obtaining PRP by Extracting 10 cc of blood, and filled it in a vacuum tube of sodium citrate and gel which manufactured by REGEN LAB. Then the tube was centrifuged in a centrifusion machine at 4000 rpm for 5 min, subsequently about 4–6 mL of plasma was separated. Plasma was extracted in a syringe and injected subcutaneous at the edges and directly to the granulating tissue, starting from the edges to the center to cover all area injured with a distance between each injection 3–5 mm. The injection procedure was repeated if needed every at least 7–10 days depending on size of ulcer, absence of infection signs, presence and amount of healthy tissue, and vascularity status.
Ethics approval and consent to participate
The study protocol received approval from the Research and Ethics Committee of Kahel Specialized Centre, Riyadh, Saudi Arabia (Approval number of ethical committee 007/2020). Written informed consent was obtained from all patients for anonymized patient information to be published in this article. A general consent form to publish patient information was obtained from all the patients before the study. At the time of informed consent being obtained from each participant, digital photographs were taken of the reference wound.
No animals were used in this study. The CARE guidelines, a checklist to standardize reporting of case reports was followed and the study conducted in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
Written informed consent was obtained from all patients for anonymized patient information to be published in this article. A general consent form to publish patient information was obtained from all the patients before the study. At the time of informed consent being obtained from each participant, digital photographs were taken of the reference wound.
Cases
Case 1
An ex-smoker 72-year-old male diabetic patient who presented to amputation prevention clinic with a case of DFU and gangrene at the 5th toe associated with right Charcot foot deformity. The patient health history revealed that he had developed several comorbid diseases including HTN, ischemic heart disease (IHD), retinopathy, and peripheral neuropathy (PNP) and his glycosylated hemoglobin level was 7.5%.
On the presentation; patient was treated by improving the blood circulation and patient underwent to lower limbs angioplasty which done successfully, then patient underwent to amputation of the 4th and 5th toes due gangrene and collection of infection at the dorsum of the foot which was not respond to treatments. The surgical intervention left an ulcer open which was difficult to close primarily. Patient made regular follow-ups in the clinic for about 6 weeks without significant decrease in size, despite of following the standards of diabetic foot care. Then, we have decided to include him with treatment program by using PRP injection to enhance the healing. His ulcer measured 101 mm (length) × 20 mm (width) × 12 mm (depth). He was treated with hydrogel along with the administration of PRP in the 1st week. Half shoes were used as off loader. Ulcer healing was noted with an improvement in the ulcer size with appreciable ulcer epithelialization during the 2nd week and the patient was continued on hydrogel treatment and advised the use of half shoes. There was further ulcer healing and large epithelialization with reduction in the ulcer size during the 3rd week, the patient was further treated with hydrogel and applied with PRP. During the 4th week, more than half of the ulcer epithelialized and the patient was applied hydrogel only. The ulcer had healed completely by the end of the 5th week.
Case 2
A 63-year-old female patient presented to the amputation prevention clinic with a case of unhealed DFU. Her medical history revealed type 2 DM (T2DM), HTN, dyslipidemia, PNP, and retinopathy. 4 months preceded the presentation, patient underwent to amputation of her 3rd and 4th toes due to severe infection, with regular follow-ups that’s failed to heal the ulcer. The ulcer appeared neuropathic type which had extensive ulcer and mild infection, and her toe pressure measured >60 mmHg. Ulcer measured 72 mm length and 14 mm width with moderate moist ulcer. During the 1st week of her presentation to the clinic, she was treated with hydrogel and also given PRP treatment to speed up the healing. She was kept on TCC as an off loading device. Hydrogel treatment was continued for 7 weeks while PRP was administered intermittently on week 3 and week 6. The patient’s ulcer healed completely by the 8th week of her treatment at the podiatry clinic.
Case 3
A 57-year-old male patient presented to the podiatry clinic with a case of unhealed DFU with ulcer probing to the bone. The patient’s medical history revealed that he was an ex-smoker, and suffering from T2DM, had HTN, dyslipidemia, and retinopathy. The patient ulcer indicated neuropathic type and showed extensive ulcer with mild soft tissue infection. His toe pressure measured >60 mmHg. Patient underwent a surgical intervention to excise the infected bone at the hallux with medicated cement impedes application. Post operatively, surgical ulcer partially dehisced due to skin tension. The ulcer measured 12 mm in length, 5 mm in width, and 7 mm in depth. The ulcer was treated with hydrogel along with PRP and half shoes were prescribed as an off-loader. Improvement in ulcer healing was observed in the 2nd week with reduction in ulcer’s size and fully granulation. Hydrogel was used and he advised to continue use half shoe for the next week. Ulcer healed completely during the 3rd week observation.
Case 4
A 75-year-old female patient who presented to the podiatry clinic with old DFU developed post trans metatarsal amputation due to gangrenous toes which has been done after successful lower limbs revascularization. The surgical ulcer almost healed and left 18 mm (length) × 15 mm (width) not healed. Her medical history revealed T2DM with poor glycemic control (HbA1C, 11%). She had HTN, dyslipidemia, IHD and retinopathy. She also reported peripheral vascular disease (PVD) and PNP. She had a neuro-ischemic type of ulcer. During the 1st week of her visit to the clinic, she was treated with hydrogel along with the administration of PRP. Approximation suture was also done on her ulcer and felted foam was applied as an off-loader. In her second next week follow-up, her ulcer improved with reduction in ulcer size. Hydrogel and PRP treatment was done while keeping the patient on felted foam for off-loading. In her 3rd week visit, the ulcer showed greater amount of healing with ulcer measuring only 11 mm (length) × 4 mm (width) in size and no depth. Only hydrogel treatment was applied and continued on felted foam off-loader. Her ulcer healed completely in 4 weeks duration of her treatment with hydrogel and PRP.
Case 5
A 60-year-old male patient presented to the amputation prevention clinic with 5th toe gangrene and cellulitis. His medical history suggested that he had HTN, retinopathy, and PVD and was also a smoker. Patient underwent to vascular assessment and revealed no significant occlusion or stenosis, then patient underwent to surgical irrigation and debridement with amputation of 5th toe. The surgical intervention left a large area of the ulcer open, measuring 100 mm (length) × 66 mm (width) × 20 mm (depth). The ulcer appeared erythematous with exposure of the dorsal tendons and metatarsal bones. On his first visit in the 1st week, his ulcer was treated with hydrogel along with PRP treatment for 5 weeks. Half shoes were prescribed as an off-loader. The patient’s ulcer improved gradually with disappearance of erythema and was granulating well. From week 6 to week 14, he was treated with hydrogel except on week 8 where both hydrogel and PRP treatment was given. The patient was treated for a total period of 15 weeks by the end of which the patient’s ulcer had healed completely.
Case 6
An 85 years old, known as T2DM, with poor glycemic control HbA1C 9%, HTN, Retinopathy, dyslipidemia, PVD and PNP, and had no history of prior DFU, and ex-smoker. Patient underwent peripheral revascularization to treat PVD, then he underwent to surgical intervention in form of irrigation and debridement with excision of osteomyelitis and application of medicated cement impedes. His ulcer was indicative of a neuro-ischemic type of ulcer. The ulcer was deep with mild cellulitis of <2 cm but the ulcer was probing to the bone. His toe pressure between 30 and 39 mmHg. The patient ulcer measured 20 mm (length) × 10 mm (width). The patient was treated until complete healing for a total period of 5 weeks. During the first and the 3rd weeks, the patient was treated with both the hydrogel and PRP therapy. He was suggested to use half shoes as off loader to support ulcer healing. The patient ulcer showed complete granulation with more than 50% epithelialization where ulcer’s size reduced to 4 mm (length) × 3 mm (width) with no depth, at week 4. The ulcer showed complete healing at week 5 and needed no treatment.
Case 7
A 51-years-old female patient presented to the amputation prevention clinic with ulcer at the plantar metatarsal area. Her medical history revealed that she had T2DM with poor glycemic control (HbA1c; 14%), retinopathy and dyslipidemia. She was also had PNP. Investigations of her ulcer were suggestive of a neuro-ischemic type which was deep with gangrene limited to toes and moderate infection. Her toe pressure measured >60 mmHg. The ulcer was 18 mm (length), 15 mm (width) and 9 mm (depth). Swab for culture and sensitivity revealed MRSA. The patient was treated with Cadexomer iodine in addition to systemic IV antibiotic (Imepenem), and advised half-shoe off-loader during the first visit. On her second visit, her ulcer measured 11 mm (length) × 5 mm (width) × 8 mm (depth) in size. She was treated with hydrogel and PRP and advised half shoes. She received only hydrogel treatment until week 6 and her ulcer showed significant healing with ulcer measuring 5 mm (length) × 3 mm (width) with no depth. At week 6, there was complete healing of ulcer.
Case 8
A 76-years-old, male patient, presented to the amputation prevention clinic with a medical history of T2DM and had also developed retinopathy and PNP. The patient presented with a DFU and had a previous amputation of the third and fourth toes. He however was not an active smoker. His current ulcer at the amputation site was suggestive of a neuro-ischemic type which was deep with gangrene limited to toes and moderate infection. His toe pressure measured >60 mmHg. During the 1st week observation, the patient’s ulcer measured 80 mm in length and 31 mm in width. He was given hydrogel and PRP treatment and advised to use half-shoes as off-loader. There was no appreciable change in the ulcer dimension during the 2nd week. The patient was administered hydrogel without PRP during the next 2 weeks. The patient again received treatment with hydrogel and PRP during the 4th week. Subsequently, he was treated with hydrogel alone until the 9th week and continued to use half-shoes as off-loader. The ulcer had significantly healed which was only 5 mm in length and 4 mm in width and at the end of the 10th week. By the 10th week, patient achieved the complete epithelialization and needed no treatment.
Case 9
A 71-years-old male, type 2 diabetic, visited the amputation prevention clinic with a history of PNP, dyslipidemia, and retinopathy. The patient had PVD but was a non-smoker. The patient presented with a neuro-ischemic type of ulcer at big toe which was small in size with no gangrene formation but showed signs of moderate cellulitis (>2 cm) and purulence discharge. His toe pressure ranged between 40 and 59 mmHg. Ulcer dimension was 40 mm in length and 18 mm in width. He was treated with hydrogel that applied regularly, and minor debridement, this plan kept for 4 weeks, but the ulcer getting worse, eschar tissue developed, no granulation or epithelialization, which was gradually. Swab for culture and sensitivity collected and shows no growth, while the toe pressure was the same result of before. In week 5, patient given one injection of PRP after doing a minor debridement, several days later, noticed a good granulation growth with size decreased significantly. By the week 14, the ulcer is completely healed and epithelialized.
Case 10
A 19-years-old male presented to the amputation prevention clinic with no medical history of illness. The patient was also a non-smoker. He presented with an ulcer measuring 28 mm in length, 30 mm in width, and 16 mm in depth. Ulcer resulted from trauma caused tibia fracture for 1 year ago. Ulcer was probed to the bone, and MRI shows osteomyelitis at the tibia. Orthopedic team intervenes to do surgical irrigation and debridement with excision of infected bone, and due to ulcer shape it was not possible to close it primarily. His ulcer was treated with hydrogel and PRP during the 1st week. From the 2nd till 4th week, his ulcer was treated with hydrogel alone during which the ulcer showed signs of healing with complete granulation. He was again treated with hydrogel and PRP during the 5th week because of delay in healing of the ulcer. Subsequently for the 6th and 7th week treatment, he received hydrogel treatment only which hastened the healing which was now 3 mm in length and 2 mm in width. The ulcer healed completely at the end of 8 week.
Case 11
A 31-years-old female presented to the amputation prevention clinic with a history of type 1 diabetes. Her medical history also revealed that she was having HTN, and had developed retinopathy, nephropathy and PNP. She was a non-smoker. She also had a history of below knee amputation. The investigation of her ulcer revealed a neuropathic type at the heel. The patient’s ulcer was deep with no signs of infection. Her toe pressure measured >60 mmHg. Her ulcer measured 58 mm in length, 60 mm in width and 21 mm in depth. She was administered with a hydrogel treatment with PRP at 1st week and advised heal protector as offloading device. Subsequently, she was treated with hydrogel alone for the next 4 weeks. At the 4th week examination, her ulcer reduced significantly in size which was 5 mm in length and 19 mm in width, and it was granulating very well. The ulcer dried up completely at the end of the 5th week and need no treated except the off loader as protection from recurrence.
Case 12
A 46-year-old female having spine bifida and Varus hind foot presented to the amputation prevention clinic. Her medical history revealed that she had partial thyroidectomy and complete PNP. The ulcer on her foot measured 13 mm in length, 10 mm in width and 8 mm in depth which not healed for more than 2 years. Her ulcer was treated with hydrogel and kept on TCC. During the 2nd week, she was treated with hydrogel as well as PRP and kept on TCC. She was further treated with hydrogel for another 2 weeks where the ulcer showed complete granulation and was progressing very well. The ulcer measured 2 mm in length and 3 mm in width. Her ulcer healed completely at the end of the 5th week and needed no further treatment.
Case 13
An 81-year-old male having T2DM presented to the amputation prevention clinic with a medical history of HTN, dyslipidemia, and PNP. The patient also had bone deformity in the form of severe bilateral hallux valgus and claw toes which was corrected surgically. 1 month later, the surgical ulcer was healed except 10 mm in length, 20 mm in width and 5 mm in depth. Failed to heal. His ulcer investigations were suggestive of neuropathic type which was deep with no signs of infection. His toe pressure measured >60 mmHg. His ulcer was treated with hydrogel and PRP without offloading device for the first, second and 4th week. At the 4th week, ulcer significantly granulated which reduced in size to 2 mm in length, 2 mm in width, and 3 mm in depth. The ulcer dried up and healed completely at the end of the 5th week and needed no further treatment.
Case 14
A 52-year-old male having T2DM (HbA1c:8.5%) presented to the amputation prevention clinic with a medical history of HTN, IHD, PNP, and old DFU. The patient was ex-smoker. The investigations of ulcer were suggestive of a neuropathic type which was deep with no signs of infection. Plain radiological exam of the foot shows Charcotic changes at the mid foot with unstable joint. His toe pressure measured >60 mmHg. During the first examination, his ulcer showed signs of moderate moisture and measured 80 mm in length, 35 mm in width, and 10 mm in depth. The patient’s ulcer was treated with hydrogel and PRP and put on wheelchair following the first visit. He was subsequently treated with hydrogel and kept on TCC at the third, fifth and 7th weeks and used wheelchair for the second, fourth and 6th weeks. The ulcer size reduced significantly but did not heal completely at the end of the 7th week and later on, the patient’s discontinued the treatment.
Results and Discussion
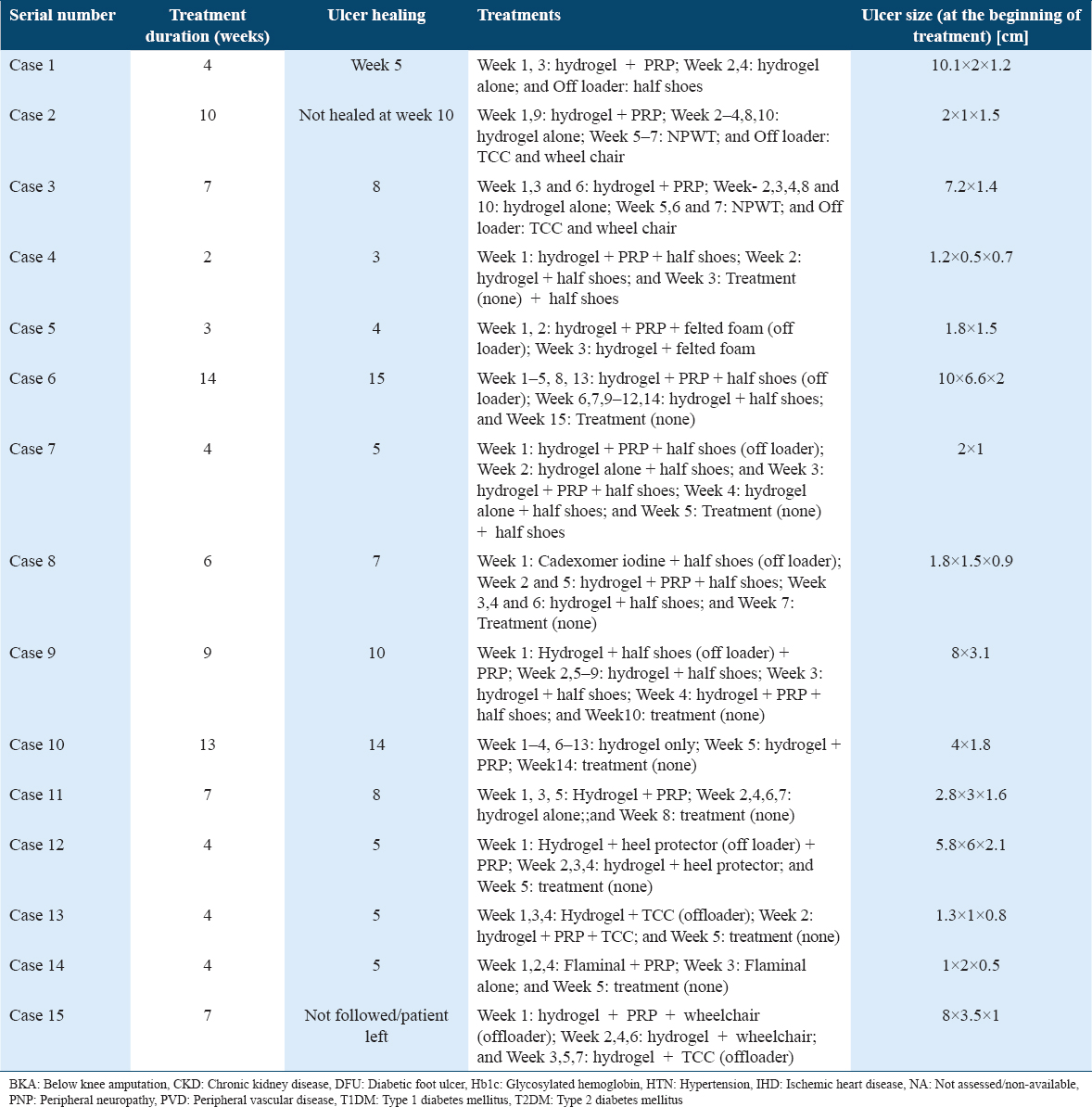
This is a case series of chronic unhealed ulcers involving 14 cases belonging to age groups ranging from 19 to 85 years. The details about the type of patients have been presented in Table 1 and Figure 1. In this case series, majority (80%) of the patients were above 50 years of age, and 10 (66.7%) patients were male and 5 (33.3%) were female. Of all the cases presented to the amputation prevention clinic, majority (73.3%) reported suffering from T2DM and also, one reported T2DM (6.7%), one (6.7%) case involved patient who was healthy and one (6.7%) patient was nondiabetic but reported thyroidectomy and spina bifida with Varus hind foot deformity. Furthermore, majority of the cases showed secondary diabetes complications such as retinopathy, PNP, HTN, PVD, and dyslipidemia. Furthermore, many of them were smokers or ex-smokers. The etiology of the foot ulcer must be determined before starting the treatment plans. Furthermore, it has been reported that ulcer classification before the initiation of ulcer therapy aid in the approach to treatment and help predict the outcome of the therapy.[28,29] The ulcer should be assessed with regard to severity, location, presence of infection, stage of healing, temperature, and odor. In line with this approach, we have also recorded these parameters before starting the therapy. Neuropathic foot ulcer types present less challenges compared to neuro-ischemic or ischemic ulcers which pose a higher risk of adverse outcomes, including non-healing, infection, amputation, and death.[52] In this case series, we observed that 9 (60%) of the cases were on Wagner grade 3, 3 (20%) on Grade 4, 1(6.7%) on Grade 2 and 2 (13.3%) were not applicable to the grading system. Furthermore, all the cases of DFU received a combination of hydrogel and autologous PRP treatment and were put of suitable offloading devices, except one case which received Flaminal and PRP combination and also one case received a combination of Cadexomer iodine, hydrogel, and PRP treatment. The standard management practices in DFU include surgical debridement, topical wound dressings to provide a moist environment, proper off-loading way, vascular assessment, presence of infection, and glycemic control.[53,54] Furthermore, aiding the pressure relief by the use of suitable off-loading device such as total contact cast, removable cast walkers, or “half shoes” have been used as the mainstay of the initial management plan.[30] There are several adjuvant therapies which have been added to lower ulcer healing times and amputation rates. The add-on include the following categories: nonsurgical debridement agents, dressings and topical agents, oxygen therapies, negative pressure wound therapy, acellular bio products, human growth factors, energy-based therapies, and systemic therapies.[53,54] Non-surgical debridement includes hydrogel, clostridial collagenase ointment, maggot/larval therapy, and hydro surgery.[55] Dressings and topical agents include various dressing types, honey, topical antimicrobials,[56] silver dressings, and polyhedral preparations have been efficacious in healing diabetic foot ulcers.[57] Oxygen therapies include topical oxygen therapy, and hyperbaric oxygen therapy.[58] According to a recent case series, NATROX topical oxygen therapy was found to an advanced topical oxygen delivery system compared to other conventional oxygen delivery systems.[58] Furthermore, human growth factors have been used to facilitate ulcer healing and include fibroblast growth factor, epidermal growth factor, vascular endothelial growth factor, and platelet-derived growth factors.[59-63] In addition, there are energy based therapies which include treatment with electrical stimulation therapy, shock wave therapy, electromagnetic therapy, laser therapy, and phototherapy. Treatment with systemic therapy includes the use of insulin. The majority of treatment plans for DFUs address the altered biochemical composition of the diabetic ulcer while no single treatment have proven to be definitive for recommendation for the treatment of DFUs. Platelets are known to start the wound healing process through the release of locally active growth factors. PRP has been found to reduce inflammation and infection by the suppression of cytokine release and antimicrobial properties against several microorganisms. PRP has also been demonstrated to be of some antimicrobial properties against microorganisms, such as E. coli, MRSA, C. albicans, and C. neoformans. Although evidence supporting use of autologous PRP in wound healing is comparatively few, studies supporting its use in wound healing have increased during recent years. According to a study, treatment with PRP significantly increased the healing rate and over 86% of the patients who received PRP achieved complete healing in comparison to 68% who did not receive PRP treatment.[64] Another study reported that there was an increase in the likelihood of chronic wound healing, reduction in ulcer volume and time to complete healing, supporting the use of PRP for non-healing DFUs.[46,65] Some studies have reported the safety and efficacy of autologous PRP in DFU treatment.[66] A systematic review reported that PRP application, topically, for DFUs had resulted in higher healing rates and reduced the occurrence of complications in comparison to controls.[50]
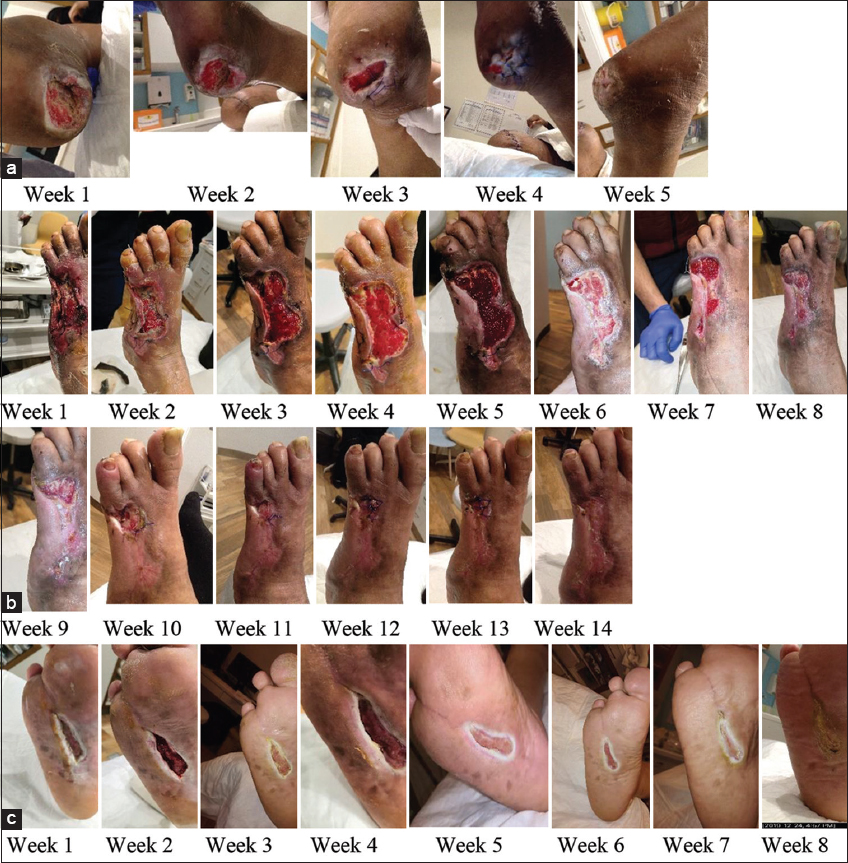
- (a-c) The following are some of the representative pictures of patients with chronic unhealed ulcers taken at the time of treatment initiation until ulcer closure
In the present case series, the treatment duration, from admission (to the amputation prevention clinic) to discharge (free of ulcer) varied from 3 to 14 weeks, and only 2–3 doses of autologous PRP were required for obtaining complete healing or maximum wound closure, supporting the previous studies showing efficacy of PRP in DFU treatment. The details about the treatments and duration of treatment of each case are presented in Table 2. This case series support other studies showing that PRP is an attractive and viable alternative treatment for managing chronic DFUs if adequate blood supply is maintained along with the use of suitable off loaders.[41,45,47] The strength of this study is that it is the first of its kind of study in Saudi Arabia, which has reported the benefits of PRP in chronic unhealed ulcers including diabetic ulcers. However, this case series was limited in term of sample size which is the number patients enrolled for the study. The sample size was very low to conclusively proclaim the benefits of PRP in speeding up the healing chronic ulcers, particularly of diabetic ulcers. Hence, this study warrants further study on a large number of sample to conclusively proclaim benefit of adding PRP to standard of care therapy for chronic ulcer healing particular of diabetic ulcers.
Conclusion
The present case series involving 14 cases of chronic unhealed ulcers, revealed that autologous PRP is efficacious in facilitating healing of ulcers supporting the findings of previous studies advocating the use of PRP as an attractive adjuvant therapy for the treatment of DFU’s and other types of chronic unhealed ulcers.
Consent to Participate
Written informed consent was obtained from all patients for anonymized patient information to be published in this article. A general consent form to publish patient information was obtained from all the patients before the study. At the time of informed consent being obtained from each participant, digital photographs were taken of the reference wound.
Conflict of Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Declaration
No data have been shared from this manuscript and no data were published in part or full elsewhere. The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
The authors acknowledge the services of professional medical writer in helping with the manuscript write up.
REFERENCES
- 2 Classification and diagnosis of diabetes:Standards of medical care in diabetes-2019 Diabetes Care. 2019;42:S13-28.
- Global estimates of undiagnosed diabetes in adults. Diabetes Res Clin Pract. 2014;103:150-60.
- [Google Scholar]
- 2016. Global Report on Diabetes. Geneva: World Health Organization; Available from: https://apps.who.int/iris/handle/10665/204871
- Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045 :Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843.
- [Google Scholar]
- Global prevalence of diabetes:Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047-53.
- [Google Scholar]
- Incidence of diabetes mellitus Type 2 complications among Saudi adult patients at primary health care center. J Phys Ther Sci. 2015;27:1727-30.
- [Google Scholar]
- Prevalence and risk factors for diabetes-related foot complications in translating research into action for diabetes (TRIAD) J Diabetes Complications. 2013;27:588-92.
- [Google Scholar]
- Literature review on the management of diabetic foot ulcer. World J Diabetes. 2015;6:37-53.
- [Google Scholar]
- Risk factors for recurrence of diabetic foot ulcers:Prospective follow-up analysis in the Eurodiale subgroup. Int Wound J. 2013;10:555-61.
- [Google Scholar]
- Incidence and risk factors of diabetic foot ulcer:A population-based diabetic foot cohort (ADFC Study)-two-year follow-up study. Int J Endocrinol. 2018;2018:7631659.
- [Google Scholar]
- Diabetes-related lower extremities amputations in Saudi Arabia:The magnitude of the problem. Ann Vasc Dis. 2012;5:1204160115.
- [Google Scholar]
- Lower limb amputations among diabetics admitted with diabetic foot disorders in three major hospitals in Jeddah, Saudi Arabia. J King Abdulaziz Univ. 2011;18:23.
- [Google Scholar]
- Extremities amputations in King Abdulaziz University Hospital (2005-2009) JKAU Med Sci. 2011;18:13-25.
- [Google Scholar]
- Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015;10:e0124446.
- [Google Scholar]
- Risk factors affecting the degree of diabetic foot ulcers according to Wagner classification in diabetic foot patients. Medi Clín Práct. 2021;4:100231.
- [Google Scholar]
- The frequency and risk factors of diabetic foot ulcer recurrence among Jordanian patients with diabetes. Curr Diabetes Rev. 2020;16:910-5.
- [Google Scholar]
- The risk of diabetic foot complication among Type 2 diabetes mellitus patients in Kendari City, Indonesia. Enferm Clín. 2021;31:S713-7.
- [Google Scholar]
- A systematic review of scoring systems for diabetic foot ulcers. Diabet Med. 2010;27:544-9.
- [Google Scholar]
- Risk of diabetic foot ulcer and its associated factors among Bangladeshi subjects:A multicentric cross-sectional study. BMJ Open. 2020;10:e034058.
- [Google Scholar]
- Brutsaert, Complications of Diabetes Mellitus. MSD Mannual Professional Version 2020. Available from: https://www.msdmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/complications-of-diabetes-mellitus
- [Google Scholar]
- Guidelines on the classification of diabetic foot ulcers (IWGDF 2019) Diabetes Metab Res Rev. 2020;36:e3273.
- [Google Scholar]
- Wagner's classification as a tool for treating diabetic foot ulcers:Our observations at a suburban teaching hospital. Cureus. 2022;14:e21501.
- [Google Scholar]
- Diabetic foot ulcer classifications:A critical review. Diabetes Metab Res Rev. 2020;36:e3272.
- [Google Scholar]
- Management of diabetic foot ulcers:Fed Pract. 2016;33:16-23.
- A retrospective analysis of amputation rates in diabetic patients:Can lower extremity amputations be further prevented? Cardiovasc Diabetes. 2012;11:18.
- [Google Scholar]
- The prevalence and incidence of diabetic foot ulcers among five countries in the Arab world:A systematic review. J Wound Care. 2017;26:S27-34.
- [Google Scholar]
- Economic impact of diabetic foot ulcers on healthcare in Saudi Arabia:A retrospective study. Ann Saudi Med. 2020;40:425-35.
- [Google Scholar]
- Diagnosis and Management of Diabetic Foot Complications. United States: American Diabetes Association; 2018.
- Diabetic foot ulcers:Current advances in antimicrobial therapies and emerging treatments. Antibiotics (Basel). 2019;8:193.
- [Google Scholar]
- Platelet-rich plasma:Support for its use in wound healing. Yale J Biol Med. 2010;83:1-9.
- [Google Scholar]
- Platelet rich plasma:A short overview of certain bioactive components. Open Med. 2016;11:242-7.
- [Google Scholar]
- Platelet-rich plasma for the treatment of chronic wounds:Evidence to date. Chronic Wound Care Manag Res. 2017;4:107-20.
- [Google Scholar]
- Mechanisms of Vascular Disease:A Reference Book for Vascular Specialists. Adelaide: University of Adelaide Press; 2011.
- Antimicrobial action of autologous platelet-rich plasma on MRSA-infected skin wounds in dogs. Sci Rep. 2019;9:12722.
- [Google Scholar]
- Role of platelet-rich plasma in healing diabetic foot ulcers:A prospective study. J Wound Care. 2018;27:550-6.
- [Google Scholar]
- Platelet-rich plasma for the treatment of diabetic foot ulcers:A meta-analysis. Wound Repair Regen. 2019;27:170-82.
- [Google Scholar]
- Role of platelet rich plasma in treatment of diabetic foot ulcers. Surg Sci. 2016;7:272.
- [Google Scholar]
- Effectiveness of autologous preparation rich in growth factors for the treatment of chronic cutaneous ulcers. J Biomed Mater Res B Appl Biomater. 2008;84:415-21.
- [Google Scholar]
- Topical application of platelet-rich plasma for diabetic foot ulcers:A systematic review. World J Diabetes. 2018;9:172-9.
- [Google Scholar]
- Autologous platelet-rich plasma treatment for patients with diabetic foot ulcers:A meta-analysis of randomized studies. J Diabetes Complications. 2020;34:107611.
- [Google Scholar]
- Emerging evidence for neuroischemic diabetic foot ulcers:Model of care and how to adapt practice. Int J Low Extrem Wounds. 2009;8:82-94.
- [Google Scholar]
- Current and emerging therapies in the management of diabetic foot ulcers. Curr Med Res Opin. 2016;32:519-42.
- [Google Scholar]
- Debridement of diabetic foot ulcers. Cochrane Database Syst Rev. 2010;2010:CD003556.
- [Google Scholar]
- The impact of topical agents and dressing on pH and temperature on wound healing:A systematic, narrative review. Int Wound J. 2021;19:1397-408.
- [Google Scholar]
- A pilot study on the effects of a polyherbal formulation cream on diabetic foot ulcers. Indian J Med Res. 2011;134:168-73.
- [Google Scholar]
- Management of diabetic foot ulcers using topical oxygen therapy:A case series. Curr Diabetes Rev. 2022;18:e051021196984.
- [Google Scholar]
- Growth factors for diabetic foot ulcers:Mixed treatment comparison analysis of randomized clinical trials. Br J Clin Pharmacol. 2018;84:434-44.
- [Google Scholar]
- Role of growth factors and cytokines in diabetic foot ulcer healing:A detailed review. Rev Endocr Metab Disord. 2019;20:207-17.
- [Google Scholar]
- Diabetic foot ulcers and epidermal growth factor:Revisiting the local delivery route for a successful outcome. Biomed Res Int. 2017;2017:2923759.
- [Google Scholar]
- Fibroblast growth factor in diabetic foot ulcer:Progress and therapeutic prospects. Front Endocrinol (Lausanne). 2021;12:744868.
- [Google Scholar]
- Epidermal growth factor in healing diabetic foot ulcers:From gene expression to tissue healing and systemic biomarker circulation. MEDICC Rev. 2020;22:24-31.
- [Google Scholar]
- Platelet-rich plasma for the treatment of clean diabetic foot ulcers. Ann Vasc Surg. 2017;38:206-11.
- [Google Scholar]
- Platelet-therapeutics to improve tissue regeneration and wound healing-physiological background and methods of preparation. Biomedicines. 2021;9:869.
- [Google Scholar]
- Platelet-rich plasma for the treatment of diabetic foot ulcer:A randomized, double-blind study. Egypt J Surg. 2018;37:178-84.
- [Google Scholar]







