Translate this page into:
Color and flexural properties of nanoparticles-modified denture base resin: An in vitro comparative study
Address for correspondence: Dr. Mohamed Ahmed Helal, Department of Prosthodontics, Faculty of Dental Medicine, Al-Azhar University, Cairo, Egypt. Phone: +2022629412. E-mail: mhelal@azhar.edu.eg
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
ABSTRACT
Objectives:
Reinforcement of polymethylmethacrylate (PMMA) denture base resins (DBRs) with inorganic fillers with superior properties and accepted aesthetics are favored and still a big dilemma. This study was undertaken to evaluate the color change, flexural strength, and modulus of elasticity of heat-polymerized DBR material modified with silver nanoparticles (AgNPs) and zirconium dioxide nanoparticles (ZNPs).
Methods:
Sixty acrylic specimens (30/color test, 30/flexural properties) were fabricated and divided according to nanoparticles type and addition into 3 groups (n = 10). Group-I; unmodified specimens, Group-II; modified specimens with 0.5wt% AgNPs (PMMA/AgNPs), and Group-III; modified specimens with 7.5wt% ZNPs (PMMA/ZNPs). Disc-shape (20 × 3 mm) and bar-shape (65 × 10 × 2.5 mm) specimens were fabricated for color and flexural properties, respectively. The spectrophotometer was used for evaluation of the color change (∆E). The flexural strength and elastic modulus evaluation was carried out using a 3-point bending test (5 mm/min). Tukey’s post hoc and one-way ANOVA were used to analyze the data at a significant level P ≤ 0.05.
Results:
PMMA/AgNPs group exhibited a significant increase in color change when compared with PMMA/ZNPs. PMMA/ZNPs showed significantly the highest flexural strength value when compared with unmodified and PMMA/AgNPs groups (P < 0.001), however, there was an absence of significant differences in terms of flexural strength values between PMMA/AgNPs and unmodified groups (P > 0.05). PMMA/AgNPs insignificantly increased its modulus of elasticity strength (P = 0.09410) while PMMA/ZNPs significantly increased its modulus of elasticity strength (P = 0.00396).
Conclusion:
The AgNPs and ZNPs addition to PMMA increased the color change and AgNPs change the color of DBRs. The flexural attributes of DBRs have been increased by ZNPs.
Keywords
Color change
denture base
mechanical testing
nanoparticles
polymethylmethacrylate
Introduction
Completely or partial removable dental prosthesis having acrylic denture bases that provide the support for the prosthesis and carry the artificial teeth.[1,2] Polymethyl-methacrylate (PMMA) has become the most broadly used material for the manufacture of denture-base because its moderate cost, has good esthetic appearance, light in weight, easy of processing, and chemically stable.[1,3] However, its poor mechanical properties can lead to denture base fracture.[1,4,5] After many years of wearing removable dentures, the denture base is weakened by persistent stress caused by poor denture fit and occlusion, which can lead fracture of the denture base.[6]
The characteristics of denture-based PMMA have been improved by many attempts either through chemical composition modifications or additives (macro-, micro-, or nano-fillers).[5,7-9] Inorganic nanoparticles (NPs) are one category of additive that has been suggested to be incorporated into PMMA and broadly investigated aiming to improve its properties.[10-12] NPs have many unique properties due to nano-size, large surface area to mass ratio, thermal stability, and high reactivity with other materials.[9] The properties of a polymer/nanocomposite mixture are determined by the size and the concentration as well as the interaction of these NPs with the matrix of the polymer matrix.[13] Many types of NPs as zirconia, zinc, titanium, gold, and silver had been developed and used in the dental field for the antimicrobial activity and to improve physical and mechanical properties.[8,14-17]
Silver NPs (AgNPs) are commonly used to strengthen several dental materials due to their unique physical and mechanical properties, biocompatibility with human tissues, and antimicrobial activities.[18-21] Hence, incorporating AgNPs into heat-polymerized denture base materials to improve the physico-mechanical properties was suggested.[19,22] Denture base resins (DBRs) containing AgNPs showing a decrease in microbial adhesion and colonization and generally enhance the overall oral health.[19,23-26] Also adding 2.5% AgNPs having an antimicrobial effect but, when the concentration increased above 2.5% affects the properties of heat-polymerized DBRs.[19,23-26] Therefore, low concentrations were recommended in terms of mechanical performance.[19,23-26]
Recently, zirconia NPs (ZNPs) received great attention due to its white color and good biocompatibility. It possesses better surface as well as biological properties thus making the ZNPs a beneficial material in reinforcement of the most materials used in the dental field.[5,11,27] In terms of ZNPs concentrations, Zidan et al. added ZNPs ranging from 1.5% to 10% and concluded that high mechanical performance was reported with high concentrations.[28] In addition, previous studies[11,29] reported that adding 7.5% ZNPs to the denture-base resin led to an increase in tensile and flexural strengths.
Although many researchers have been studied the impact of adding different NPs on the attributes of DBR materials, still more data regarding the effect of adding AgNPs and AgNPs on color change and flexural properties of DBR are required. Therefore, the primary objective of this in vitro study was to evaluate and compare the effect of AgNPs and ZNPs incorporation on the color change, flexural strength, and modulus of elasticity of DBR. The null hypothesis stated that there is no change in color and no effect on flexural properties of AgNPs and ZNPs modified heat-polymerized DBRs.
Materials and Methods
Based on the previous studies, a total of 60 specimens (n = 10) were required to carry out the current in vitro study.[29] The samples of heat/polymerized denture base acrylic resin were prepared in accordance with plates were fabricated in dimensions per respective test, each of them was milled into disk forms with 20 mm diameter and thicknesses of 3 mm for color test and 65 × 10 × 2.5 mm for flexural properties test.
Materials used in the present study
The materials that throughout the current study used were the heat-polymerized denture base acrylic resin (Vertextm Rapid simplified), AgNPs with a concentration of 0.5wt% and ZNPs with a concentration of 7.5 wt% (Nano-gate Company, Egypt). Sixty specimens were constructed and divided into 3 groups (n = 20; 10/color test and 10/flexural properties test): Group I: contained 20 specimens of heat/polymerized denture base acrylic resin. Group II: contained 20 heat/polymerized denture base acrylic resin modified with 0.5 wt % AgNPs. Group III: contained 20 specimens of heat/polymerized denture base acrylic resin modified with 7.5 wt.% ZNPs.
NPS and mixtures preparation
The treatment of AgNPs and ZNPs silane coupling agent to create reactive groups on the surface to provide good bonding between NPs and the matrix of the resin, and to guarantee that this material would evenly coat the NPs surface; 0.3 mg of silane coupling agent was dissolved in 100 mL of acetone. 30 g of NPs (AgNPs or ZNPs) were added to the solution which formed from mixing of silane coupling agent and acetone and stirred using the magnetic stirrer followed by evaporation using a rotary evaporator and then dried. The silanization process was completed following previous studies.[3,30] The treated AgNPs were measured using an electronic analytical balance device (Sartorius; AG; Germany), and added in concentration of 0.5 wt.% into the PMMA powder. With the same manner, treated ZNPs were measured with the same device and added in a concentration of 7.5 wt.% into the PMMA powder. Each modified powder was stirred with an electric-mixer at a rotating speed of 400 rpm at room temperature for 30 s to obtain a homogenous mixture with an equal distribution of the NPs.
Specimens processing
Each stainless-steel pattern was used for the fabrication of the specimens using the conventional processing technique of heat/polymerized denture base acrylic resin.[31] After that, a tungsten carbide bur was used to trimming of the specimens to eliminate any remaining small scratches, finished and polished in a conventional manner, and then stored by keeping in distilled water at 37°C for 48 h.
Color measurement
The assessment of the color change was carried out using a Spectrophotometer device (X-Rite; model RM200QC; Neu-Isenburg; Germany). The discs color from each main group were assessed (3 times/disc) on the scale of the CIE-Lab. The color difference between specimens was detected using (ΔΕ* = [(ΔL*)2 +(Δa*)2 + (Δb*)2]1/2). For clinical assessment of color change, ΔΕ value was transformed to the NBS units with the help of the following equation: NBS Unit = ΔΕ × 0.92.[32]
Flexural properties
The flexural properties were assessed using a universal testing machine and a 3-point bending test. Specimens were placed horizontally on two metal supports 50 mm distance apart and then the load (5 KN) was applied at the center of specimens with crosshead speed of 5 mm/min till specimen failure recording the force at fracture (N). The flexural properties were calculated using the following formulas: (S=3FI/2bh2) and (E= FI3/4bh3d) where;
S: is flexural strength (MPa),
F: is maximum load at the moment of fracture (N),
b: is width and h: thickness (mm) of specimen, and
E: is Modulus of Elasticity (GPa),
l: is distance between the supports,
d: is deflection.
Statistical analysis
Descriptive analyses were performed using means and standard deviations (SD). Shapiro–Wilk test was used for results normality and revealed normal data distribution so the parametric test was used for data analysis. The statistical data underwent analysis through a one-way ANOVA test, subsequently followed by Tukey’s post hoc test for pairwise comparison. The significance level was set at P < 0.05, and the statistical software utilized was SPSS ® Statistics Version 20.
Results
Standard deviation (SD) in color change (∆E) of NPs-modified groups and mean values are shown in Table 1. One-Way ANOVA test indicated that there was a significant difference between different tested groups, also the comparison in pairs using Tukey’s post hoc test showed significant differences between tested groups. The incorporation of AgNPs and ZNPs markedly increases the color change of heat-polymerized PMMA specimens. PMMA/AgNPs group resulted in marked increase in color change (∆E = 24.64 ± 2.54) when compared with PMMA/ZNPs (∆E = 4.19 ± 0.37). According to NBS classification, PMMA/ZNPs resulted in NBS values with a range of (3.33–4.20) which means marked color alteration in the heat-cured acrylic base denture resin. While the incorporation of PMMA/AgNPs resulted in NBS values with range of (20.90–26.45) which means a change of the color of heat-polymerized PMMA specimens to other colors.
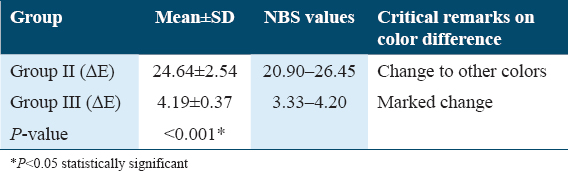
Table 2 and Figure 1 show the mean values, SD, and significance of flexural strength (MPa) results for all tested groups. The difference between all tested groups was statistically significant as indicated by one-way ANOVA test (F = 24.947, P < 0.001). In comparison to unmodified group, PMMA/AgNPs showed non-significant increase in flexural strength (P = 0.05293) while PMMA/ZNPs significantly increased its flexural strength (P < 0.001). Where PMMA/ZNPs showed the highest flexural strength (124.04 ± 7.07 MPa); followed by PMMA/AgNPs (107.61 ± 6.74 MPa) while the least value of flex strength was (98.30 ± 6.88 MPa) which was recorded in PMMA group.
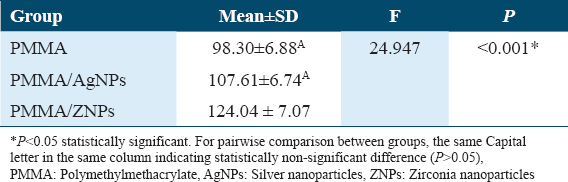
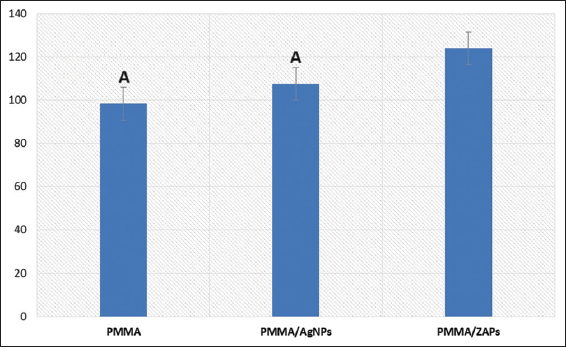
- Comparison of flexural strength (MPa) test results among tested groups. Same letter indicating statistically non-significant difference (P > 0.05)
The average values, SD, and significance of modulus of elasticity (GPa) results for all tested groups are listed in Table 3 and Figure 2. One-way ANOVA test indicated that there was a significant difference between all tested groups (F = 7.1201, P = 0.00527). PMMA/ZNPs group showed the highest modulus of elasticity (3.70 ± 0.34 GPa); followed by PMMA/AgNPs (3.48 ± 0.26 GPa) while the unmodified group showed the lowest value (3.14 ± 0.22 GPa). PMMA/AgNPs insignificantly increased its modulus of elasticity strength (P = 0.09410) while PMMA/ZNPs significantly increased its modulus of elasticity strength (P = 0.00396). Tukey’s post hoc test showed non-significant difference (P > 0.05) between unmodified group versus PMMA/AgNPs group and PMMA/ZNPs versus PMMA/AgNPs group.
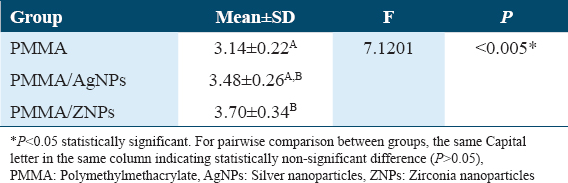
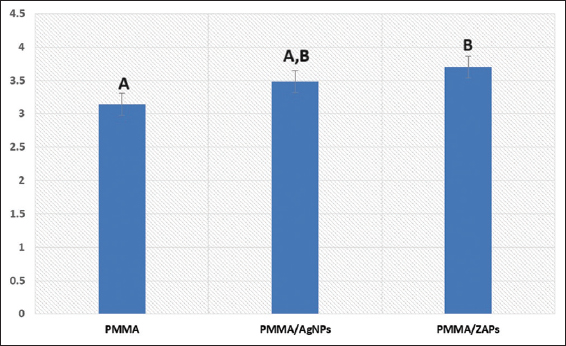
- Comparison of modulus of elasticity (GPa) test results among tested groups. The same letter indicating a statistical difference which is non-significant (P > 0.05)
Discussion
In this study, two different NPs were selected in concentrations (0.5wt.% AgNPs and 7.5wt.% ZNPs) and showed appropriate mechanical performance to be compared in terms of mechanical and esthetic demands. Previous studies reported that these concentrations can be used to decrease the possible unfavorable alterations in the visual and mechanical characteristics of the heat-polymerized denture acrylic base. In addition to that these concentrations are non-toxic and biocompatible.[12,33] The results of the presented study indicated that the addition of both NPs affects the color and ZNP increase the flexural properties while AgNPs had not a significant effect on the flexural properties. Therefore, the null hypothesis was partially rejected.
The powder of PMMA heat-polymerized acrylic-based resin is available in a pink shade, when it is mixed with a monomer solvent and undergoes a heat-cured setting reaction.[34] Color instability is considered as one of the great problems that encountered after reinforcement of the PMMA heat-polymerized acrylic resin with NPs. The alteration of the color prosthesis may lead to aesthetic problems and patient dissatisfaction and may affect finally the acceptance of the prosthesis.[32,35] NBS measurable factors are important to correlate the amount of the color alteration and its quality to the clinical environment[36,37] and for the color comparisons.[38] So in the present study the color alteration values (ΔE) were transformed to the values of NBS and their clinical validities were evaluated.
The observed NBS values were respectively (24.64 and 4.19) for the PMMA/AgNPs and PMMA/ZNPs in the tested samples, these values were out of the clinically accepted limits. The expression of color difference using NBS rating system indicates that the PMMA/AgNPs reveal change to other color while, the PMMA/ZNPs exhibited a marked change in color.[39,40] The difference in the refractive index of filler and matrix affects the reflection and refraction at the filler-matrix interface which changes the translucency of modified material (PMMA/AgNPs or PMMA/ZNPs).[41] Since inorganic NPs and resin are present in this modified material, the opacity of the modified material will increase with increase in difference between the refractive index of the two phases.[11,29,42] The refractive index of ZNPs (2.1750) was found to be higher than that of the PMMA (1.4813).[43] It was found that the AgNPs, have a high-negative effective refractive index (0.135), and the change in color of the PMMA/AgNPs specimens into brownish color. Therefore, ZNPs could be used in concentrations <7.5% while for AgNPs caution with addition and concentration selection must considered. If both NPs indicated to attain nanocomposites with improved mechanical properties and have antifungal activities[44] and at the same time has no adverse effect on esthetics, it could be added in unaesthetic areas or added in the doubling layer technique reported in previous studies.[3,45]
After using the denture for many years, it loses its adaptation to the underling tissue, this denture mal-adaptation increases the exposure to excessive transverse stresses, especially during mastication.[46,47] The mid-line of the upper denture is the most common site of fracture. Furthermore, the modulus of elasticity is the other property that has an important effect in the assessment of the properties of the PMMA denture base in addition to the flexural strength.[32] As the modulus of elasticity is the withstanding ability of the material against non-permanent or elastic deformation.[48] Hence, in this study; 3-point bending test was performed for the purpose of attaining flexural properties values.
Hence the denture base is exposed to continuous transverse deformation during functional movements,[49] nanocomposite DBRs with high fracture resistances were suggested.[50] These nanocomposites are formed by the addition of NPs into resin matrix. However, the good adhesion and bonding between rein matrix and added NPs are required.[51,52] In the present study, NPs treated with a silane coupling agent to improve the bonding, dispersion of NPs within the resin matrix, and decrease the chance of NPs aggregation and cluster formation and eventually led to new nanocomposite with enhanced properties.[53]
Per the ISO 20795-1 standard, DBRs require minimum thresholds of 65MPa for flexural strength and 2GPa for modulus of elasticity. In our study, the average flexural strength and modulus of elasticity across all tested groups surpassed these clinically acceptable limits. The incorporation of ZNPs and AgNPs resulted in notable enhancements in both flexural strength and modulus of elasticity. Particularly, ZNPs exhibited a significant increase, while AgNPs showed a comparatively less significant effect. This observed improvement can be attributed to the high surface area of the NPs, enabling efficient stress transfer from the matrix to the NPs. This transfer effectively enhances the mechanical properties of the material.[23] In addition, the formation of polar interactions, especially between the (C=O) group of PMMA chains and NPs, promotes better compatibility between the polymeric matrix and the NPs.[23,54] However, the less significant impact of AgNPs may be linked to their lower concentration and inadequate dispersion within the matrix.[23]
The findings of the current study were in agreement with previous studies[30,55] that reported an increase in the flexural strength of PMMA denture base by adding ZNPs. This is attributed to the distribution within the resin material and the inherent property of ZNPs which is called the transformation toughening.[30] Through the mechanism involving the transformation of ZrO2 from its tetragonal to monoclinic phase, it absorbs the energy associated with crack propagation. This ability of ZNPs serves to impede the propagation of cracks.[33] Simultaneously, the expansion of ZrO2 crystals during this process induces a state of compressive stress within the crack. This stress contributes to halting the progression of the crack, thereby enhancing the fracture resistance of nanocomposites compared to their unmodified counterparts.[23,30]
AgNPs were added mainly due to their antimicrobial effectiveness and showed some improvement in mechanical properties.[12,18,19,21] This effect was concentration dependent[12,19,22] and the insignificant increase may be due to low concentrations. However, the low concentrations of AgNPs used, the color change (brownish nanocomposite) limits its use in high concentrations, especially in the esthetic zone. Therefore, AgNPs addition clinically affect the esthetic outcome, and the area where it to be added consecrations must considered. On the other side, PMMA/ZNPs is whitish but improve the mechanical properties when it added in 7.5%. It was reported that 5%ZNPs also showed high mechanical properties.[27,28] Therefore, ZNPs could be added in concentration <7.5% and at the same time may be decrease the color change to be within clinical acceptable value.[29] Therefore, further studies were recommended with the using of different concentrations of AgNPs and ZNPs to assure the proper concentration which could improve the mechanical properties of PMMA/AgNPs composite and PMMA/ZNPs composite without affecting the color of PMMA resin.
Using only one DBR and one concentration per NPs add limitations to the in-vitro study limitations. In addition to testing specimens shape not mimic denture configuration and absence of oral environments. Therefore, more studies with different concentrations and different DBRs are recommended to be tested in-vivo or in conditions simulating oral condition with aging are recommended.
Conclusion
The addition of AgNPs and ZNPs to PMMA denture base resulted in a dramatic color change from pink to whitish with ZNPs and changed from pink to grayish color with AgNPs. The addition of ZNPs PMMA acrylic resin resulted in increase of the flexural properties of PMMA denture base materials. The incorporation of AgNPs into PMMA acrylic resin has no significant effect on the flexural properties of PMMA denture base materials.
Authors’ Contributions Statement
-
Study design and conducting experiments (Abdel-Naser M. Emam, Karim-Eldin Ibrahim Ahmed, Adel M. Shaaban, Mohamed Ahmed Helal)
-
Data collection and data analysis (Karim-Eldin Ibrahim Ahmed, Adel M. Shaaban)
-
Manuscript drafting and reviewing (Abdel-Naser M. Emam, Mohamed Ahmed Helal, Mohammad Abdullah Alqhtani, Mohammed M. Gad)
-
Final editing and reviewing (Abdel-Naser M. Emam, Mohamed Ahmed Helal, Mohammed M. Gad)
-
All authors read and approved the final manuscript.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval Statement
Not applicable
References
- Conventional and contemporary polymers for the fabrication of denture prosthesis:Part I - overview, composition and properties. Int J Appl Dent Sci. 2015;1:82-9.
- [Google Scholar]
- Physical properties of polyamide-12 versus PMMA denture base material. Biomed Res Int. 2014;2014:150298.
- [Google Scholar]
- Double-layered acrylic resin denture base with nanoparticle additions:An in vitro study. J Prosthet Dent. 2022;127:174-83.
- [Google Scholar]
- PMMA denture base material enhancement:A review of fiber, filler, and nanofiller addition. Int J Nanomed. 2017;12:3801-12.
- [Google Scholar]
- Incorporation of antimicrobial macromolecules in acrylic denture base resins:A research composition and update. J Prosthodont. 2014;23:284-90.
- [Google Scholar]
- Overview of incorporation of inorganic antimicrobial materials in denture base resin:A scoping review. J Prosthet Dent. 2021;130:202-11.
- [Google Scholar]
- Effect of zirconium oxide nanoparticles addition on the optical and tensile properties of polymethyl methacrylate denture base material. Int J Nanomedicine. 2018;13:283-92.
- [Google Scholar]
- Antibacterial effects of a new dental acrylic resin containing silver nanoparticles. J Appl Polym Sci. 2008;110:1699-703.
- [Google Scholar]
- Experimental trends in polymer nano composites - a review. Mater Sci Eng. 2005;393:1-11.
- [Google Scholar]
- Nanoparticle-modified PMMA to prevent denture stomatitis:A systematic review. Arch Microbiol. 2021;204:75.
- [Google Scholar]
- The impact of nanoparticles-modified repair resin on denture repairs:A systematic review. Jpn Dent Sci Rev. 2021;57:46-53.
- [Google Scholar]
- An in vitro comparison of the fracture resistance of standard and modified mesio-occluso-distal cavity designs restored with resin composite restoration. Int J Health Sci (Qassim). 2018;12:26-30.
- [Google Scholar]
- Cutting efficiency of different dental materials utilized in an air abrasion system. Int J Health Sci (Qassim). 2017;11:23-7.
- [Google Scholar]
- Silver nanoparticles as a new generation of antimicrobials. Bio Technol Adv. 2009;1:76-83.
- [Google Scholar]
- In vitro comparison of compressive and tensile strengths of acrylic resins reinforced by silver nanoparticles at 2% and 0.2% concentrations. J Dent Res Dent Clin Dent Prospect. 2014;8:204-9.
- [Google Scholar]
- Silver nanoparticles as antimicrobial agent:A case study on E. coli as a model for Gram-negative bacteria. J Colloid Interface Sci. 2004;275:177-82.
- [Google Scholar]
- Effects of silver nanoparticle-based antimicrobial formulations on the properties of denture polymer:A systematic review and meta-analysis of in vitro studies. J Prosthet Dent. 2023;129:310-21.
- [Google Scholar]
- Effect of silver nanoparticles on flexural strength of acrylic resins. J Prosthodont Res. 2012;56:120-4.
- [Google Scholar]
- Effect of nanosilver on thermal and mechanical properties of acrylic base complete dentures. J Dent (Tehran). 2014;11:495-505.
- [Google Scholar]
- Antimicrobial and mechanical properties of acrylic resins with incorporated silver-zinc zeolite - part I. Gerodontology. 2008;25:187-94.
- [Google Scholar]
- Antifungal and physical characteristics of modified denture base acrylic incorporated with silver nanoparticles. Gerodontology. 2012;29:e413-9.
- [Google Scholar]
- The effect of zirconium dioxide (ZrO2) nanoparticles addition on the mechanical parameters of polymethyl methacrylate (PMMA):A systematic review and meta-analysis of experimental studies. Polymers (Basel). 2022;14:1047.
- [Google Scholar]
- Investigating the mechanical properties of ZrO2-impregnated PMMA nanocomposite for denture-based applications. Materials (Basel). 2019;12:1344.
- [Google Scholar]
- Polymethylmethacrylate-based nanocomposites for denture base fabrication:Impact of nanoparticle type and concentration on the color change in vitro. Int J Dent. 2023;2023:4245801.
- [Google Scholar]
- Influence of incorporation of ZrO2 nanoparticles on the repair strength of polymethyl methacrylate denture bases. Int J Nanomedicine. 2016;11:5633-43.
- [Google Scholar]
- Dentistry-Base Polymers BS EN ISO 20795-1:2008. London, UK: British Standards Institution (BSI); 2008. p. :36.
- The assessment of some physical and mechanical properties of PMMA added different forms of nano-ZrO2. J Dent Oral Health. 2017;3:64-74.
- [Google Scholar]
- Effect of zirconium oxide nanofillers addition on the flexural strength, fracture toughness, and hardness of heat- polymerized acrylic resin. World J Nano Sci Eng. 2014;4:50-7.
- [Google Scholar]
- Translucency evaluation of polymethyl methacrylate (PMMA) reinforced with ZrO2-Al2O3-SiO2 filler system in fabricating indirect restoration. UIP Health Med. 2016;1:1-7.
- [Google Scholar]
- Color stability of heat and cold cure acrylic resins. J Clin Diagn Res. 2015;9:5-12.
- [Google Scholar]
- Color stability of silicone or acrylic denture liners:An in vitro investigation. Eur J Dent. 2007;1:144-51.
- [Google Scholar]
- Effects of fibers on the color change and stability of resin composites after accelerated aging. Dent Mater J. 2012;31:872-8.
- [Google Scholar]
- Influence of denture cleansers on the color stability of three types of denture base acrylic resin. J Prosthet Dent. 2009;101:205-13.
- [Google Scholar]
- The effects of adding various ratios of zirconium oxide nanoparticles to poly (methyl methacrylate) on physical and mechanical properties. J Oral Sci. 2018;60:304-15.
- [Google Scholar]
- Color change in acrylic resin processed in three ways after immersion in water, cola, coffee, mate and wine. Acta Odontol Latinoam. 2013;26:183-93.
- [Google Scholar]
- Light transmission characteristics of dentine and resin composites with different thickness. J Dent. 2012;40:77-82.
- [Google Scholar]
- Influence of different beverages on the color stability of nanocomposite denture base materials. Int J Dent. 2021;2021:5861848.
- [Google Scholar]
- Microbiological evaluation for antifungal activity of some metal oxides nanofillers incorporated into cold cured soft lining materials:Clinical based study. Braz Dent Sci. 2022;25:e2921.
- [Google Scholar]
- Polymethylmethacrylate denture base layering as a new approach for the addition of antifungal agents. J Prosthodont. 2023;32:298-308.
- [Google Scholar]
- Comparative study of the flexural strength of high impact denture base resins reinforced by silver nanoparticles and e-glass fibers:An in-vitro study. J Clin Diagn Res. 2018;12:ZC22-6.
- [Google Scholar]
- Craig's Restorative Dental Materials. Philadelphia, PA: Mosby Publishers; 2011.
- Flexural and fatigue strengths of denture base resin. J Prosthet Dent. 2008;100:47-51.
- [Google Scholar]
- Comparative effect of incorporation of ZrO2, TiO2, and SiO2 nanoparticles on the strength and surface properties of PMMA denture base material:An in vitro study. Int J Biomater. 2022;2022:5856545.
- [Google Scholar]
- Impact of nanoparticles additions on the strength of dental composite resin. Int J Biomater. 2022;202:1165431.
- [Google Scholar]
- Color stability of nanoparticles-modified dental resin-based composites. Appl Sci. 2023;13:3870.
- [Google Scholar]
- Influence of silver nanoparticles incorporation on flexural strength of heat-cure acrylic denture base resin materials. Ann Res Rev Biol. 2017;17:1-8.
- [Google Scholar]
- Effect of reinforcement of high impact acrylic resin with micro-zirconia on some physical and mechanical properties. Rev Clin Pesq Odontol Curitiba. 2008;4:145-51.
- [Google Scholar]







