Translate this page into:
Comparative evaluation of clinical attachment and alveolar bone levels in patients with infrabony pockets treated by conventional and microsurgical approach – a randomized clinical trial
Address for correspondence:Dr. Subash Chandra Raj, Department of Periodontics, SCB Dental College and Hospital, Cuttack, Odisha, India. Phone: +9437008298. E-mail: drsubash007@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
ABSTRACT
Objectives:
The aim of the present study is to evaluate and compare healing outcomes, probing pocket depth (PPD) reduction, clinical attachment, and alveolar bone level following Modified Widman Flap (MWF) with and without 4× prismatic loupe in infrabony pockets.
Methods:
Patients having at least one infrabony pocket with PPD ≥5 mm and angular bone loss ≥3 mm bilaterally were randomly assigned to a microsurgical (test) group with MWF using 4× magnifying loupes and conventional (control) group by MWF only. At baseline, 3 and 6 months plaque index, bleeding index, PPD, and relative clinical attachment level were taken. The healing outcome was evaluated with a healing index by Landry. Pain score was assessed with Visual Analog Scale (VAS). The percentage of defect depth (DD) reduction was assessed by cone beam computed tomography (CBCT) and periapical radiograph. Continuous data between groups were analyzed using an unpaired “t” test. Within-group comparison was done using repeated measures analysis of variance followed by multiple pairwise comparisons and paired “t” test.
Results:
There was a statistically significant (P = 0.004) reduction in intrabony DD in each group evaluated through CBCT. The mean VAS score after 1 week of surgical procedure was 3.67 at the conventional site compared to 2.9 at the microsurgical site, which was statistically significant (P = 0.004). Statistically significant (P ≤ 0.05) healing scores were observed for microsurgery group (84.6% after 1 week) compared to control group (15.4% after 1 week).
Conclusion:
Although blinding of patients and surgeons was difficult and healing indices used are subjective, it can be concluded that microsurgery under 4× magnifying loupe is as effective as conventional MWF in the treatment of infrabony pockets but clinical parameters are greatly enhanced by microsurgery with improved healing and less patient discomfort.
Keywords
Conventional surgery
infrabony pocket
microsurgery
modified Widman flap
prismatic loupes
Introduction
Periodontitis is a multifactorial chronic inflammatory disease that leads to clinical attachment loss, periodontal pocket formation, gingival recession, alveolar bone loss resulting in tooth mobility and further its loss.[1] The gold standard in treating periodontal disease is the removal of plaque and calculus from the tooth surface.[2] “Closed” (subgingival scaling and root planing) and “Open” (surgical) methods are used for the treatment of periodontitis.[3] Treatment done through flap procedures have been used mainly for three purposes: surgical elimination/reduction of periodontal pockets, to induce reattachment, new attachment and bone regeneration, and to correct gingival and mucogingival defects and deficiencies.[4] Modified Widman flap (MWF) remains the standard surgical procedure among various periodontal surgical techniques that include precise incisions, minimal flap exposure, and complete debridement.[5,6] It still remains the most sought after surgical procedure for pocket therapy as it establishes an intimate post-operative adaptation of collagenous connective tissue to the tooth surface thereby resulting in pocket reduction.[5] Conventional surgical technique is often based on large, beveled incisions, and reflection of large mucoperiosteal flaps which causes bone exposure and the results were unsatisfactory due to limited regenerated periodontal tissue.[7,8]
Periodontal microsurgery is the improvement of standard surgical techniques by the increased visual acuity with the help of a surgical microscope. There are three benefits which comes under the microsurgical triad: illumination, magnification, and increased precision in surgical skills.[9] Less trauma to the tissues, excellent flap control, and proper suturing technique help in achieving primary wound closure.[10,11] Prismatic magnifier produces a larger field of view, greater depth of field, longer working distance, and higher magnification compared to other magnifying loupes. Loupes with a magnification of <4× are generally unsuitable for periodontal microsurgery.[12]
Conventional MWF includes large incisions with a reflection of large mucoperiosteal flaps, increases the chance of trauma to tissues, flap control may be difficult, and proper suturing may not be achieved.[7,8] These factors can be well taken care of by microsurgery because of magnification, illumination, and increased precision in surgical skills. An approach to access the intra-bony defects by Harrel used minimal incisions for debridement and involved papilla reflection to access the intra-bony defect using specialized instruments. The majority of periodontal procedures done under 4× to 5× magnifiers having an effective combination of magnification, an optimal field of view size, and depth of field provide higher visual acuity. As of today, there is hardly any randomized controlled trial comparing the effectiveness of 4× magnifying loupes and MWF in treating patients with infrabony pockets.[12] Hence, the aim of the present study is to compare and evaluate the gain in clinical attachment and alveolar bone levels in patients with infrabony pockets treated by MWF using a conventional approach to that of microsurgical approach with 4× magnifying loupes.
Materials and Methods
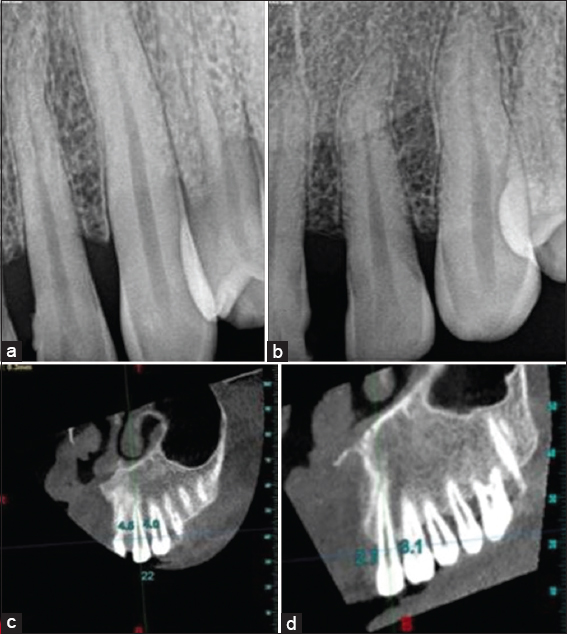
This single-center, split-mouth randomized controlled trial was performed from March 2020 to January 2022, in the Department of Periodontics, SCB Dental College and Hospital, Cuttack, Odisha. The subjects in the study completed and signed a written informed consent form to participate in the study. This study followed the ethical guidelines of the Helsinki Declaration 1964 as revised in 2013[13] and was recommended under the institutional ethics committee (IEC), SCB Dental College and Hospital, Cuttack, Odisha (IEC/SCBDCH/072/2020 dated March 11, 2020). This study is registered at ClinicalTrials.gov (CTRI ID: CTRI/2020/06/025724). The study population (sampling frame) was selected based on pre-defined inclusion and exclusion criteria, irrespective of gender and religion is as follows:
Inclusion criteria
-
Age ≥25 years
-
At least one infrabony pocket with probing pocket depth (PPD) >5 mm bilaterally or in both arches
-
Vertical/angular bone loss >3 mm
-
Adequate width of attached gingiva
-
Plaque index <2.
Exclusion criteria
-
Previous periodontal surgery within the past 6 months in an area of interest
-
Systemic conditions which are contraindications to periodontal surgery
-
Pregnant or lactating females
-
Current or former smokers
-
Hopeless tooth.
On initial examination, all selected subjects underwent scaling and root planing and were recalled after 4 weeks. Based upon the compliance and residual probing pocket depth >5mm, the subjects were selected for the study. Patient consent statements were taken. A stent was customized and fabricated that acted as a fixed reference point from cementoenamel junction (CEJ) to the base of the sulcus/pocket for vertical measurements at baseline and all subsequent follow-up periods. All baseline clinical parameters [Plaque index (PI),[14] modified sulcus bleeding index (mSBI),[15] PPD, relative clinical attachment level (RCAL),[16] healing index (HI),[17] Visual Analog Scale (VAS)[18] were made by a calibrated and blinded examiner and baseline radiological parameters (Intraoral periapical [IOPA] and cone beam computed tomography [CBCT]) were recorded before the surgery. HI by Landry was evaluated for 3 weeks by using parameters of tissue color, bleeding response to palpation, presence of granulation tissue, characteristics of incision margins, and presence of suppuration.[17] VAS was assessed for 1 week using a scale from 0 to 10 where 0 depicted no pain, 1–3 meant mild pain, 4–6 for moderate pain, 7–9 for very severe pain, and 10 depicted worst pain.[18] Defect depth (DD) and percentage of DD reduction were assessed by CBCT and periapical radiograph. The clinical parameters were recorded again at 3rd and 6th months after surgery for each subject. This study adhered to the standardized CONSORT reporting guidelines.
Radiographic assessment of intrabony defects (IBDs)
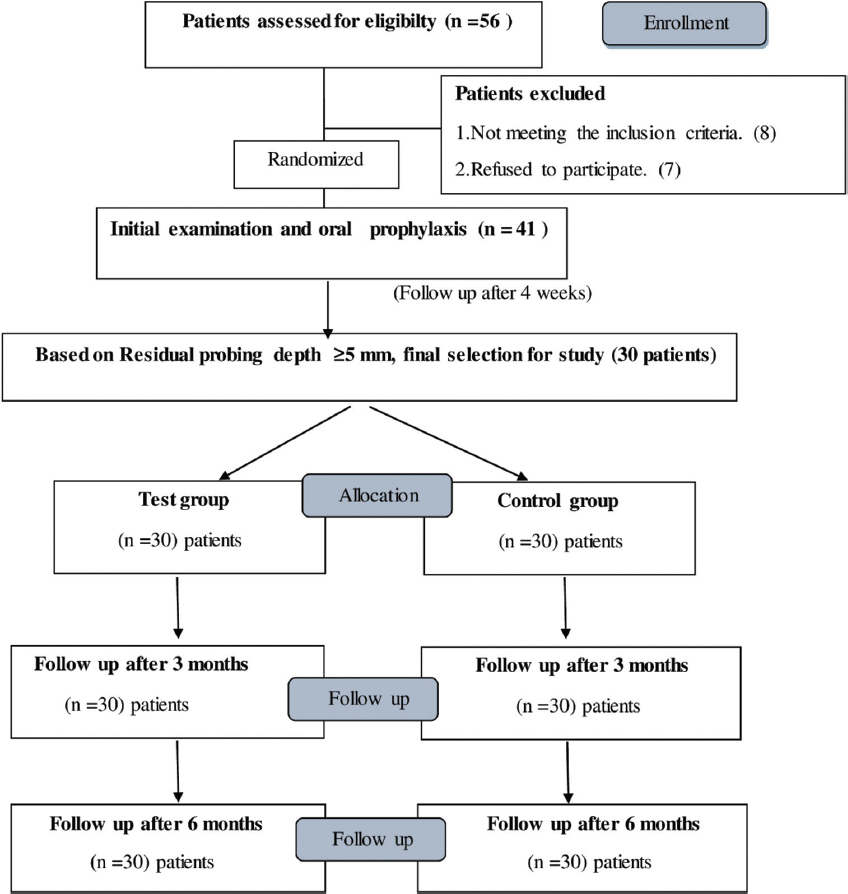
Long-cone parallel angle technique was used to obtain standardized IOPA X-rays by a single operator using a Vatech X-ray unit and Kodak 5100 intraoral X-ray sensor (Eastman Kodak Company, USA). The CS imaging software v7.0.23 (Carestream, Inc. 2017) was used for the evaluation of digital imaging. CBCT was done on each patient using a NewTom Giano 9000 (Verona, Italy) CBCT machine. The radiographic parameters measured were (1) the depth of the defect which is the distance from CEJ to the base of the defect and (2) DD percentage. The images were analyzed by a single experienced examiner. Radiographic assessment was done for IOPA and CBCT according to Misch et al.[19] Evaluation of percentage of defect depth reduction (DDR%) was done as per the formula given below:
Where DD is the linear radiographic depth (in mm) of the defect.
After enrollment, the subjects were randomly assigned test sites (30 sites treated with MWF under a magnifying loupe) and control sites (30 sites treated by conventional MWF) by computer-generated system using Excel 2013, v15.0 for Microsoft Windows. [Figure 3] In subjects with more than one adjacent IBDs, the defect measuring the greatest intrabony component was included in the study. The computer-generated sequence allocation was opened immediately before the procedure to allot the test site or control site. Randomization tables were used to assign the flap design and site of operation with subjects numbered according to the order in which they presented for surgery. The time interval between the sides/arches was at least 2 weeks. The test sites of all subjects were treated first followed by the control site.
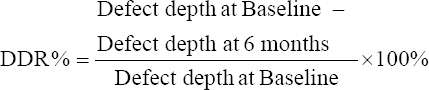
- Radiographs (a) Intraoral periapical (IOPA) at microsurgical site at baseline (b) IOPA at microsurgical site at 6 months (c) cone beam computed tomography (CBCT) at microsurgical site at baseline (d) CBCT at microsurgical site at 6 months
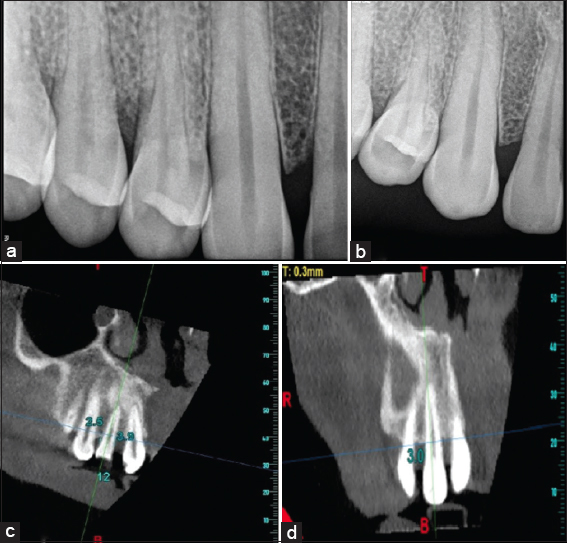
- Radiographs (a) Intraoral periapical (IOPA) at conventional site at baseline (b) IOPA at conventional site at 6 months (c) cone beam computed tomography (CBCT) at conventional site at baseline (d) CBCT at conventional site at 6 months
- Flow chart of study design
Surgical procedure
One operator (principal investigator) performed all periodontal surgical procedures under standard aseptic conditions. In the test site, 2% lignocaine hydrochloride with 1:1,00,000 adrenaline was used to anesthetize the operative site. Microsurgery was performed with 4× prismatic loupe (Zumax, Korea) as shown in [Figure 4a]. After achieving adequate anesthesia, the internal bevel followed by crevicular incisions was extended at least one tooth mesial and distal to the tooth associated with the IBDs on both facial and lingual/palatal side by microsurgical blades i.e., 15° Lance tip ophthalmic knife as shown in [Figure 4b]. A microsurgical periosteal elevator was used to elevate a full-thickness buccal and palatal/lingual flap.[20] A third interdental incision was made in a horizontal direction. Surgical debridement was carried out to remove subgingival plaque and calculus. Pocket epithelium and granulation tissue were removed using Gracey curettes (Hu-Friedy No. 5–6, 11–12, 13–14) and ultrasonic scalers. The surgical sites were irrigated with sterile saline. The flaps were sutured using 6–0 polyamide microsutures shown in [Figure 4c]. A non-eugenol dressing (Coe pak, GC America Inc., USA) was applied on the operated site [Figure 5].
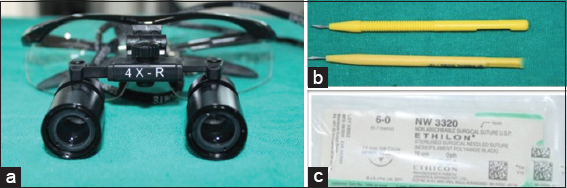
- Instrumentation for microsurgical site (a) 4× Prismatic loupes (b) 15° lance tip ophthalmic knife microblades (c) 6–0, polyamide 10 mm 3/8 reverse cutting needle sutures
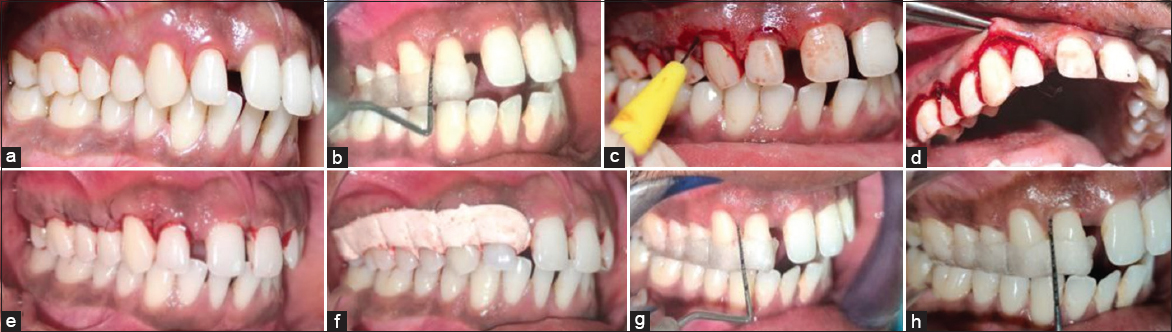
- (a) Pre-operative microsurgical site at baseline (b) Probing pocket depth (PPD) and relative clinical attachment level (RCAL) at microsurgical site at baseline (c) Internal bevel incision with microsurgical blade lance tip ophthalmic knife (d) Flap reflection with microsurgical periosteal elevator and debridement (e) Suturing done with 6–0 monofilament polyamide microsutures (f) Coe Pak applied at surgical site (g) Follow-up PPD and RCAL at microsurgical site at 3 months (h) PPD and RCAL at microsurgical site at 6 months
The control site was treated with the conventional MWF technique as per instructed by Ramfjord and Nissle in 1974.[4] It was done with B.P. blades No-11, 12, and 15 and regular periodontal surgical instruments. 4–0 silk suture was used to approximate the flaps. Every surgical step was done conventionally without the dental loupe [Figure 6].
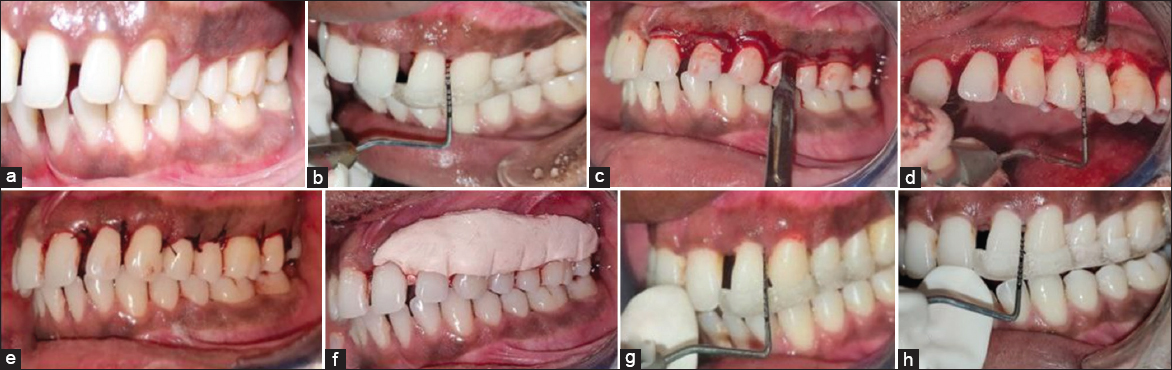
- (a) Pre-operative conventional site at baseline (b) probing pocket depth (PPD) and relative clinical attachment level (RCAL) at conventional site at baseline (c) Internal bevel Incision with surgical blade (d) Flap reflection with molt periosteal elevator and debridement (e) Suturing done with 3–0 Mersilk sutures (f) Coe-Pak applied at surgical site (g) Follow-up PPD and RCAL at conventional site at 3 months (h) PPD and RCAL at conventional site at 6 months
Post-operative instructions
Amoxicillin 500 mg and ibuprofen 400 mg were given 3 times daily for 3 days. Patients were advised to rinse with 0.2% undiluted chlorhexidine gluconate 10 mL 2 times daily for 1 week. Periodontal dressings and sutures removed 1-week postoperatively. The measurements of clinical parameters were taken at 3 and 6 months and radiographic assessment of the IBDs was taken after 6 months.
Statistical analysis
The data were analyzed using SPSS for Windows (SPSS version 22.0, IBM Corp., Armonk, NY). Continuous data between two different groups were analyzed using an unpaired “t” test. Within-group comparison was done using repeated measures analysis of variance followed by multiple pairwise comparisons and paired “t” test. Graphs and tables were used for the presentation of data and the statistical significance was set at P < 0.05.
Results
The demographical data regarding the age, gender, and site of IBDs are described in Table 1. The age of the participants ranged between 25 and 60 years where 46.6% are males and 53.4% are females.
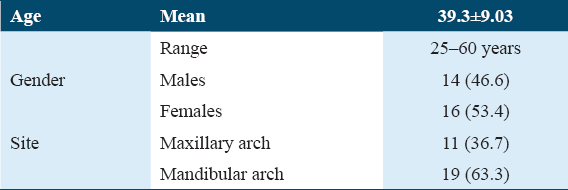
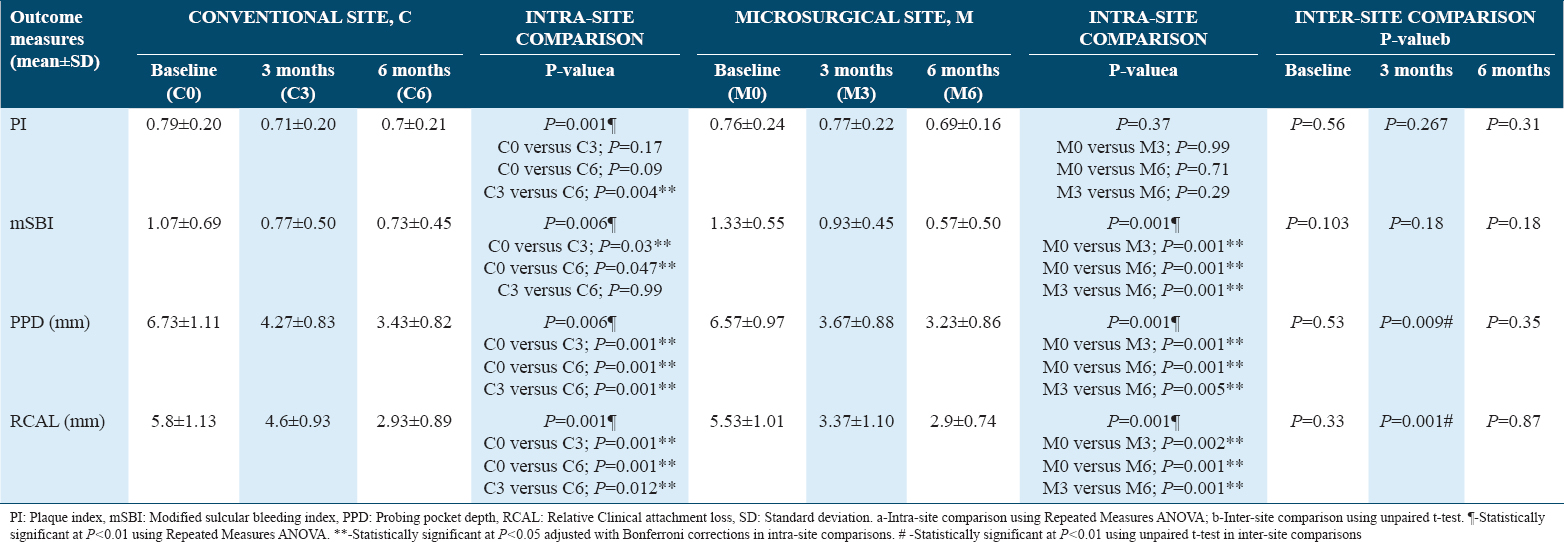
Table 2 depicts changes in the clinical parameters from baseline to 3 months and 6 months where PI and mSBI showed a statistically significant improvement in the conventional group. PI showed no statistically significant difference in the microsurgical group whereas mSBI showed a statistically significant difference in the microsurgical group, but the intergroup comparison was not significant. Table 2 also shows statistically significant improvement in PPD and CAL in both the groups from baseline to 3 months and 6 months, while inter-group comparisons showed better results in the microsurgical group which was statistically significant at 3 months.
The radiographic measurements depicting mean DD using IOPA and CBCT in Table 3 showed statistically significant improvements in both the groups from baseline to 6 months regarding defect fill. It shows a non-significant difference between the 2 groups when IOPA was done to compare mean DD reduction but a significant difference between the 2 groups when CBCT was done to compare mean DD reduction. Table 3 also shows a comparison of DD difference from baseline to 6 months where DD reduction was more in the microsurgery group than conventional group that was statistically significant (P = 0.004).
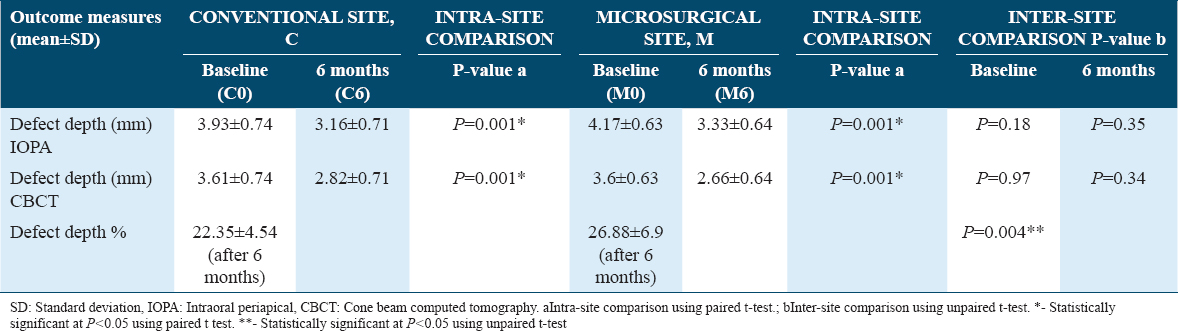
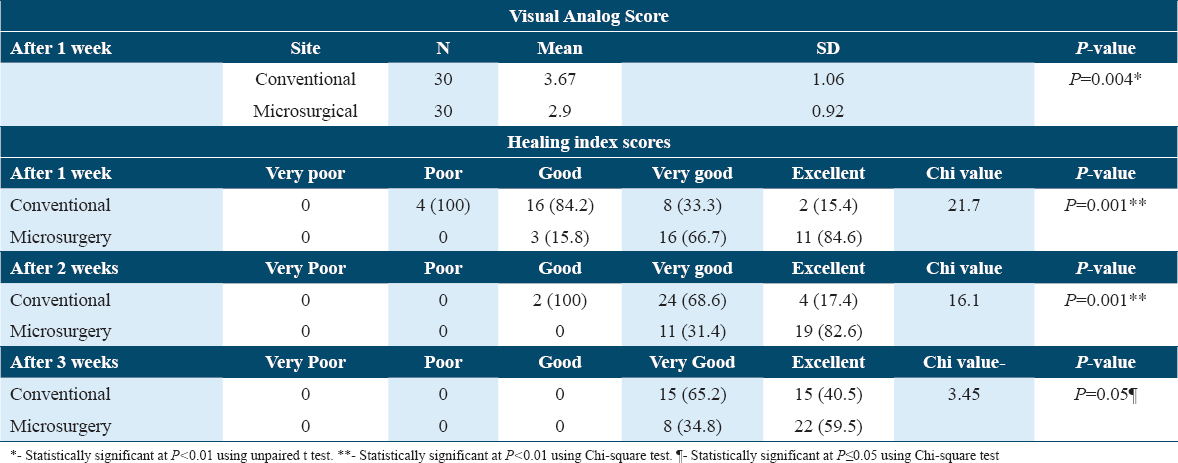
Table 4 shows VAS scores where it is seen that VAS pain scores at microsurgical sites after 1 week were less than conventional sites which was statistically significant. Table 4 also illustrates that after 1-week, 2-week, and 3-week patients had excellent healing scores for the microsurgery group as compared to the conventional group that was statistically significant.
Discussion
The present single-center split-mouth randomized controlled trial was carried out to evaluate and compare the clinical and radiographic treatment outcomes following MWF procedures with 4× prismatic loupe and the conventional MWF. Results of the present study showed a reduction in probing depth and gain in clinical attachment level at 3 and 6 months in both groups with comparatively better results in the microsurgical group. There was significant improvement in PPD and CAL score at 6 months in microsurgery-treated sites. Excellent healing scores and less VAS pain scores were seen for the microsurgery group. There was statistically significant intrabony DD reduction at 6 months which was more in the microsurgical site which was evident in CBCT. There is hardly any literature available to compare the clinical outcomes following MWF procedures with and without 4x prismatic loupes in the management of infrabony pockets. To the best of our knowledge, this is the first-ever study that compares the clinical and radiographic outcomes following MWF procedures with 4× prismatic loupe to that of conventional one. To remove the effect of individual patient characteristics and a more powerful estimate with a smaller size, a split-mouth design was planned. As the periodontal disease stability was measured over a period of 4–8 weeks, till the baseline data were collected without any episode of active disease, the period effect was overruled. As a minimum of 2 weeks gap was given between the test and control site and strict plaque control measures were undertaken, a spillover effect is not possible between the groups and an unbiased assessment of all parameters was performed.[21] The sample size used in this study was in accordance with the vast majority of clinical periodontal studies in humans; moreover, it was estimated with a pilot study and proper sample size estimation.[21] In this research, the parameters taken into consideration were plaque index score, mSBI score, PPD, RCAL, HI scores, VAS pain score, DD, and DD percentage. Moreover, probably, this is the first-ever study measuring the alveolar bone level through CBCT in patients with IBDs with or without 4× magnifying loupes. Mean plaque and bleeding scores: on comparison, the mean plaque scores between the conventional and microsurgery group was statistically not significant (P = 0.56). A trend toward lower mean plaque score was observed in both the microsurgical and conventional groups. This might have been due to the rigorous periodontal maintenance. For the success of periodontal treatment and disease control, effective plaque and calculus removal have always been an important factor. The mean bleeding score was reduced after 3 months and 6 months in both the groups but it was not statistically significant which is in accordance with Perumal et al., 2015, Chacko et al., 2021, and Shetty et al., 2019.[20,22,23] There was a reduction in bleeding scores suggesting a reduction in inflammation after both treatment modalities which is in agreement with Wachtel et al., 2003 and Fickl et al., 2009.[24,25] Results of the present study showed improved probing depth and gain in clinical attachment level at 3 and 6 months in both groups with slightly better results in the microsurgical group as seen in the studies by Wachtel et al., 2003 and Fickl et al. 2009.[24,25] There was significant improvement in PPD score at 6 months and 12 months in microsurgery-treated sites. Studies by Chacko et al., 2021 and Reddy et al., 2019 showed similar findings[22,26] but the findings of PPD and RCAL in the study done by Perumal et al., 2015 did not show a significant difference at 3 months between the test and control group which is in contrast to our study.[20] Excellent healing scores were seen for the microsurgery group. This could be attributed to minimal trauma due to the use of micro sutures (6–0) which reduces inflammation and pain. Improved healing is also due to proper tissue handling and with precise closure of the wound as seen in studies done by Chacko et al., 2021, and Perumal et al., 2015.[20,22] Shetty and Bebika 2018 confirmed this finding where they did a histologic examination of the healing tissues which was in favor of the microsurgical approach.[27] Curtis et al. 1985 assessed healing clinically by evaluating the gingival color change, assessment experience of the degree of swelling by the patient, bleeding, pain, and root sensitivity after periodontal surgery.[28] Our result is also in accordance with the early wound HI after surgery by Wachtel H et al. 2003[24] and fluorescent angiograms for vascularization by Burkhardt and Lang 2005.[29] Statistically significant mean VAS pain scores were obtained which was less at microsurgical sites at 1 week. Similar results were seen in studies done by Chacko et al., 2021, and Perumal et al., 2015.[20,22] This could be because of using finer sutures and microsurgical blades and instruments. There was statistically significant intrabony DD reduction at 6 months in the microsurgical site as evident in CBCT. There are numerous factors like the force with which probing is done, the shape of the tip, and probe direction that affects the clinical results.[30] IOPA radiographs may overestimate or underestimate the amount of bone loss due to projection errors and they also lack 3D information. Till today, not much efforts have been made to compare radiographic bone levels between both groups using CBCT.[19] Therefore, in this study, we have evaluated using both the IOPA and CBCT. To maintain the beneficial effects of therapy, a recall of once every 3 months appears to be sufficient even if there is variation in individual personal oral hygiene and gingival inflammation. Revaluation of surgical therapy should be done approximately 3 months after the surgical therapy.[31] This study has some limitations, in split-mouth design, blinding of subjects whenever feasible minimizes treatment response bias. In this study, it was difficult to blind patients and surgeons, however, optimum care was taken to avoid treatment response bias by doing the test site first followed by the control site, justifying the chance of post-operative pain due to apprehension at the first surgery. The healing indices used are subjective. Fluorescein angiogram, evaluation of healing by immunohistochemistry using various MMPs as markers, and flow cytometry using markers for various cells and cytokines are methods which are objective and yields more reliable results. The future implications of this study are the emergence of a microsurgical approach under magnification greatly influenced clinical outcomes in delicate tissues like periodontium. It will help in surgically treating the patient in a more conservative manner as there is faster healing of the surgical site, increased visibility of the surgical field, and increased acceptance by the patient as they experience less pain and post-operative morbidity. Hence, periodontal microsurgery with 4× prismatic loupe should be performed in day-to-day clinical practice which will be widely accepted by the patients.
Conclusion
Taking into consideration of the limitations in the present study, it can be concluded that microsurgery under 4× magnifying loupe is as effective as conventional MWF surgery in the treatment of infrabony pockets but microsurgery greatly enhances the predictability of improvements in terms of less discomfort to the patient and improved healing. 4× prismatic loupe can be the choice of magnification system in periodontal microsurgery when an operating microscope is unavailable. Magnification-assisted surgical procedures will help the periodontist in treating the patient in a more conservative manner as it uses enhanced visibility of the surgical field which increases the effectiveness of SRP, minimizes surgical wounds, fastens healing, decreases post-operative morbidity, and increases acceptance by the patient as they experience less pain. Further long-term, multicentric randomized controlled trial studies are required in this to strengthen the evidence.
Ethics Approval and Consent to Participate
It was recommended under the IEC, SCB Dental College and Hospital, Cuttack, Odisha (IEC/SCBDCH/072/2020 dated March 11, 2020). The patient’s consent statement to participate in this study and for publication was taken.
Availability of Data and Material
The data used in this study are available and will be provided by the corresponding author on a reasonable request.
Competing Interests
None.
Funding Statement
None.
Authors’ Contributions
Conceptualization: Subash Chandra Raj (SR) and Shaheda Tabassum (ST). Methodology: Dr. Neelima Katti (NK) and Shaheda Tabassum (ST). Formal analysis: Subash Chandra Raj (SR) and Dr Devapratim Mohanty (DM). Literature search: Dr Swoyangprava Sil (SS) and Debajani Baral (DB). Data curation: Shaheda Tabassum (ST). Project administration: Subash Chandra Raj (SR) and Dr Devapratim Mohanty (DM). Visualization and Supervision: Subash Chandra Raj (SR) and Dr NeelimaKatti (NK) Manuscript preparation: Subash Chandra Raj (SR) and Shaheda Tabassum (ST). Manuscript editing: Shaheda Tabassum (ST) and DebajaniBaral (DB). Manuscript review: Dr. Neelima Katti (NK) and Dr Devapratim Mohanty (DM).
Acknowledgment
None.
References
- Glossary of Periodontal Terms (4th ed). Chicago: American Academy of Periodontology; 2001. p. :44.
- Nonsurgical and surgical treatment of periodontitis:How many options for one disease. Periodontol 2000. 2017;75:152-88.
- [Google Scholar]
- An overview of nonsurgical and surgical therapy. J Periodontol 2000. 2004;36:35-44.
- [Google Scholar]
- Present status of the modified widman flap procedure. J Periodontol. 1977;48:558-65.
- [Google Scholar]
- Hall's Critical Decisions in Periodontology and Implantology. USA: People's Medical Publishing House; 2013.
- Osseous resection;a basic principle in periodontal surgery. Oral Surg Oral Med Oral Pathol. 1949;2:31625.
- [Google Scholar]
- Longterm evaluation of periodontal therapy:I. Response of 4 treatment modalities. J Periodontol. 1996;67:93102.
- [Google Scholar]
- A perspective on periodontal microsurgery. Int J Periodontics Restorative Dent. 2001;21:191-6.
- [Google Scholar]
- Comparison between micro-and macrosurgical techniques for the treatment of localized gingival recessions using coronally positioned flaps and enamel matrix derivative. J Periodontol. 2010;81:1572-9.
- [Google Scholar]
- A perspective on the future of periodontal microsurgery. Periodontol 2000. 1996;11:5864.
- [Google Scholar]
- Principles and practice of periodontal microsurgery. Int J Microdent. 2009;1:13-24.
- [Google Scholar]
- J Am Med Assoc. 2013;310:2191-4.
- Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121-35.
- [Google Scholar]
- The microbiota osseointegrated with successful or failing implants. Oral Microbiol Immunol. 1987;2:145-51.
- [Google Scholar]
- Stent as an accessory tool in periodontal measurements:An insight. J Indian Soc Periodontol. 2019;23:81-4.
- [Google Scholar]
- Effectiveness of benzydamyne HCl in the treatment of periodontal post-surgical patients. Res Clin Forums. 1988;10:105-18.
- [Google Scholar]
- Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261-6.
- [Google Scholar]
- Comparison of microsurgical and conventional open flap debridement:A randomized controlled trial. J Indian Soc Periodontol. 2015;19:406-10.
- [Google Scholar]
- Split-mouth and cross-over designs in dental research. J Clin Periodontol. 1990;17:446-53.
- [Google Scholar]
- Microsurgical and conventional open flap debridement procedure in the management of periodontitis:A comparative clinical study. IOSR J Dent Med Sci. 2021;20:24-32.
- [Google Scholar]
- A comparative clinical evaluation of microsurgical and conventional open flap surgical procedure in patients with chronic periodontitis-a pilot project. Int J Sci Res. 2019;8:4-7.
- [Google Scholar]
- Microsurgical Access flap and enamel matrix derivative for the treatment of periodontal intrabony defects:A controlled clinical study. J Clin Periodontol. 2003;30:496-504.
- [Google Scholar]
- Microsurgical access flap in conjunction with enamel matrix derivative for the treatment of intra-bony defects:A controlled clinical trial. J Clin Periodontol. 2009;36:784-90.
- [Google Scholar]
- Open flap debridement using microsurgical loupes and modified widman flap approach -a case series. Int J Appl Dent Sci. 2019;5:96-9.
- [Google Scholar]
- Comparative evaluation of microsurgical and conventional open flap surgical procedure outcomes in patients with periodontitis-a histopathological and scanning electron microscopy study. Biomed J Sci Tech Res. 2018;6:1-6.
- [Google Scholar]
- The incidence and severity of complications and pain following periodontal surgery. J Periodontol. 1985;56:597-601.
- [Google Scholar]
- Coverage of localized gingival recessions:Comparison of microandmacrosurgical techniques. J Clin Periodontol. 2005;32:287-93.
- [Google Scholar]
- Probing pocket depth and clinical attachment level between non-surgical and surgical periodontal therapy in chronic periodontitis patients:A randomised controlled clinical trial. J Nepal Soc Periodontol Oral Implantol. 2018;2:40-4.
- [Google Scholar]







