Translate this page into:
Factors delaying mobilization after hip and knee arthroplasty
Address for correspondence: Kamran Hafeez, Department of Trauma and Orthopedics, Kings Mill Hospital, Sutton in Ashfield, Nottinghamshire, NG17 4JL, United Kingdom. E-mail: kamranhafeez@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
ABSTRACT
Objective:
Arthroplasty patients undergo pre-operative assessment and medical optimization before surgery with the objective to mobilize and discharge home as soon as deemed fit to reduce hospital stay. This study was aimed to investigate factors delaying mobilization after hip and knee arthroplasty in our hospital.
Methods:
This observational study was conducted in our hospital between August 2021 and October 2021. We included all elective orthopedic patients who were admitted for hip and knee arthroplasty during this period. Patients admitted for revision arthroplasty were excluded from the study. We collected data prospectively on a pro forma including patient demographics and different other variables. All patients were reviewed on the first post-operative day by one of the authors and pro formas were completed. We used SPSS to analyze data.
Results:
Sixty patients were included; 32 females and 28 males with a mean age of 69.62 years. Primary knee arthroplasty was done in 30 patients while 30 underwent primary hip arthroplasty. Most of the patients (n = 50) were mobilized on the 1st day; however, ten patients were unable to mobilize. Orthostatic hypotension, dizziness, and pain were statistically significant factors responsible for failed mobilization on day one. Patients who failed to mobilize on day one had longer hospital stay (P = 0.018).
Conclusion:
Orthostatic intolerance and post-operative pain were independent factors delaying mobilization after hip and knee arthroplasty thereby increasing the length of stay in these patients.
Keywords
Hip arthroplasty
Knee arthroplasty
Mobilization
Orthostatic intolerance
Introduction
Osteoarthritis is a common joint disease affecting many individuals across the world.[1] Lower limb arthroplasty is an effective treatment option in osteoarthritis affecting knee and hip joints.[2] It helps in relieving the symptoms, and improves mobility and quality of life.[3] With increasing life span, the burden of arthritis on the health-care system is constantly increasing. In United Kingdom, many people are waiting for their arthroplasty procedures to be done under NHS. Enhanced Recovery After Surgery (ERAS) Society strongly recommended to mobilize the patient as soon as possible after arthroplasty.[4] Arthroplasty patients can be mobilized as early as within 24 h of surgery, and length of stay can be reduced.[5] In addition to reducing length of stay, early mobilization also helps in preventing adverse physiological effects including reduced pulmonary function, impaired tissue oxygenation, risk of pneumonia, urinary tract infection, and venous thromboembolism.[6,7] A number of factors have been reported to be responsible for delayed mobilization in post-operative period.[8,9]
Elective arthroplasty patients are medically optimized before surgery and aimed to be mobilized as early as possible to reduce the length of stay. We have observed that some of our patients failed to be mobilized on day 1 after primary hip or knee arthroplasty. The aim of this study was to identify the factors that were responsible for delaying the mobilization in post-operative period in our hospital.
Methods
This is a prospective observational study conducted at our hospital from August to October 2021. The study was approved by the Hospital Research Committee. All elective lower limb arthroplasty patients admitted during this period were assessed. Patients undergoing primary hip or knee arthroplasty were included in the study. Patients with revision arthroplasty were excluded from the study.
Patients were assessed in anesthesia pre-operative clinic before admission and were medically optimized. Patients were allowed to take their regular medications until the day of surgery except oral anticoagulants, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers. These were restarted on day one. TEDs stockings were prescribed to all and assessed for venous thromboembolism. Patients underwent surgical procedure under general or regional anesthesia with local ropivacaine infiltration in some patients as per surgeon preference. None of the patients received a block for the procedure. Postoperatively, all patients were prescribed for analgesia by an anesthetist and managed by a pain team. DVT prophylaxis was prescribed as per NICE guidelines.
On day one, patients were encouraged to mobilize out of bed under direct supervision of physiotherapists. During mobilization, patients were assessed for symptoms of orthostatic hypotension including nausea, vomiting, and dizziness. Blood pressure readings were taken in the case of a symptomatic patient. If the symptoms were severe enough, then patients were not mobilized and shifted back to the bed. Pain score was calculated using visual analog score before and during mobilization. Patient analgesia prescription was reviewed, and morphine equivalent daily dose per day was calculated.[10] Post-operative bloods were repeated, and hemoglobin level was compared with pre-operative values. Patient length of stay was recorded once discharged from the hospital.
A pro forma was designed to record patient demographics, medical comorbids, medications, type of anesthesia, surgical details, and assessments at day one. Data were analyzed on SPSS. Different variables were compared in between patients who were mobilized or not. For categorical variables, Chi-square or Fischer exact test was used and for continuous variables, the independent samples t-test or Mann–Whitney U-test was used.
Results
There were 60 patients who underwent primary knee (n = 30) or hip (n = 30) arthroplasty during our study period. Mean age was 69.62 years (43–86 years) and 32 patients were females while 28 were male. Most of the patients (n = 57) were operated under spinal anesthesia and only three patients were under general anesthesia. Local infiltration of the operative field with ropivacaine was done in 25 patients.
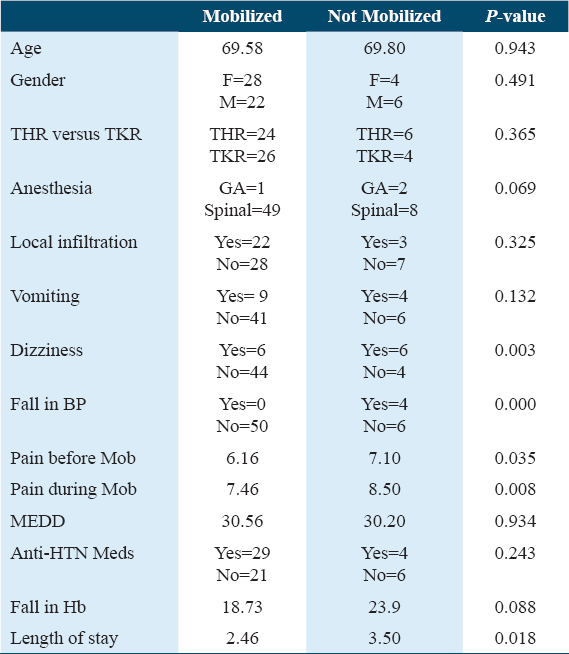
All the patients were assessed by physiotherapist and were given a chance to be mobilized under supervision; however, ten patients failed to mobilize on day one. Some patients showed orthostatic intolerance when mobilized on day one. Thirteen patients experienced vomiting and 4 failed to mobilize (P = 0.132). Twelve patients felt dizziness and 50% (n = 6) were not mobilized (P = 0.003). Four patients had a fall in blood pressure as compared to pre-mobilization blood pressure and all failed to mobilize (P = 0.000). Thirty-three patients were taking anti-hypertensive medications including atenolol, amlodipine, bisoprolol, losartan, ramipril, and furosemide; however, there was no statistically significant difference in terms of mobilization (P = 0.243).
The mean pain score in the patients before mobilization was 6.32. It was higher in the group of patients who failed to mobilize (7.1 vs. 6.16; P = 0.035). Similarly, the mean pain score during mobilization was 7.63. Again, it was higher in the group of patients who failed to mobilize (8.5 vs. 7.46; P = 0.008). All patients received opioids as analgesia in post-operative period. Mean morphine equivalent daily dose (MEDD) was almost similar in both groups of patients who were mobilized or not (30.56 vs. 30.20; P = 0.934).
Mean fall in hemoglobin was a little more in the patients who were not mobilized; however, the result was not statistically significant (23.9 vs. 18.73; P = 0.088). Patients who failed to mobilize stayed on average a day longer as compared to those who mobilized on the 1st day (P = 0.018). Results are summarized in Table 1.
Discussion
In our study, we found that many patients (83.3%) were mobilized on day 1; however, some (16.6%) failed to mobilize on day one after surgery resulting in increased length of stay. Pain and orthostatic intolerance including low blood pressure and dizziness were the main factors affecting mobilization at day one.
Early mobilization after lower limb arthroplasty provides the number of health benefits, improve patient satisfaction, reduces rate of post-operative complications including DVT and reduced length of stay.[11] Chua et al.[12] presented the results of their observational study in which 818 total hip arthroplasty and 989 total knee arthroplasty patients were followed prospectively at 19 Australian hospitals. They found that at the end of day 1 65.2% of the patients were mobilized. Hospital site was one of the important covariant in their study as early mobilization required availability of staff which affected the mobilization protocols at different hospital sites. In addition, any acute complication may also delay mobilization. We also found staff shortage a limiting factor in our study as the physiotherapy team was only available at 1 time in a day. If the patient failed to mobilize once, then he was reviewed the next day. Vomiting, dizziness, and pain were also found to delay mobilization in our patients. Fast-track protocols favor mobilization at day 0 and consider it safe.[13] Prinsloo and Keller[14] compared a prospective patient group, which received an increased frequency of physiotherapy visits on day 0 to mobilize them early, with the traditional retrospective group undergoing hip and knee arthroplasty. They reported that same-day discharge is possible in patients undergoing advanced rehabilitation pathway. However, in our hospital, patients were mobilized at day one, again linked to availability of physiotherapy team.
Post-operative pain also affects mobilization. Holm et al.[15] reported that 90% of their TKA patients were mobilized on the first day with a median pain intensity of 5 or less. In our study, the mean pain score at day 1 was 6.32 at rest and 7.63 during mobilization. Local infiltration of analgesia is an effective pain management tool in total knee arthroplasty with short-term safety.[16] In our study, 25 patients received local infiltration at the time of surgery. However, three patients who received local infiltration also failed to mobilize on day 1. There was no statistically significant difference between the patients with local infiltration who were mobilized or not (P = 0.325). Additional adjuncts also can improve pain management and enhance recovery of joint function. Liao and Xu[17] reported that application of cold therapy improves pain and swelling after total knee arthroplasty and shortens the recovery time.
Post-operative nausea and vomiting affect patient rehabilitation after hip and knee arthroplasty, increases length of stay, and leads to poor patient satisfaction. Wang et al., reported vomiting in 7.52% of the patients who underwent unilateral hip or knee arthroplasty.[18] In our study, 21.6% (n = 13) had vomiting and four failed to mobilize. It might be due to opioid analgesia receiving in post-operative period. Bulut and Vatansever[9] assessed different factors affecting mobilization after hip and knee arthroplasty. In their study, nine patients had nausea/vomiting before mobilization and two patients had hypotension after mobilization; however, it was not statistically significant affecting mobilization time.
Raut et al.,[19] examined various factors affecting the length of stay after total knee arthroplasty in patients over 75 years of age. They reported that patients who were mobilized early had reduced length of stay. In our study group, we also found that patients who failed to mobilize on day 1 stayed longer as compared to those who were mobilized. Smith et al.[20] studied the clinical outcome of 95 patients of total hip and knee replacements who followed an enhanced recovery program. The patients who were mobilized on day 0 had shorter length of stay and better pain scores postoperatively. Oberfeld et al.[21] compared two groups undergoing total hip arthroplasty in their randomized controlled trial. They focused on obese, elderly, and severely diseased patients. Patients in the first group were mobilized on day 0 while the patients in the other group were mobilized on day 1. They reported that the time to readiness for discharge was shorter in patients mobilized on day 0 and there was no increase in the rate of immediate adverse events.
Decreasing the length of stay will increase the availability of beds which can be utilized for providing medical services for other needy patients. There were some limitations of this study including a small number of patients as we were operating with reduced capacity due to COVID, and single-center design.
Conclusion
Post-operative pain and orthostatic intolerance were independent factors responsible for delayed mobilization. We recommend better pain control, an earlier visit by the pain team before mobilization, and use of other modalities like cryo cuff in TKA patients to improve pain. Availability of physiotherapy staff in the latter half of the day was to give another chance to those who failed to mobilize.
Authors’ Declaration Statements
Ethical approval and consent to participate
Approval was obtained from the Hospital Research Committee. Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Availability of data and material
The authors confirm that the data supporting the findings of this study are available within the article.
Competing interests
The authors declare that they have no conflicts of interest.
Funding statement
There is no funding source.
Authors’ contributions
All authors contributed to the study’s conception and design.
Acknowledgment
Not applicable
References
- Effectiveness of patient decision aids for total hip and knee arthroplasty decision-making:A systematic review. Osteoarthritis Cartilage. 2021;29:1399-411.
- [Google Scholar]
- Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86:963-74.
- [Google Scholar]
- Consensus statement for perioperative care in total hip replacement and total knee replacement surgery:Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2020;91:3-19.
- [Google Scholar]
- Early mobilization of patients who have had a hip or knee joint replacement reduces length of stay in hospital:A systematic review. Clin Rehabil. 2015;29:844-54.
- [Google Scholar]
- Low risk of thromboembolic complications after fast-track hip and knee arthroplasty. Acta Orthop. 2010;81:599-605.
- [Google Scholar]
- Incidence and risk factors of orthostasis after primary hip and knee arthroplasty. J Arthroplasty. 2022;37:S70-5.
- [Google Scholar]
- Determination of factors affecting early mobilization of patients who have undergone knee and hip arthroplasty. J Perianesth Nurs. 2022;37:646-53.
- [Google Scholar]
- Opioid Converter. Available from: https://www.paindata.org/calculator.php
- Risk of re-admission, reoperation, and mortality within 90 days of total hip and knee arthroplasty in fast-track departments in Denmark from 2005 to 2011. Acta Orthop. 2014;85:493-500.
- [Google Scholar]
- Early mobilisation after total hip or knee arthroplasty:A multicentre prospective observational study. PLoS One. 2017;12:e0179820.
- [Google Scholar]
- Rapid mobilization decreases length-of-stay in joint replacement patients. Bull Hosp Jt Dis (2013). 2013;71:222-6.
- [Google Scholar]
- Same-day discharge after early mobilisation and increased frequency of physiotherapy following hip and knee arthroplasty. S Afr J Physiother. 2022;78:1755.
- [Google Scholar]
- The role of pain for early rehabilitation in fast track total knee arthroplasty. Disabil Rehabil. 2010;32:300-6.
- [Google Scholar]
- Efficacy and safety of single-dose local infiltration of analgesia in total knee arthroplasty:A meta-analysis of randomized controlled trials. Knee. 2014;21:636-46.
- [Google Scholar]
- The effect of cold therapy combined with ERAS in the postoperative care of patients undergoing total knee arthroplasty. Am J Transl Res. 2022;14:3154-63.
- [Google Scholar]
- Risk factors of postoperative nausea and vomiting after total hip arthroplasty or total knee arthroplasty:A retrospective study. Ann Transl Med. 2020;8:1088.
- [Google Scholar]
- Factors associated with prolonged length of stay following a total knee replacement in patients aged over 75. Int Orthop. 2012;36:1601-8.
- [Google Scholar]
- Rehabilitation implications during the development of the Norwich Enhanced Recovery Programme (NERP) for patients following total knee and total hip arthroplasty. Orthop Traumatol Surg Res. 2012;98:499-505.
- [Google Scholar]
- Effect of mobilization on the day of surgery after total hip arthroplasty in elderly, obese, and severely diseased patients. J Arthroplasty. 2021;36:3686-91.
- [Google Scholar]







