Translate this page into:
Impact of one-stop clinic on the clearance of COVID-19 surgical backlog
Address for correspondence: Yacoub Abuzied, Department of Nursing, Rehabilitation Hospi tal, King Fahad Medical City, Riyadh, Saudi Arabia. E-mail: yabuzied2@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
During the COVID-19 pandemic, there was a significant decrease in the number of operated elective cases due to the shutdown procedures. This situation created a substantial surgical backlog. Several visits are generally necessary before a surgical decision making and booking the surgery time. Improving patient access by creating “one-stop” clinics might help decrease the number of visits before the surgery. This study investigated the effect of one-stop clinic application as a new care model on COVID-19 surgical backlog clearance.
Methods:
We conducted a quasi-experimental, interrupted time-series, pretest-posttest study design in the northern areas of Saudi Arabia. The study outcomes were the number of surgeries and the time elapsed from the first seen day to the booked room day.
Results:
A total of 358 surgeries were included. Of them, 107 (29.9%) surgeries were performed before initiation of the one-stop clinic and 251 (70.1%) after initiation. The median (quartile Q1, Q3) time elapsed from the first seen day until the booked OR day post-one-stop clinic was 10 (6-17), which was significantly lower than pre-one-stop clinic 20 (11-33), P < 0.0001.
Conclusion:
One-stop clinics shortened the period between first visit and booking in the operating room. One-stop clinics may alleviate the surgical backlog resulting from the COVID-19 crisis.
Keywords
COVID-19
clearance
one-stop clinic
surgical backlog
Introduction
A coronavirus disease 2019 (COVID-19) was recently identified as a viral infection with severe acute respiratory syndrome triggered by a coronavirus 2 (SARS-CoV-2). The first pneumonia case was reported in December 2019 in Wuhan, China. The virus has spread exponentially worldwide, leading to the World Health Organization (WHO) declaring COVID-19 a public health emergency.[1] On 11th March 2020, the WHO officially reported COVID-19 as a pandemic.[2]
Soon after the WHO announced a pandemic, many countries globally took steps to contain and prevent the virus’s spread. Curfews, quarantines, lockdowns, and other restrictions were put in place worldwide to control the further spread of COVID-19 infection.[3] These restrictions disturb everyday life activities and affect many sectors, including the health care system. During the COVID-19 pandemic, there was a complete shutdown of surgical services or decreased the number of elective surgeries due to the overwhelming health system with COVID-19 cases. This, in turn, created a vast surgery backlog.
The COVID Surg Collaborative Project expected canceling or delaying more than 28 million surgeries across 190 countries in the first 12 weeks of COVID-19.[3] Another study estimated the recovery time until the health care system returned to its total capacity to be between 7 and 16 months.[4] In Canada, the estimated size of elective surgical backlog during COVID-19 pandemics was 148,364 surgeries, with an average increase of 11,413 surgeries per week and 84 weeks of estimated backlog clearance time.[5]
Further, the surgical backlog during COVID-19 caused profound financial pressure and economic impact. The American Hospital Association estimated the financial impact of an average of $50.7 billion per month in losses for America’s hospitals and health systems.[6] The Canadian Medical Association estimated that an extra $1.3 billion in funding is required to return waiting times to pre-pandemic levels.[6] These estimates would be much higher if the costs associated with hospital space limitations, restricted machinery, and other restrictions of the COVID-19 policy were applied.[6]
The COVID-19 surgical backlog has severe consequences for the recovery stage. In addition to the capacity of the health care system reduction, the anticipated demand will likely result in the creation of waitlists and potentially worsening health effects, making it critical to beginning recovery planning as soon as possible. Under the existing system, the patients seeking surgical services will be initially seen in an outpatient clinic. Several visits are generally necessary before a management decision and booking in the operating room for definitive treatment. Improving patient access by creating specific “one-stop” clinics may help reduce the number of waiting list patients, shorten the period between the first visit and surgery booking, and positively impact surgical backlog management, time utilization, and patient satisfaction.
A one-stop clinic offers consultation, a diagnosis, and a care plan in almost a single visit. The one-stop clinic contains a multidisciplinary team (consultants, nurses, imaging technicians, etc.) to accommodate patient’s needs during their visit. A one-stop clinic is not a new approach; it has been used frequently to solve surgical backlog or waiting time problems.[7-11] This approach was also projected by the National Health Service Institute for Innovation and Improvement to reduce the maximum waiting time and improve the patient experience.[12] Herein, we investigated the effect of the one-stop clinic’s application as a care model on clearance of COVID-19 surgical backlog in north areas of Saudi Arabia.
Methodology
This is a quasi-experimental, interrupted time-series, pretest-posttest study. The study was conducted in the northern areas of Saudi Arabia. The north areas include multiple provinces: Tabuk, Ha’il, Al Jawf, and Northern Borders regions. As per 2019 statistics, the population in these regions is estimated at 2,595,762 people, representing around 7.6% of Saudi Arabia’s population.[13] In 2019, the number of government hospitals in these regions was 50 Hospitals (48 MOH hospitals and two other governmental hospitals) with 7497 beds. In these regions, the number of private hospitals was four hospitals.[14]
The institutional review board approved this study of King Fahad Medical City, Riyadh, Saudi Arabia, which requested qualified collaborators from each site to facilitate the data collection and validate data. Permission from the hospitals under investigation was obtained to conduct this study. Data were gathered in each hospital by each collaborator and given to the researchers for review and analysis.
The one-stop clinics’ approach was started after the OR recovery stage in August 2020, and it was conducted in four hospitals. However, the data were available for analysis pretest-posttest in one hospital and posttest only in another hospital. Patients can receive multidisciplinary consultations, diagnoses, and a care plan in almost a single visit in these clinics. To facilitate the patients’ fast service without reducing quality, we reduced the unnecessary investigations and procedures [Figure 1]. The surgeries that operated through the one-stop clinic involved mainly general surgery, ophthalmology surgery, ENT surgery, and orthopedic surgery. Examples of these surgeries include but were not limited to cholecystectomy, adenoidectomy, nail removal, and cataracts.
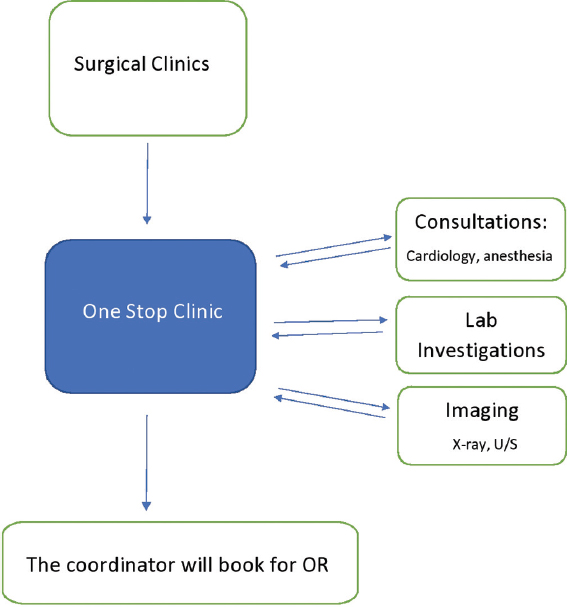
- Reduce unnecessary investigations and procedures
The surgical backlog was defined as the number of patients waiting for their elective surgeries. Lowering the waiting time from the first seen (visit) until the OR booking will reduce the surgical backlog. To study the effect of the one-stop clinic on clearance of surgical backlog, we calculated the number of surgeries and the time elapsed from the first seen day till the booked OR day (primary outcomes). We compared the period of one-stop clinic applications from August 17, 2020 to March 11, 2021 (posttest) with the period before establishing the one-stop clinic from December 1, 2019 to March 31, 2021 (pretest). We measured the time elapsed from the first seen day to the booked OR day per site (site 1 and 2) and specialty (general surgery, ophthalmology surgery, ENT surgery, and orthopedic surgery).
The categorical variables were represented as frequency and percentage, and the continuous variables as mean±standard deviation (SD) or median (quartile Q1, Q3). The Shapiro-Wilks test tested normality distribution. The student’s t-test or two-sample Wilcoxon rank-sum test was used to comparing the pretest and posttest groups of the time elapsed from the first seen day until the booked surgery. The Chi-square test or Fisher’s exact test compared the number of surgeries between the pretest and posttest groups. We calculated the 95% confidence interval, and the P < 0.05 was considered statistically significant. We constructed a run chart reporting the average of days from the first seen day until the booked OR day per month for the pretest and posttest periods. Statistical analysis was performed with Stata Statistical Software (Release 16. College Station, TX: StataCorp LLC. 2017).
Results
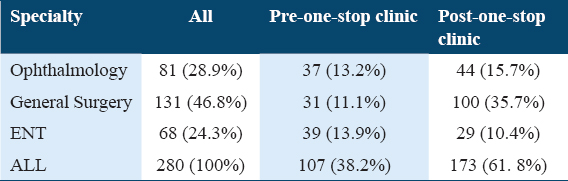
We included 358 surgeries in this study. Of them, 107 (29.9%) surgeries were performed before initiation of the one-stop clinic and 251 (70.1%) after initiation. On site one, there were 280 surgeries in which 107 (38.2%) surgeries were performed before initiation of the one-stop clinic and 173 (61. 8%) after initiation of the one-stop clinic. The majority of these surgeries were under general surgery 131 (46.8%), followed by ophthalmology surgery 81 (28.9%) and ENT surgery 68 (24.3%) [Table1].
However, after Comparing three months before (December 2019, January 2020, and February 2020) with 3 months after (December 2020, January 2021, and February 2021), the total number of surgeries was significantly higher in the pretest group P-value 0.0003.
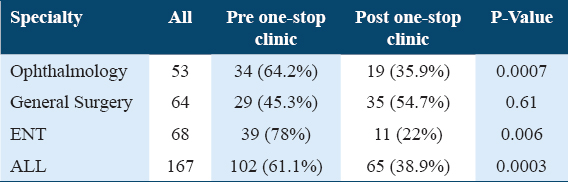
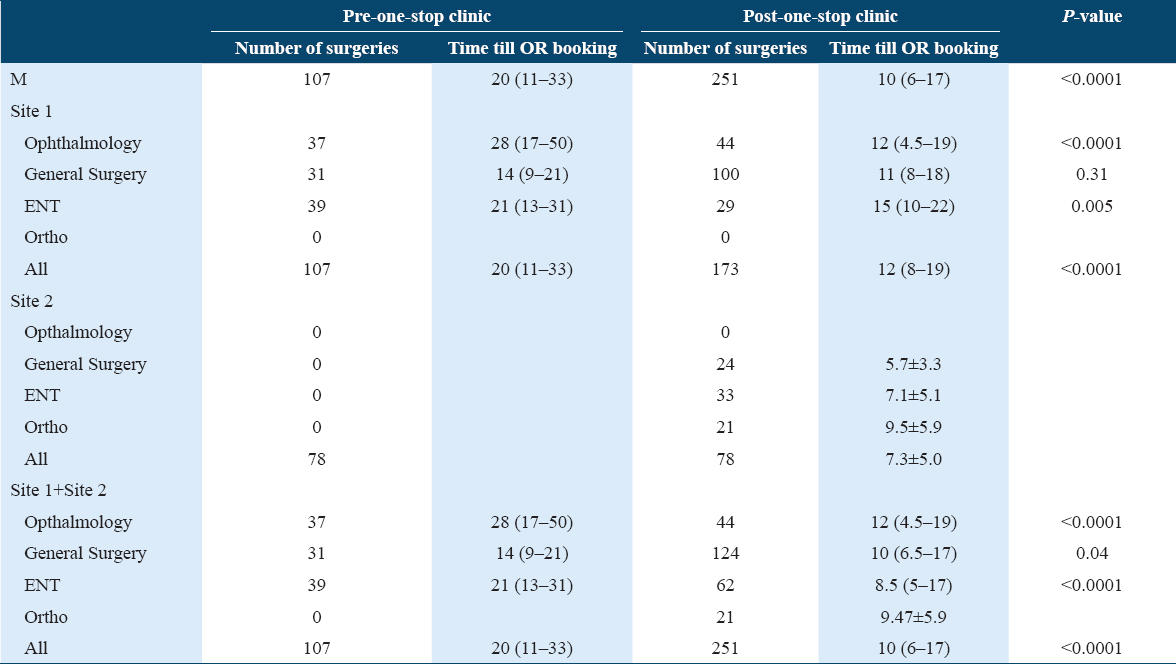
The median (quartile Q1, Q3) time elapsed from the first seen day until the booked OR day post-one-stop clinic 10 (6–17) was significantly lower than pre-one-stop clinic 20 (11–33), P < 0.0001 [Table 2]. Similarly, in site one, the median (quartile Q1, Q3) time elapsed from the first seen day until the booked OR day of post-one-stop clinic 12 (8–19) was significantly lower than pre-one-stop clinic 20 (11–33), P < 0.0001. Furthermore, for the subgroups, the median time elapsed from first seen day until the booked OR day was lower in ophthalmology surgeries (28 [17–50] vs. 12 ([.5–19], P < 0.0001), general surgeries (14 [9–21] vs. 11 [8–18], P-value 0.31) and ENT surgeries (21 [13–31] vs. 15 [10–22], P-value 0.005) after the initiation of the one-stop clinic [Table 3]. The average monthly time elapsed from the first seen day until the booked OR day pre and post-one-stop clinic are shown in [Figure 2].
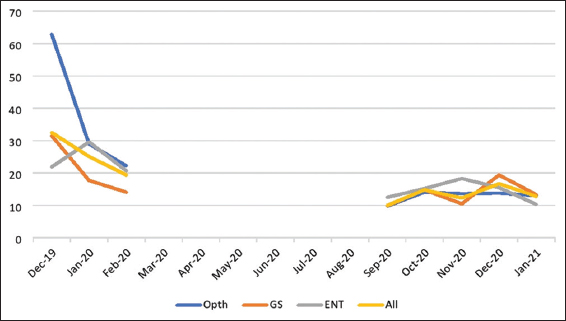
- The time elapsed from first seen day until the booked OR day pre- and post-one-stop clinic
Discussion
This study investigated the effect of a one-stop clinic’s application as a care model on the clearance of the COVID-19 surgical backlog. We measured the number of surgeries and the time elapsed from the 1st day seen until the booked OR day before and after the one-stop clinic initiation. Our results revealed that the time elapsed from the 1st day seen until the booked OR day was lower after initiating the one-stop clinic.
The one-stop clinic may reduce the surgical backlog during COVID-19 and limit patients’ exposure to more hospital visits, which in turn may reduce infections exposures, reduce the cost, and increase patients’ satisfaction.[8,15] Although the one-stop is not a new model, the studies that assess its effect on surgical backlog due to COVID-19 are limited. A one-stop clinic approach was adopted in the United Kingdom for plastic surgeries during the COVID-19 pandemic.[15,16] It showed positive outcomes, encouraging them to continue this approach with the extreme resource limitation.[15,16]
Away from the COVID-19 pandemic, several studies have advocated introducing one-stop clinics. A local national survey in the United Kingdom showed that around 95% were satisfied with and preferred the one-stop clinic approach compared to conventional service.[8] From a non-compliant mean of 80% to a compliant 95%, the one-stop clinic improved the waiting times. Besides, the capability of the department grew by 15%.[8] Javaid et al. described their experience in using this approach in plastic surgery. They concluded that these clinics were cost-effective and effectively reduced the burden in a routine clinic and allowed more patients with major serious problems to be seen earlier.[9] In 2011, Páez et al. reported that a one-stop clinic was feasible for various procedures in a urological ambulatory clinic.[10] Similarly, Voorbrood et al. revealed that applying the one-stop clinic for endoscopic hernia surgery was effective, with a patient satisfaction score of 9 out of 10.[11]
Study results should be interpreted in light of their strengths and limitations. This study is from the few studies that examined the effect of implementing the one-stop clinic on the surgical backlog due to the COVID-19 pandemic. Besides, it is from the few studies that involved multiple surgical specialties. This study’s limitation includes the quasi-experimental design’s known weaknesses, such as lack of randomization and control group, limiting its ability to conclude causal association. In addition, this study did not control possible confounders that can affect the waiting time for surgery, such as the availability of instrumentations, number of surgeons, number of anesthesia, bed capacity, and limitation of supplies. Further, we did not measure the patients’ satisfaction and aspects of post-operative care, cost, quality of care, and outcomes. We recommend considering these measures in future researches.
Conclusion
This study has shown that one-stop clinics might help recruit the patients on the waiting list quickly, shorten the period between first visit and booking in the operating room. After considering the limitations of this study, we recommend studying the one-stop clinic’s effect on patient satisfaction and surgeries outcome.
Authors’ Declaration Statements
Ethics approval and consent to participate
Permission from the hospitals under investigation was obtained in order to conduct this study. Data were gathered in each hospital by each collaborator and given to the researchers for review and statistical analysis. This study was ethically approved by the institutional review board of King Fahad Medical City in Riyadh, Saudi Arabia.
Availability of data and material
All data generated and/or analyzed during this study included in this published article. The data are available from the corresponding author upon request.
Competing interests
The authors declare no conflict of interest
Funding statement
This research received no specific grant from public, commercial, or non-profit funding agencies.
Authors’ contributions
The research team designed and led the design of the study and the preparation of the article; also carried out data extraction, analysis and carried out a systematic review of the literature for data retrieval. The final version of this manuscript was read and approved by all authors. Before submission, all listed authors have approved the manuscript, including the names and data included and the graphs. All of the writers got input and helped shape the research, review, and manuscript.
Acknowledgments
The authors would like to express their gratitude to King Fahad Medical City, Research Center and the Northern Business Unit in Health Holding Company for their technical assistance.
ORCID link of the submitting author: ORCID iD: http://orcid.org/0000-0003-1388-4549
References
- 2019. Coronavirus Disease (COVID-19). Geneva: World Health Organization; https: //www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19#:~:text=symptoms
- 2020. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 11 March 2020. Geneva: World Health Organization; https: //www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- SARS-CoV-2 impact on elective orthopaedic surgery:Implications for post-pandemic recovery. J Bone Joint Surg Am. 2020;102:e68.
- [Google Scholar]
- Clearing the surgical backlog caused by COVID-19 in Ontario:A time series modelling study. CMAJ. 2020;192:E1347-56.
- [Google Scholar]
- Hospitals and Health Systems Face Unprecedented Financial Pressures Due to COVID-19. Available from: https://www.aha.org/system/files/media/file/2020/05/aha-covid19-financial-impact-0520-FINAL.pdf
- [Google Scholar]
- A pigmented lesion clinic:Analysis of the first year's 1055 patients. Br J Plast Surg. 1995;48:247-51.
- [Google Scholar]
- One-stop clinic utilization in plastic surgery:Our local experience and the results of a UK-wide national survey. Plast Surg Int. 2015;2015:747961.
- [Google Scholar]
- The see-and-treat clinic in plastic surgery:An efficient, cost-effective, and training-friendly setup. Plast Reconstr Surg. 2004;113:1060-3.
- [Google Scholar]
- The one-stop clinic as the standard of out-patient care in a hospital urology department. Int Braz J Urol. 2011;37:623-9.
- [Google Scholar]
- One-stop endoscopic hernia surgery:efficient and satisfactory. Hernia. 2015;19:395-400.
- [Google Scholar]
- Seven Ways To No Delays. Available from: https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/Seven-Ways-to-No-Delay.pdf
- Population and Demography. Available from: https://www.stats.gov.sa/en/1006
- Hospitals and Beds in KSA Health Sectors by Region, 2019G. Statistical Yearbook 2019. Kingdom of Saudi Arabia 2020
- [Google Scholar]
- Managing hand trauma during the COVID-19 pandemic using a one-stop clinic. J Plast Reconstr Aesthet Surg. 2020;73:1357-404.
- [Google Scholar]
- Percutaneous needle fasciotomy for Dupuytren's disease:A one-stop approach incidentally suited to the era of COVID-19. J Plast Reconstr Aesthet Surg. 2020;73:2086-102.
- [Google Scholar]







