Translate this page into:
Isolated benign neutropenia in healthy individuals from Saudi Arabia’s central region: A comprehensive study
Address for correspondence: Ahmad AlShomar, Department of Medicine, College of Medicine, Qassim University, Buraidah, Qassim, Saudi Arabia. E-mail: a.alshomar@qu.edu.sa
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
ABSTRACT
Objectives:
Neutrophils are the most common cell types in circulation and are considered the first line of defense in the immune system against microorganisms. This study was undertaken to investigate the occurrence of isolated benign neutropenia (IBN) among healthy individuals in the central region of Saudi Arabia.
Methods:
This retrospective study analyzed complete blood count tests as part of routine checkups for chronic health conditions from April to September 2022. The 10,442 participants were randomly selected and their medical records were reviewed for neutropenia and mean absolute neutrophil counts (ANCs) were calculated. Descriptive analysis was employed to assess the prevalence of IBN across various demographic factors, such as age, gender, and nationality.
Results:
The prevalence of IBN in the central region of Saudi Arabia was found to be 2.82% across the entire cohort of participants. The mean ANC among all participants was 4.55 × 109/L. The prevalence of neutropenia was higher in male participants compared with female. Male neutropenic had a lower mean ANC than female; however, the differences were not statistically different (P > 0.05). The prevalence of neutropenia was lower in Saudi participants compared with non-Saudis. While the mean ANC was lower among Saudis as compared with non-Saudi participants. However, the differences were not statistically different (P > 0.05).
Conclusion:
This is the first study from the central region of Saudi Arabia that determined the prevalence of chronic benign neutropenia among healthy individuals. The prevalence of IBN was found to be relatively low. Furthermore, neutropenia was more frequent in males than females. Moreover, male neutropenic individuals have a lower ANC.
Keywords
Absolute neutrophil count
ethnicity
neutropenia
neutrophils
Saudi Arabia
Introduction
Neutrophils are the first line of defense in the immune system against microorganisms.[1] Neutropenia is a frequently encountered medical condition defined by a decrease in the absolute neutrophil count (ANC) to the lower threshold of the normal range, which varies by age and racial background. The World Health Organization has adopted an ANC threshold of 1.8 × 109/L for the definition of neutropenia in European adults.[2] Neutropenia can be classified based on degree of severity: mild when ANC is between 1.0 and 1.5 × 109/L, moderate when ANC is 0.5–1.0 × 109/L, and severe when ANC is <0.5 × 109/L.[3,4] Agranulocytosis is a serious condition associated with the risk of severe, life-threatening infections, and occurs when ANC <0.2 × 109/L.[4] Moreover, neutropenia can be categorized as either congenital or acquired, besides being acute or chronic. Neutropenia is a key infection risk factor.[4] Cancer patients receiving chemotherapy are more susceptible to neutropenia and infection.[5] Fever during a period of severe neutropenia (ANC <0.5 × 109/L) is referred to as febrile neutropenia.[5]
It is notable that certain people of African and Middle Eastern ethnicity, who have routine testing, exhibit a normal range of ANCs between 0.5 and 1.5 × 109/L.[6] This particular variation is referred to as benign ethnic neutropenia (BEN) or benign neutropenia (BN).[6] It is not linked to any clear disease burden and does not pose an increased risk of infection.[7] It affects 25–50% of people from Africa and the Middle East.[8] Saudi Arabia occupies a large portion of the Arabian Peninsula, has an area of around 2,150,000 km2, and has a population of 32.175 million people. Saudi citizens represent 58.4% of the population, while non-Saudis represent the remainder at 41.6% (As per the General Authority for Statistics, 2023). The prevalence of BN in the central region of Saudi Arabia is not well described. A study estimated the prevalence of BN in Jeddah, Saudi Arabia, to be 20%, with an average ANC of 1.48 × 109/L, with Saudis having a significantly higher prevalence of BN than non-Saudis.[9] A previous study found the prevalence of BN in southern and southwest Saudi Arabia to range from 11% to 23%.[10] Alqahtani performed a study that revealed that the prevalence of BN in the southern and western regions of Saudi Arabia varied between 19% and 35%.[11] The prevalence of BN shows variation among gender and smoking status, with males being more prone to BN and smoking being associated with higher ANC risk.[12]
Simply attributing the cause of neutropenia to BN could have a major impact on clinical practice. BN in healthy Africans may result in an incorrect lowering or delaying of the chemotherapy medication dose in cancer patients, leading to a suboptimal outcome. African American women, for example, have better survival in breast cancer than white women because they receive less intensive chemotherapy and a longer treatment duration since they have a lower baseline ANC.[13] Clozapine, an antipsychotic medication that frequently induces neutropenia, is more likely to be suspended in blacks than whites.[14] Furthermore, blacks are less likely to use clozapine due to agranulocytosis-related concerns.[15] Other concerns can arise in patients who have BN, such as the improper administration of antibiotics to treat febrile viral diseases and unnecessary invasive hematological procedures, such as bone marrow biopsies.
The study aimed to evaluate the prevalence of isolated BN among healthy participants in the central region of Saudi Arabia. A comparative analysis was conducted to evaluate the mean ANC and the prevalence of BN across different demographic factors such as age, gender, and nationality.
Materials and Methods
Patients and study design
In this retrospective study, we evaluated the medical records of participants aged between 18 and 55 who had complete blood count tests as part of regular check-up or follow-up care for chronic health issues in an outpatient setting at Dr. Sulaiman Al-Habib Hospital in Saudi Arabia, Al Qassim region. There were no restrictions on gender or body mass index. Laboratory testing was conducted between April and September 2022, and participants were chosen randomly from men and women. The total number of participants who were first screened was 28717 [Figure 1]. The final analysis included 10,442 participants after excluding those who were outside the age limit, had abnormal hemoglobin or platelets, had an abnormal biochemical profile, or did not meet other criteria. We defined neutropenia at ANC <1.5 × 109/L. The medical records of patients with neutropenia <1.5 × 109/L were reviewed to obtain demographic information. Exclusion criteria were used to rule out any pre-existing health conditions that could contribute to neutropenia, such as patients with malignancies or rheumatological disorders and patients who have already received chemotherapy or radiation therapy. The following exclusion criteria were used to estimate the white blood cell (WBC) reference range: “Any significant abnormalities in the renal or liver tests, hemoglobin levels of <11 g/dL or >18 g/dL, thrombocytopenia (<150 × 109/L), platelet counts >450 × 109/L, and WBCs >11 × 109/L were ruled out.
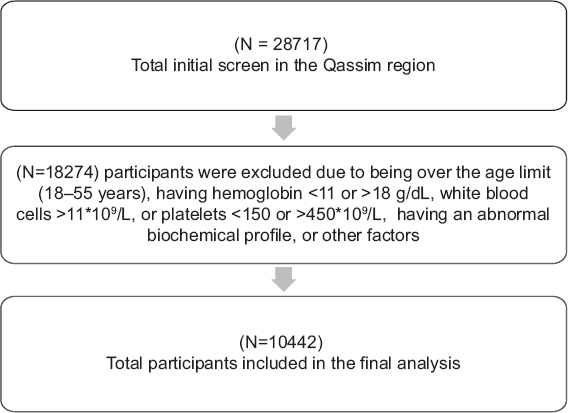
- Flowchart of participant screening and exclusion
Blood extraction began by cleaning the skin with an antiseptic solution, followed by tightening a tourniquet around the upper arm to point out the vein. After that, a needle was inserted to extract 4 mL of fresh whole blood into anticoagulated tubes containing Ethylenediamine tetraacetic acid, which was processed within 4 h of collection. The extraction area was bandaged to stop any bleeding. The extracted blood was bottled, got a label sample, and was submitted to a laboratory for analysis. We utilized the CELL-DYN Ruby system, which is an automated hematology analyzer with numerous parameters designed for in vitro diagnostics in clinical laboratories. To determine Red Blood Cells (RBCs), WBCs, and platelets, the used equipment was (Multi-Angle Polarized Scatter Separation) technology with laser flow cytometry.
Statistical analysis
Before being imported into an Excel datasheet, the patient’s data were de-identified for any identifying information. After extraction, the data were revised, coded, transferred, and analyzed using the Statistical Package for the Social Sciences, version 26 (SPSS, IBM, TX, USA). The data had been verified for accuracy and missing information. All scale parameters were subjected to a normal distribution analysis. Data for gender, nationality, and age were stratified into two groups: male and female, Saudi and non-Saudi, young adults (18–30 years old), and middle-aged adults (31–55 years old), respectively. Descriptive analyses using the mean, median (range), and standard deviation were utilized to assess the prevalence of neutropenia in the selected participants. P < 0.05 was considered statistically significant at a 95% confidence interval.
Ethical approval
The Research Ethics Committee of the Al-Habib Research Center in Saudi Arabia granted ethical approval with study number RC23.05.11. All personal information about participants were kept confidential. The Research Ethics Committee waived the participants’ consent due to the use of completely anonymized data with no associated harm. All procedures performed and patient confidentiality were carried out in compliance with the institution’s ethical standards, the national research committee in KSA, and the Helsinki Declaration.
Results
The final analysis included 10,442 participants, 68% males and 32% females, while 92.77% were Saudis and 7.23% were non-Saudis. About 64.63% of the participants were between the ages of 31 and 55, while 35.36% were between the ages of 18 and 30. The mean age among all participants was 35 ± 9.2, and the mean ANC was 4.55 ± 1.8. Table 1 summarizes the demographic data (gender, age, and nationality) of all participants and neutropenic patients.
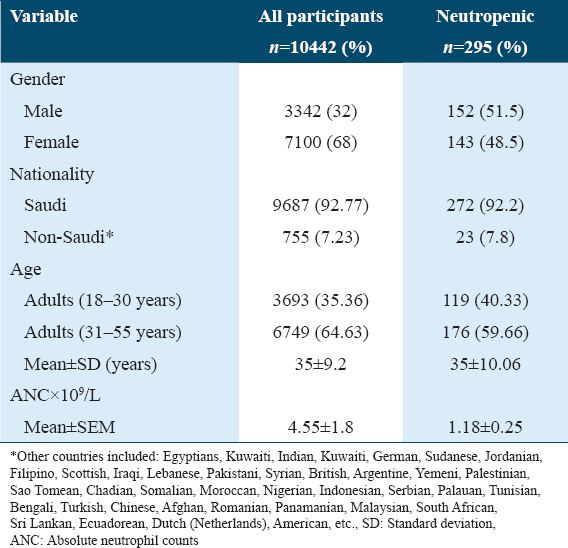
The prevalence of neutropenia was found to be 2.82% across the entire cohort of participants, with most neutropenic participants having mild (78%) or moderate neutropenia (19%). The prevalence of neutropenia was 4.5% in male participants and 2% in female participants. The prevalence of neutropenia was 2.8% in Saudi participants and 3% in non-Saudi participants. The gender distribution among neutropenic participants was 51.5% male and 48.5% female. Most of the neutropenic participants were of Saudi nationality (92.2%), while the remaining were non-Saudi (7.8%). The mean age among neutropenic participants was 35 ± 10.06, and their mean ANC was 1.18 ± 0.25.
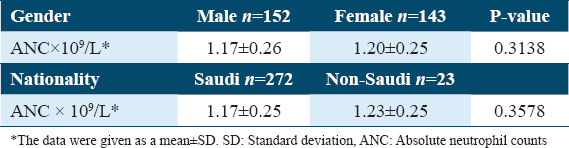
The mean ANC among male neutropenic participants was lower (1.17 ± 0.26) than female participants (1.20 ± 0.25); however, the differences were not statistically different (P = 0.3138). The mean ANC among Saudi neutropenic participants was lower (1.17 ± 0.25) than non-Saudi participants (1.23 ± 0.25); however, the differences were not statistically different (P = 0.3578) [Table 2].
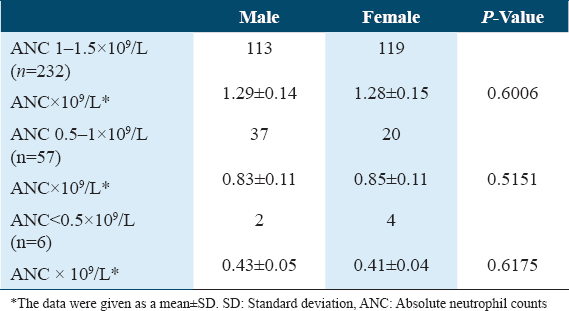
The mean values of the neutropenic participants were separated into three groups based on gender and degree of neutropenia (mild ANC 1–1.5 × 109/L, moderate ANC 0.5–1 × 109/L, and severe ANC <0.5 × 109/L) [Table 3]. There were no statistically significant differences between the male and female groups concerning neutropenia degree (mild, moderate, and severe).
Discussion
The prevalence of isolated neutropenia in Saudi Arabs was not well established. To the best of our knowledge, this is the first study from the central region of Saudi Arabia that assesses the prevalence of isolated neutropenia. The final analysis of this study included 10,442 participants after excluding non-eligible participants. The prevalence of BN varies from region to region worldwide, as well as within Saudi Arabia. We think that the most likely cause of this isolated neutropenia is BEN. The present study revealed that the prevalence of isolated BN in the central region of Saudi Arabia was found to be 2.82% across the entire cohort of participants, with a mean ANC among all participants of 4.55 × 109/L.
We found a lower mean ANC in Saudi neutropenic participants (1.17 × 109/L) compared to non-Saudi participants (1.23 × 109/L); however, the differences were not statistically different. This finding suggests that BEN is more prevalent among specific ethnic groups. Consanguineous marriages are prevalent in Saudi Arabia, which could explain why BN has a higher prevalence in Saudi Arabia compared to non-Saudi participants. The average ANC in the black-American population is lower than that of the Caucasian and Mexican-American populations.[12] This difference could be explained by ethnic variation.
Our findings are significantly lower than those demonstrated in a previous study by Alqahtani, who reported that the prevalence of BN varied between 19% and 35% in the southern and western parts of Saudi Arabia.[11] The possible explanations for this high frequency are altitude factors (the southern region is 2200 m above sea level) and underlying ethnic neutropenia. We found a much lower value of neutropenia concerning those reported by Awan et al., who found the prevalence of BN in southern and southwest Saudi Arabia to range from 11% to 23%.[10] The present study contradicted prior research in Jeddah, through the western region of Saudi Arabia, which estimated the prevalence of BN to be 20% with an average ANC of 1.48 × 109/L.[9] The close location of the southern and western regions of Saudi Arabia to the African continent may also contribute to the migration of African-origin populations to the Arabian Peninsula, which may explain the higher prevalence of neutropenia in these parts of the country.
Our results are consistent with the previous results in which the prevalence of neutropenia varied among genders, with males being more prone to neutropenia and being associated with a lower ANC.[12]
The association between the BEN and a genetic deletion of the Duffy antigen receptor for chemokines (null genotype) has been widely recognized. This genotype, which is the consequence of a single-nucleotide polymorphism, is believed to confer an advantage in malaria protection.[6] The Duffy-null phenotype (Fy a-b-) was found to be around 61% popular in Saudi Arabia. Therefore, Duffy-null phenotype-induced BEN may be contributing to the reported cases of isolated neutropenia in Saudi Arabia.[16] The lack of Duffy antigen in blood groupings can be utilized to assess the presence of BEN. If established, this will provide a simple method for diagnosing BEN in the appropriate clinical setting without comprehensive testing.[17]
Most general practitioners assume isolated mild neutropenia to be a serious illness when treating patients in the primary care setting; nevertheless, benign causes of neutropenia are more likely to be the etiology.[18] In patients with BEN, a bone marrow biopsy and aspiration reveal normal cellularity and leukocyte maturation.[19] The long-term prognosis is favorable, and there appears to be no risk of developing an infection.[20] Chronic, isolated mild neutropenia is exceedingly unlikely to result in serious diagnoses, such as hematological malignancies.[21] Patients with isolated neutropenia frequently have comprehensive laboratory investigations, including invasive procedures such as bone marrow biopsy, without any clear diagnosis. Despite that, the appropriate approach to neutropenic outpatients can be established in the appropriate clinical context.[4] The presence of stable, isolated mild-to-moderate neutropenia in patients of African or Middle Eastern ethnicity in an outpatient setting without a history of recurrent or severe infection with a normal physical examination and the absence of alarming findings in blood films all support the diagnosis of BEN.[7] Severe congenital neutropenia is typically diagnosed in childhood and is characterized by severe neutropenia, an increased risk of infections, extra-hematological features, and a higher risk of developing acute leukemia.[22] Cyclic neutropenia is caused by mutations in the ELANE gene, a rare cause of neutropenia characterized by recurrent aphthous ulcers, and/or infections as well as a fluctuation in neutrophil count every 3 weeks.[23]
The findings of this study should help clinicians understand the magnitude of isolated BN in our population. To avoid a significant impact on clinical practice by attributing neutropenia in our populations to BEN, longer-term follow-up and further prospective studies are required. Nevertheless, the present study has several limitations, including the fact that it was conducted in a single center, making it difficult to extrapolate results to the whole central area of Saudi Arabia. Furthermore, we evaluated the ANC value using single measurements; hence, the fluctuations over time in the ANC could not be confirmed.
Conclusion
The findings of this study indicate that the prevalence of isolated BN in the central region of Saudi Arabia was lower than anticipated. The practical implications of these findings remain to be determined; however, we recommend that clinicians review the patient’s age, ethnicity, and clinical setting when assessing the need for a diagnostic workup for neutropenia.
Author’s Declaration Statements
The author declare no conflicts of interests.
Ethical Approval and Patients Consent
The Research Ethics Committee of the Al Habib Research Center in Saudi Arabia granted the ethical approval with study number of RC23.05.11. All personal information about participants was kept confidential. The Research Ethics Committee waived the participants consent due to the use of completely anonymized data with no associated harm. All procedures performed and patient confidentiality was carried out in compliance with the Institution’s Ethical Standards, the National Research Committee in KSA, and the Helsinki Declaration.
Consent for Publication
Not applicable.
Availability of Data
All data and materials used in this present study are available from the corresponding author on reasonable request.
Competing Interest
The authors declare that they have no conflicts of interest.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contribution
AA contributed to the design of the study, the interpretation of the data, data collection, analysis, and manuscript writing.
Acknowledgments
The authors would like to thankful to Dr.Sulaiman Al Habib Medical Group’s Research Centre for their tremendous support, and all patients that participated are also gratefully acknowledged.
References
- Neutrophil:A cell with many roles in inflammation or several cell types? Front Physiol. 2018;9:113.
- [Google Scholar]
- The 5th edition of the World Health Organization classification of haematolymphoid tumours:Myeloid and histiocytic/dendritic neoplasms. Leukemia. 2022;36:1703-19.
- [Google Scholar]
- Evaluation and management of patients with isolated neutropenia. Semin Hematol. 2013;50:198-206.
- [Google Scholar]
- The European guidelines on diagnosis and management of neutropenia in adults and children:A consensus between the European hematology association and the EuNet-INNOCHRON COST action. Hemasphere. 2023;7:E872.
- [Google Scholar]
- Optimal management of neutropenic fever in patients with cancer. J Oncol Pract. 2019;15:19-24.
- [Google Scholar]
- Ethnic benign neutropenia:A phenomenon finds an explanation. Pediatr Blood Cancer. 2018;65:e27361.
- [Google Scholar]
- Benign ethnic neutropenia:What is a normal absolute neutrophil count? J Lab Clin Med. 1999;133:15-22.
- [Google Scholar]
- Incidence and potential causative factors associated with chronic benign neutropenia in the Kingdom of Saudi Arabia. BMC Proc. 2015;9(Suppl 2):S1.
- [Google Scholar]
- Isolated neutropenia/benign ethnic neutropenia:A common clinical and laboratory finding in southern and Western Saudi Arabia. Int J Gen Med. 2021;14:451-7.
- [Google Scholar]
- Prevalence of neutropenia discovered in routine complete blood cell counts among healthy adults from Saudi Arabia at different altitudes. J Pharm Negat Results. 2022;13:1454-8.
- [Google Scholar]
- Prevalence of neutropenia in the US population:Age, sex, smoking status, and ethnic differences. Ann Intern Med. 2007;146:486-92.
- [Google Scholar]
- Ethnic neutropenia and treatment delay in African American women undergoing chemotherapy for early-stage breast cancer. J Natl Cancer Inst. 2003;95:1545-8.
- [Google Scholar]
- Clozapine underutilization and discontinuation in African Americans due to leucopenia. Schizophr Bull. 2007;33:1221-4.
- [Google Scholar]
- Racial disparities in antipsychotic prescription patterns for patients with schizophrenia. Am J Psychiatry. 2002;159:567-72.
- [Google Scholar]
- Phenotype frequencies of major blood group systems (Rh, Kell, Kidd, Duffy, MNS, P, Lewis, and Lutheran) among blood donors in the eastern region of Saudi Arabia. J Blood Med. 2020;11:59-65.
- [Google Scholar]
- Duffy antigen phenotyping is a useful and clinically available test for benign ethnic neutropenia. Blood. 2018;132:2546.
- [Google Scholar]
- Hematology referrals for leukopenia in the bronx rarely result in clinically significant diagnoses:First steps towards and evidence-based referral guideline. Blood. 2016;128:4743.
- [Google Scholar]
- Bone marrow granulocyte reserve in chronic benign idiopathic neutropenia. Clin Lab Haematol. 1987;9:281-8.
- [Google Scholar]
- Natural history of benign ethnic neutropenia in individuals of African ancestry. Blood Cells Mol Dis. 2019;77:12-6.
- [Google Scholar]
- Age-related prevalence and clinical significance of neutropenia-isolated or combined with other cytopenias:Real world data from 373 820 primary care individuals. Am J Hematol. 2020;95:521-8.
- [Google Scholar]
- Congenital neutropenia in the era of genomics:Classification, diagnosis, and natural history. Br J Haematol. 2017;179:557-74.
- [Google Scholar]
- The diversity of mutations and clinical outcomes for ELANE-associated neutropenia. Curr Opin Hematol. 2015;22:3-11.
- [Google Scholar]







