Translate this page into:
Parents as coronavirus disease-19 carriers in intrafamily settings: Cases of severe forms in a family cluster
Address for correspondence: Hyppolite K. Tchidjou, Pediatric Emergency Services, Amiens University Hospital, 1 Rue du Professeur Christian Cabrol, 80054 Amiens-France. Phone: +33 0322087550. Fax: +33 0322089665. E-mail: tchidjoukuekou.hyppolite@chu-amiens.fr
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The outbreak of coronavirus disease-19 (COVID-19) infection that started in China in December 2019 has subsequently spread too many countries worldwide with high contagiousness. Given the spread and the current debate on the management and origin of intrafamilial clusters of COVID-19, this case highlights how essential it has become to prompt quarantine for the whole family and any contact member who may be at risk of infection. For this, the management of family clusters requires specific guidelines that need to be prepared to help clinicians and families to better face the disease, especially the risk of developing severe forms. We reported a case and the management of severe forms of COVID-19 infection in an intrafamily cluster with different child and parent outcomes.
Keywords
Children
coronavirus disease-19 infection
family cluster
liver injury
treatment
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is one of the seven coronaviruses known to infect humans.[1,2] It is now known that SARS-CoV-2 infection due to coronavirus disease-19 (COVID-19) is highly contagious with a high mortality rate and caused varying degrees of illness throughout the world.[2-4] The symptoms of COVID-19 are similar in children and in adults.[3] Pediatric cases are mainly family cluster cases that have epidemiological links to adult patients. However, children with COVID-19 generally have milder illness and rarely require treatment at a hospital.[5,6]
Care for most COVID-19 patients is home based and consists of supportive treatment for fever and mild associated symptoms.[7] For a minority of children who will become critically ill, hospitalization may be needed for supplemental oxygen inhalation therapy or invasive ventilation and sometimes drugs must be used.[7-9]
We reported a case of SARS-CoV-2 in an intrafamily cluster in France where the children had different outcomes, especially a 16-year-old girl without medical history, with severe respiratory symptoms due to SARS-CoV-2 infection requiring intensive care unit (ICU) treatments.
Case Report
On April 2, 2020, a 16-year-old girl was admitted to Creil Regional Hospital, France, and immediately placed in quarantine ward because she had been in a close contact with her family members [Figure 1] who were COVID-19 positive.
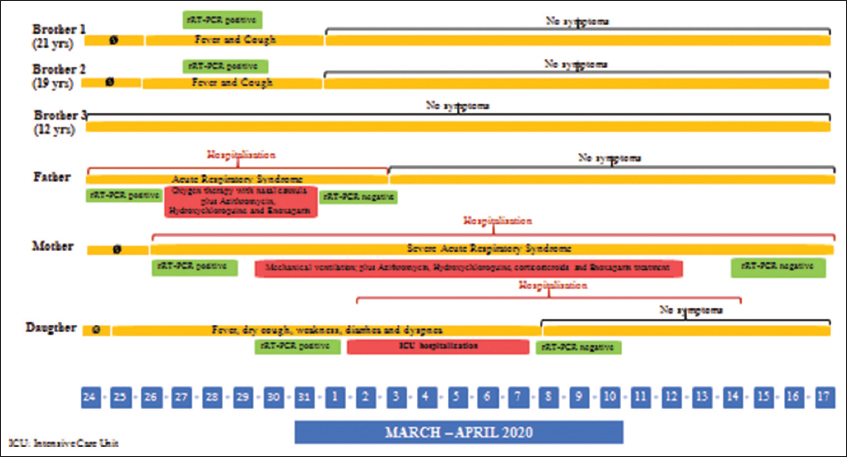
- Timeline of exposure and symptoms of the intrafamily cluster with COVID-19
At admission, the patient had axillary temperature of 39°C and mild dyspnea (oxygen saturation [SaO2] of 96%, respiratory rate of 30 breaths per minute). In accordance with the French guidelines, we performed nasopharyngeal swabs, chest tomography, and laboratory tests.
We investigated the source of the patient’s infection [Figure 1: Timeline of exposure and symptoms of the family cluster with COVID-19]. The patient lives in a household with her parents and three brothers (who are, respectively, 21-year-old, 19-year-old, and 12-year-old boy). On March 24, the father, a restaurant employee, presented fever, cough, chest pain, dyspnea, and asthenia, and was admitted to Creil Hospital with a diagnosis of COVID-19 infection associated with acute respiratory syndrome and required oxygen therapy with a flexible nasal cannula for a few days (from March 26 to 31), in addition to enoxaparin, azithromycin, and hydroxychloroquine treatment. On March 26, the mother presented the same symptoms and was also admitted to Creil Hospital with a diagnosis of severe acute respiratory syndrome due to COVID-19 (SARS-CoV-2) requiring mechanical ventilation and supportive measures in ICU until mid-April (from March 27 to April 14) in addition to enoxaparin, azithromycin, hydroxychloroquine, and corticosteroids treatment. The two brothers aged 21 and 19 only had dry cough and fever for 3 days, with normal respiratory and vital signs, and were tested positive on March 28. The youngest brother aged 12 never had any symptoms; he had received a few month earlier diphtheria, tetanus, poliomyelitis, and pertussis vaccines.
On April 3, the computerized tomography scanner of patient showed bilateral air space opacities and confluent areas of ground-glass attenuation dispersed in the peripheral regions of the lungs; nasopharyngeal swabs tested positive for SARS-CoV-2 infection with real-time reverse transcription polymerase chain reaction (rRT-PCR) assay. Laboratory tests revealed a C-reactive protein 30.1 mg/L (normal range [n.r.] <5 mg/L) and blood routine tests, liver and renal function, myocardial enzymes, D-dimer levels, and electrolytes were normal.
Due to severe dyspnea and progressive worsening of symptoms, SaO2 89% and respiratory rate of 30 breaths per min, oxygenation was administered through a flexible nasal cannula (flows of 5 L/min) and the patient was transferred to the ICU of University Hospital of Amiens [Figure 2].
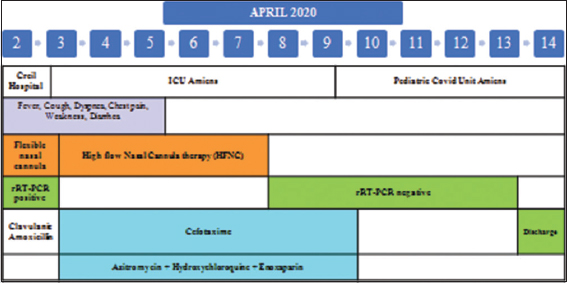
- Symptoms and management of adolescent with severe form during hospitalization to Creil Hospital and Amiens University Hospital, April 2–14, 2020
At admission, the patient had severe dyspnea, was alert but exhausted, with chest pain, an axillary temperature of 39°5C and a respiratory rate of 41 breaths per min, SaO2 94–96% with 5 L/min oxygen, PaO2: 70, and an oxygenation index of 233 mmHg. The patient actively received the high-flow nasal cannula therapy, at a rate of 50 L/min with a FiO2 of 30% and was treated with hydroxychloroquine, dexamethasone, enoxaparin, and cefotaxime.
A nasopharyngeal swab specimen was obtained to detect influenza type A and B by rapid test, respiratory syncytial virus, rhinovirus, adenovirus, human metapneumovirus, mycoplasma, and Chlamydophila pneumoniae, Bordetella pertussis, and Legionella pneumophila by RT-PCR and they were all negative; furthermore, immunological markers (humoral and cellular immunity) were normal and a blood sample was obtained for culture and all the results were negative.
Three days after admission, the patient’s clinical condition improved, supplemental oxygen was discontinued on illness day 5 and her SaO2 improved to 98% under ambient air. According to the French guidelines, laboratory routine tests including liver enzymes were performed and revealed alanine aminotransferase (ALAT) 158 U/L (n.r. 10–35 U/L) and aspartate aminotransferase (AST) 109 U/L (n.r. 10–35 U/L); hydroxychloroquine dosage was 0.54 mg/mL (n.r. 0.3–2 mg/mL). Blood routine tests, renal function values were normal.
On illness day 6, given the patient’s clinical improvement, she was transferred from ICU to the COVID-19 pediatric unit for monitoring. The final results of subsequent nasopharyngeal swab and of stool test for SARS-CoV-2 by rRT-PCR assay were negative. Given the slight increased transaminase values; on suspicion of slight liver dysfunction, all current medications were discontinued.
On April 14, given the good health conditions and the normal results of microbiological tests and blood tests (AST 38 U/L, ALAT 64, and C-reactive protein 1.6 mg/L on the last control), the patient was discharged with home monitoring indications for the next 2 weeks.
Case Discussion and Conclusion
Clinical data of SARS-COV-2 infection and management of intrafamily clusters are still very limited. Regarding children and immunizations, most children have good immunization coverage to several microorganisms, especially of a viral nature. One of the hypotheses under discussion to explain the reduced severity of SARS-CoV-2 infection is that vaccines stimulate cross-immunity, which is partially protective against other microorganisms, and that, by extension, they could protect against COVID-19 or reduce the severity of its presentation.[10,11]
Furthermore, since COVID-19 could increase liver enzymes, the physicians should keep in mind that for patients with SARS-CoV-2 infection, monitoring of liver enzymes is always important, especially if the patient must start drugs that might have a potential hepatotoxicity.[12,13]
Given the spread and the current debate on the origin of intrafamilial clusters of COVID-19 throughout the world, this case highlights how essential it has become to prompt quarantine for the whole family and for all the contact members who may be at risk of infection, with the aim of reducing the diffusion of family outbreaks.
Finally, this case also might help clinicians to identify the clinical characteristics and specific therapeutic approaches, especially in family clusters with severe or moderate respiratory symptoms sometimes associated with slight liver dysfunction due to COVID-19-related hyperinflammatory reactions.
Authors’ Declaration Statements
Patient’s consent
Written consent was taken from the studied patient
Data availability
The data are available with the corresponding author and will be produced on personal request.
Competing interest
The other authors have no conflicts of interest to disclose.
Funding
The authors have no support or funding to report and the remaining authors have no financial relationships relevant to this case report to disclose.
Authors’ contributions
All authors contributed equally.
Acknowledgments
We want to thank the patient who participated in this study. We thank Dr. Charlene Temps, Dr. Yannick Ricard, Dr. Pauline Desbureaux, Dr. Fiorella Caron, Dr. Adeline Ferec, Dr. Cécile Grenenko, and nurses for support in patient management.
References
- COVID-19:Lost opportunities and lessons for the future. Int J Health Sci (Qassim). 2020;14:4-6.
- [Google Scholar]
- Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323:1574-81.
- [Google Scholar]
- Coronavirus disease-19 spread in the Eastern Mediterranean region, updates and prediction of disease progression in Kingdom of Saudi Arabia, Iran, and Pakistan. Int J Health Sci (Qassim). 2020;14:32-42.
- [Google Scholar]
- Clinical analysis of 25 COVID-19 infections in children. Pediatr Infect Dis J. 2020;39:e100-3.
- [Google Scholar]
- Corona virus disease, a growing threat to children? J Infect Public Health. 2020;13:883-6.
- [Google Scholar]
- 2020. Centers for Disease Control and Prevention. Atlanta, Georgia, United States: CDC; Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/therapeutic-options.html
- COVID-19 in children:Clinical approach and management. Indian J Pediatr. 2020;87:433-42.
- [Google Scholar]
- Case report:Hepatotoxicity associated with the use of hydroxychloroquine in a patient with COVID-19. Am J Trop Med Hyg. 2020;102:1214-6.
- [Google Scholar]
- BCG vaccination protects against experimental viral infection in humans through the induction of cytokines associated with trained immunity. Cell Host Microbe. 2018;23:89-100s.e5.
- [Google Scholar]
- Mumps:An update on outbreaks, vaccine efficacy, and genomic diversity. Clin Microbiol Rev. 2020;33:e00151-19.
- [Google Scholar]
- Severe hyperphosphatasemia and severe acute respiratory syndrome Coronavirus 2 infection in children. Blood Coagul Fibrinolysis. 2020;31:575-7.
- [Google Scholar]







