Translate this page into:
Prescription practices of physicians, quality of care, and patients’ safety: A mixed methods comprehensive study
Address for correspondence: Babar Tasneem Shaikh, Health Services Academy, Islamabad, Pakistan. Phone: +92-51-9255590-5, Cell: +92-333-2303403. E-mail: shaikh.babar@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
ABSTRACT
Objectives:
Amidst inconsistent prescribing patterns and potentially harmful medication errors in the field of medical practice, this study endeavored to explore the prescription practices of physicians in Rawalpindi metropolitan city in Pakistan.
Methods:
A mixed method study was conducted based on the analysis of 1232 prescriptions gathered from 16 pharmacies, along with in-depth interviews with 13 practicing physicians. The prescriptions were assessed for legibility, polypharmacy, patient details, history, diagnosis, and other relevant information. Data were analyzed using descriptive statistics, and the prevalence of various aspects of prescription accuracy was calculated. Thematic analysis was conducted on the qualitative data.
Results:
Almost half of the prescriptions were from the private general practitioners, and the rest were from hospital-based doctors and consultants. Only a small percentage of prescriptions were fully legible, and many had incomplete or missing patient information, medical history, and diagnosis. Polypharmacy was also found to be prevalent, with significant differences in prescription accuracy across different medical specialties. The absence of continuing medical education, influence of pharmaceutical industry, and overcrowded practice settings drive the doctors to prescription practices. On the user side, perception of polypharmacy, patient–physician communication, and availability and cost of medicines emerged as major themes.
Conclusion:
There is an obvious need to improve prescription accuracy regarding patient safety on the whole. Increased investment in health-care infrastructure, greater access to continuing medical education, and a commitment to promote evidence-based medicine could make a difference. Prescription practices must be safe, effective, and aligned with the latest advances in medical science.
Keywords
Pakistan
physicians
polypharmacy
prescription practices
Introduction
Prescription practices of doctors play a crucial role in the health outcomes of patients. Writing prescriptions are an integral part of any medical interaction, based on the importance of information found in these documents. Errors during prescribing can have detrimental effects on the health of patients.[1] In Pakistan, the prescription practices of doctors have been the subject of much debate and discussion in recent years. Polypharmacy, the use of irrational drug combinations, and low adherence to standard treatment guidelines are common among the medical practitioners.[2] The availability of counterfeit and substandard drugs, coupled with inadequate regulation and oversight, has led to concerns about the quality of care being provided to patients.[3] The situation is further complicated by the lack of standardization in the country’s health-care system. Doctors in Pakistan are often faced with limited access to up-to-date information about the latest treatments and medications. This can lead to inconsistent prescribing patterns and potentially harmful medication errors. In addition, there is often a lack of cooperation between different health-care providers, leading to difficulties in coordinating patient care and ensuring that patients receive the best possible treatment.[4]
Despite these challenges, there are signs of progress in the prescription practices of doctors in Pakistan. In recent years, the government has taken steps to improve the regulation and oversight of the health-care system, and initiatives have been launched to promote the use of evidence-based medicine. In addition, growing number of doctors are taking advantage of new technologies, such as electronic medical records and telemedicine, to improve the quality of care they provide to patients.[5] Figure 1 explains the theoretical framework of our research study. Due to the rampant inconsistent prescribing patterns and potentially harmful medication errors in the field of medical practice, this study endeavored to explore the prescription practices of physicians in Rawalpindi metropolitan city in Pakistan. However, much work remains to be done to fully address the challenges facing the prescription practices of doctors in Pakistan. There is a need for increased investment in health-care infrastructure, greater access to training and education for health-care providers, and a commitment to evidence-based medicine. By working together, health-care providers, policymakers, and patients can help to ensure that prescription practices in Pakistan are safe, effective, and aligned with the latest advances in medical science.[6]
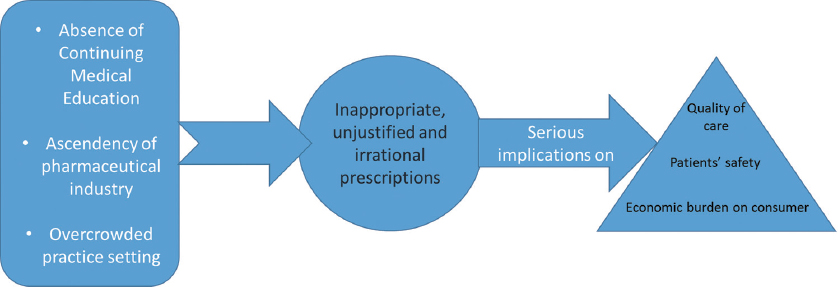
- Theoretical framework of this research
Materials and Methods
We conducted a mixed method study, in Rawalpindi City, Pakistan. A total of 1232 prescriptions from patients visiting 16 different pharmacies in Rawalpindi city were included in the study. The prescriptions were gathered for 3 months, from August to November 2022. The prescriptions were photographed at the point of dispensing at the pharmacies. The photographs were then assessed for various aspects of prescription accuracy, including legibility, polypharmacy, patient details, history, diagnosis, and other relevant information. The consultations included general medicine, pediatrics, ENT, gynecology and obstetrics, psychiatry, and dermatology. The data collected from the photographs of the prescriptions were analyzed using descriptive statistics. The prevalence of various aspects of prescription accuracy was calculated, and the results were compared across different medical specialties.
To understand the phenomenon better and answer the research questions, we included a qualitative component and employed the grounded theory by developing an interview guide for conducting in-depth interviews with practicing physicians from Rawalpindi. The questions probed their prescription practices and the influences of various factors on these practices. We interviewed 13 physicians with at least 5 years’ experience, till we reached the point of saturation. The interviews were audio-recorded, transcribed verbatim and analyzed using thematic analysis. Each interview took around 45 min and was conducted in the personal offices/practice chambers of the doctors, ensuring their privacy. Out of the 13 respondents, 4 were professors (Internal Medicine, Pediatrics, Psychiatry, and ENT), 3 were working as assistant professors (Internal Medicine, Gynecology and Obstetrics, and Pediatrics) and the remaining 6 were general practitioners/family physicians. Thematic analysis was conducted by coding and iterative interpretation was employed to identify recurring themes and patterns related to prescription practices. Data from both qualitative and quantitative phases of the study were triangulated. The study was approved by the institutional review board of Islamabad Medical and Dental College. The confidentiality of the prescribing physicians and the relevant medical information was protected in accordance with ethical principles.
Results
The largest number of prescriptions included in the study was from the private general practitioners, accounting for 49.3% of the total, followed by the specialist/consultant at 46.1%, medicine and allied at 24.4%, gynecology and obstetrics at 9.7%, and other specialties at much smaller percentages.
The results of the study, although not surprising, obviously show that there were several aspects of prescription writing that needed improvement. Out of the 1232 prescriptions included in the study, a significant percentage (27.1%) of prescriptions was not fully legible, and many had incomplete or missing patient information, medical history, and diagnosis. Polypharmacy was also found to be prevalent (34.1%), with a large proportion of patients receiving multiple medications simultaneously. There were significant differences in prescription accuracy across different medical specialties, with some specialties showing higher rates of errors than others.
As shown in Table 1, in terms of the qualifications of the doctors prescribing the medications, 41.1% of prescriptions were from MBBS doctors, whereas 46.1% were from specialist/consultant doctors and 12.7% from post-graduate trainees. With regards to the type of health-care facility where the prescriptions were issued, the majority (51.3%) were from public sector tertiary care facilities, followed by private hospital at 31.5%, private clinic at 14.9%, and public sector (primary/secondary care) at only 2.3%.
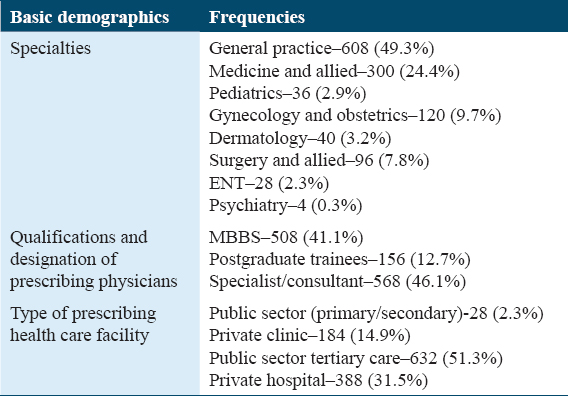
These results provide important information about the distribution of prescription medications across different medical specialties, health-care providers, and types of health-care facilities in Rawalpindi City.
Table 2 provides information on the frequency and percentage of various variables mentioned in 1232 prescription records. Most prescriptions included the patient’s name (99.4%) and age (94.2%), which suggests that these pieces of information are routinely collected and documented by health-care providers. However, only 5.8% of prescriptions included the patient’s weight, which may be an area for improvement in documentation practices.
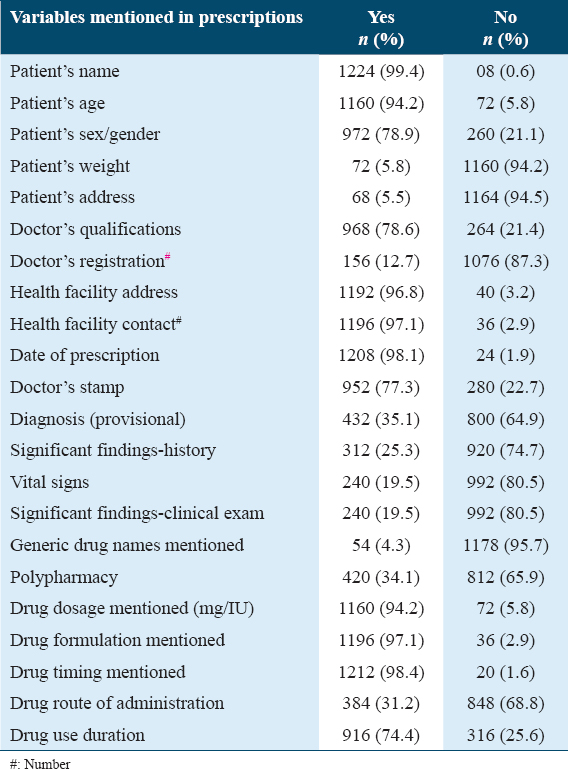
The differences in the proportion of prescriptions that included the patient’s sex/gender (78.9% yes vs. 21.1% No) and the doctor’s qualifications (78.6% yes vs. 21.4% no) were statistically significant (P < 0.05). These findings indicate that there may be variability in the information provided in prescriptions depending on the health-care provider and the health-care facility. The doctor’s registration number was mentioned in only 12.7% of prescriptions, which suggests that there may be room for improvement in the documentation practices of health-care providers. Most prescriptions included the health-care facility’s address (96.8%) and contact information (97.1%), which suggests that this information is routinely collected and documented by health-care providers. However, the doctor’s stamp was only mentioned in 77.3% of prescriptions, which may be an area for improvement in documentation practices. Notably, the generic drug names were mentioned in only 4.3% of prescriptions, which suggests that there is a lack of emphasis on the use of generic drugs in the health-care system. When patients do not have access to the generic drug names, they are forced to purchase drugs sold by specific companies, instead of having the choice to purchase medications according to their spending capacity. In contrast, drug dosage was mentioned in many prescriptions (94.2%), which indicate that health-care providers place a high emphasis on ensuring that patients receive the correct dosage of medication.
Overall, the results suggest that there is variability in the information provided in prescriptions, which could have implications for patient safety and the quality of care delivered. The findings highlight several areas for improvement in documentation practices and may inform interventions to improve the standardization and completeness of prescription records.
As regards the qualitative results, the absence of continuing medical education, influence of pharmaceutical industry, and overcrowded practice settings drive the doctors to prescription practices. On the user side, perception of polypharmacy, patient–physician communication, and availability and cost of medicines emerged as major themes.
Theme 1: Influence of Pharmaceutical Industry: Participants highlighted the pervasive influence of pharmaceutical representatives and acknowledged the impact of marketing strategies employed by the industry. “The pharmaceutical representatives visit our clinics regularly and offer various incentives to promote their products. It is hard to resist their influence when they bring gifts and offer sponsorship for medical conferences.” [P-1] “I’ve noticed that some pharmaceutical companies organize educational events where they present biased information to influence our prescribing preferences. It is challenging to separate the scientific knowledge from their marketing tactics.” [P-2]; Theme 2: Training and Continuing Medical Education: Physicians expressed concerns about the lack of updated knowledge and limited exposure to evidence-based medicine due to inadequate training programs. “Our medical education focuses more on theoretical knowledge rather than practical skills. As a result, we often rely on outdated prescribing practices and may not be aware of the latest research and guidelines.” [P-2] “Continuous medical education is crucial for keeping up with advancements in healthcare. However, the opportunities for attending relevant training programs are limited, and it becomes difficult to incorporate evidence-based practices into our prescriptions.” [P-3]; Theme 3: Challenges in Overcrowded Clinical Settings: Physicians identified time constraints, high patient load, and limited patient education as significant challenges in overcrowded outpatient department settings. “In our outpatient department (OPD), we have a large number of patients to attend to within a limited time frame. This often leads to hurried consultations and prescribing decisions without sufficient evaluation of the patient’s condition.” [P-5] “Due to the overwhelming patient load, it becomes challenging to spend enough time with each patient to educate them about their prescribed medications. Many patients leave without a clear understanding of how to take their medications properly.” [P-1]; Theme 4: Perception of Polypharmacy: Participants acknowledged patient expectations and the fear of legal repercussions as factors contributing to excessive polypharmacy. “Patients often come to us with the belief that more medications mean better treatment. They expect multiple prescriptions even for minor ailments, and meeting these expectations becomes a challenge.” [P-2] “As physicians, we also worry about legal consequences if we do not prescribe what patients demand. To avoid any potential complaints or legal issues, we sometimes tend to prescribe more medications than necessary.”[P-6]; Theme 5: Communication and Patient–Physician Relationship: Participants highlighted the importance of effective communication and the impact of the patient–physician relationship on prescription practices. “Establishing a good rapport with patients is essential. When patients trust and feel comfortable with their physician, they are more likely to follow prescribed treatments and medications.” [P-9] “Clear communication is crucial in ensuring patients understand the purpose, dosage, and potential side effects of prescribed medications. Sometimes, language barriers or cultural differences can hinder effective communication.” [P-7]; Theme 6: Availability and Cost of Medications: Physicians expressed concerns about the availability and cost of medications and their impact on prescription decisions. “Limited availability of certain medications can influence our prescribing choices. We have to consider what is readily accessible and affordable for our patients.” [P-13] “The cost of medications can be a significant burden for patients, especially those with limited financial resources. Sometimes, we have to take into account the affordability factor when prescribing medications.” [P-12]. These qualitative findings provide insights into the underlying factors contributing to poor prescription practices among physicians in Rawalpindi, Pakistan. The influence of the pharmaceutical industry, inadequate training and education, challenges in overcrowded OPD settings, and the perception of polypharmacy all play significant roles in shaping prescription behaviors.
Discussion
Prescription accuracy and patient safety are critical aspects of high-quality healthcare. The precise documentation of patient information, medical history, diagnosis, and treatment plans in medical prescriptions is essential to ensure effective and safe healthcare delivery. However, studies conducted in Pakistan[7,8] and other developing countries[9,10] have reported poor prescription accuracy and incomplete patient information in medical prescriptions, leading to adverse drug reactions, medication errors, and other health complications. In contrast, developed countries such as the United States, Canada, and Australia have reported higher prescription accuracy rates and more complete patient information in medical prescriptions. For instance, a study conducted in the United States found that over 95% of prescriptions contained complete patient information, while a study in Canada reported a 99% accuracy rate for medication orders. Similarly, a study in Australia found that only 0.1% of prescriptions had errors related to the wrong drug or dosage.[11,12] The differences in prescription accuracy between developed and developing countries may be attributed to several factors. Developed countries typically have more stringent regulatory environments, with drug regulatory agencies closely monitoring and enforcing prescribing guidelines. In contrast, developing countries such as Pakistan may have less strict regulatory environments, which can lead to inappropriate prescribing practices.[13]
Health-care providers in developed countries have access to up-to-date medical information, including prescribing guidelines, clinical trials, and new drug approvals, which may result in more accurate and effective prescribing practices.[14] In contrast, health-care providers in developing countries may have limited access to such information, leading to outdated and inappropriate prescribing practices.[15] Moreover, developed countries typically have more robust healthcare resources, including healthcare facilities, healthcare providers, and financial resources. This can lead to more individualized care and better communication between patients and healthcare providers, resulting in more accurate and effective prescribing practices.[16] In contrast, developing countries such as Pakistan may have limited health-care resources, resulting in overcrowding in healthcare facilities and limited time for healthcare providers to spend with patients, leading to rushed and inappropriate prescribing practices. This was further highlighted in the qualitative section where the respondents emphasized the fact that the chances of incomplete prescriptions increase in case of extra workload, and often patients are not completely satisfied with the consultation owing to the limitedness of the consultations.[17]
In addition, cultural and social factors may also play a role in prescribing practices. For example, patients in Pakistan may prefer to receive multiple medications, and healthcare providers may prescribe multiple drugs to meet patient expectations. In contrast, patients in developed countries may be more likely to question healthcare providers about their prescriptions, resulting in more individualized and accurate prescribing practices.[18] Finally, the influence of the pharmaceutical industry on prescribing practices is an important factor. In Pakistan, the pharmaceutical industry is a major player in the healthcare sector and may influence prescribing practices through marketing and promotional activities.[19] We have discussed this issue in the qualitative section, where the influence of the pharmaceutical industry incentivizes drug prescriptions added on by the lack of generic prescriptions. This forces people to buy products from specific country, instead of freely choosing the generic drug according to their financial capacities.
Prescription accuracy and patient safety are critical components of high-quality healthcare. The differences in prescription accuracy between developed and developing countries may be attributed to several factors, including the regulatory environment, access to up-to-date medical information, health-care resources, cultural and social factors, and the influence of the pharmaceutical industry. A country like Pakistan must develop mechanisms of regular audits of prescription practices both for public and private health sectors.[20] While our study aimed to shed light on the prevailing practices, we also acknowledged the potential for improvement and identified areas and opportunities to improve the situation. Our ultimate goal is to contribute to an informed and constructive public discussion on healthcare in the country, ensuring that patients receive optimal and high-quality care. This study provides valuable insights into the prescription practices of doctors in Rawalpindi City, Pakistan. The large sample size and the inclusion of prescriptions from multiple medical specialties enhance the generalizability of the results. In addition, the use of photographs of the prescriptions allows for objective and accurate assessment of various aspects of prescription accuracy. The study is limited by its cross-sectional design, which only provides a snapshot of prescription practices at a single point in time. The study may also be subject to bias, as the prescriptions were obtained from only 16 pharmacies, and may not be representative of all prescriptions dispensed in Rawalpindi city.
Conclusion
Our study has documented a fresh the prescription practices of physicians and their implications on the patients. Prescription writing is an integral part of medical services, as it is directly related to quality and safety of health services. Prescription accuracy and patient safety need improvement in Pakistan. The access to up-to-date medical information for the practicing physicians must be made readily available, and part of their medical practice license renewal. Stringent measures need to be taken to curb the unnecessary and unmerited influence of the pharmaceutical sector. Last but not least, patient’s education also needs to be looked into for raising awareness on irrational prescriptions. Addressing these issues requires a wide-ranging health system’s approach. Improving prescription accuracy and rationality is crucial for patient safety and quality of care, especially with the increasing use of polypharmacy. A holistic approach that keeps in mind the resource constraints and sustainability is imperative and should be implemented by strengthening the regulatory bodies and training requirements of physicians.
Authors Declaration Statements
Ethics approval and consent to participate
This study was approved by the ethics committee of, Islamabad Medical and Dental College, Islamabad, Pakistan (Reference No 681IMDC/IRB-2022) and written informed consent was taken from all participants involved in this study.
Availability of data and materials
The data sets used in this study are available with the corresponding author and will be provided on a reasonable request.
Competing interest
The authors have no conflict of interest to declare.
Funding statement
This work was not funded by any institution.
Authors’ Contributions
MAA, ASA, BTS, MBK, AS, and ZN were responsible for composing the manuscript; MAA, and ZN were responsible for conceiving the experimental study design, performing the experiment, and statistical analysis; ASA, BTS, MBK and AS analyzed the data and edited the manuscript. All authors involved in reviewing the manuscript. All authors have read and agreed to the published version of the manuscript.
References
- Overuse of medications in low-and middle-income countries:A scoping review. Bull World Health Organ. 2023;101:36-61.
- [Google Scholar]
- Prescribing practices and associated factors among medical practitioners in Lahore, Pakistan:A cross-sectional study. J Pharm Policy Pract. 2022;15:55.
- [Google Scholar]
- Prevalence and risk factors of substandard and counterfeit medicines in Pakistan:A cross-sectional study. BMJ Open. 2017;7:e017937.
- [Google Scholar]
- Prescribing practices and prescription errors in outpatient settings in Lahore, Pakistan:A cross-sectional study. BMC Health Serv Res. 2018;18:797.
- [Google Scholar]
- Adoption and impact of electronic medical records on prescription practices of general practitioners in Lahore, Pakistan. Health Inform J. 2020;26:165-72.
- [Google Scholar]
- Knowledge, attitudes, and practices regarding rational use of medicines:A cross-sectional survey among medical and non-medical university students in Karachi, Pakistan. Front Public Health. 2021;9:643730.
- [Google Scholar]
- The overprescribing of opioids:A public health approach to an epidemic of addiction. J Pak Med Assoc. 2023;73:1358.
- [Google Scholar]
- Medication errors and type 2 diabetes management:A qualitative exploration of physicians'perceptions, experiences and expectations from Quetta city, Pakistan. Front Med (Lausanne). 2022;9:846530.
- [Google Scholar]
- Good versus poor prescribers:The comparison of prescribing competencies in primary care. Prim Health Care Res Dev. 2022;23:e22.
- [Google Scholar]
- The knowledge, attitude and practice of health practitioners towards antibiotic prescribing and resistance in developing countries-a systematic review. J Clin Pharm Ther. 2018;43:606-13.
- [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS, eds. To Err is Human:Building a Safer Health System. Washington, DC: National Academies Press (US); 2000.
- Prescription writing practices in a tertiary care hospital in Pakistan. Trop J Pharm Res. 2015;14:1281-6.
- [Google Scholar]
- Prescribing Errors in General Practice:A Review of the Literature. Sydney, Australia: National Prescribing Service; 2002.
- Analysis of the degree of implementation of medication error prevention practices in Spanish hospitals (2022) Farm Hosp. 2023;47:T268-76.
- [Google Scholar]
- Prevalence, incidence and nature of prescribing errors in hospital inpatients:A systematic review. Drug Saf. 2009;32:379-89.
- [Google Scholar]
- Medication Without Harm-Global Patient Safety Challenge on Medication Safety. Geneva: World Health Organization; 2017.
- Prescribing rationality in Khartoum state, Sudan:An update. Sudan Med J. 2014;9:61-5.
- [Google Scholar]
- Evaluation of drug administration errors in a teaching hospital. BMC Health Serv Res. 2012;12:60.
- [Google Scholar]
- The extent and reasons of drug prescriptions without diagnosis in Pakistan:A scoping review. BMC Health Serv Res. 2020;20:1077.
- [Google Scholar]
- A prescription audit using the World Health Organization-recommended core drug use indicators in a rural hospital of Delhi. J Educ Health Promot. 2019;8:37.
- [Google Scholar]







