Translate this page into:
Prevalence of co-infection of human immunodeficiency virus in diagnosed tuberculosis cases: Meta-analysis
Address for correspondence: Naif H. Alanazi, College of Health Science, Saudi Electronic University, Riyadh, Saudi Arabia. E-mail: n.alanazi@seu.edu.sa
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
ABSTRACT
Objective:
The objective of the study was to find pooled prevalence and risk factors of co-infection of human immunodeficiency virus (HIV) in diagnosed tuberculosis (TB) cases.
Methods:
Search engines including PubMed and Google Scholar were used to find literature using search terms such as “co-infection,” “HIV,” “Acquired Immunodeficiency Syndrome,” TB and “Prevalence” among others. All original studies conducted on the prevalence of HIV co-infection among diagnosed TB patients that were freely available in full length had a clear methodology and relevant results were included in the study.
Result:
From 1021 initial studies, a total of 18 studies were selected for analysis. A total of 18 studies were included with a total sample size of 44943. The minimum prevalence of HIV-TB was reported in a study from Pakistan as 0.29% and the maximum prevalence of HIV-TB was found in Nigeria, that is, 44.20%. The pooled prevalence of HIV/TB co-infection was 16.291% (95%; 9.57–24.38) using the random effect method. As per Begg’s test, there was no publication bias. As I2 is 99.74% so, there is high heterogeneity among studies; hence, random effect model is preferred.
Conclusion:
The study concludes that the pooled prevalence of HIV/TB co-infection was found to be 16.291% (95%; 9.57–24.38). The risk of mortality will be substantially raised by the co-existence of HIV-TB co-infection, so early screening and emphasizing the urgent need for integrated health-care interventions can cope with the situation.
Keywords
Co-infection
HIV
meta-analysis
pooled prevalence
systematic review
tuberculosis
Introduction
Tuberculosis (TB), often caused by Mycobacterium tuberculosis (MTB) in humans, is a widespread global health issue with a high risk of mortality.[1,2] Specifically preferring to localize in macrophages, MTB is an acid-fast facultative intracellular rod-shaped obligate aerobe.[3] People with the illness cough, sneeze, or spit, which causes the aerosol to be released into the air.[4] Because MTB is an aerobic intracellular binding bacteria and favors tissues that are constantly in touch with high oxygen levels, such as the lung, TB is a very frequent chronic infection condition.[5] Depending on the immunological condition, the person may acquire the disease after breathing the bacillus, which spreads by minute droplets of saliva. MTB may spread to any area of the body after it has settled in the lungs.[5,6] One-third of the 33.2 million people living with HIV are thought to simultaneously have MTB.[7,8]
TB and HIV share an immune-compromising impact mechanism that increases mortality in HIV-infected individuals, so TB control continues to be a worldwide concern.[9,10] Almost one in ten people diagnosed with TB also have HIV. Similarly, nearly one-third of HIV-positive patients also have TB infections. Majority of them belong to developing countries with low socioeconomic features. HIV causes active TB to develop by encouraging the progression of MBT infections from latent as well as newly acquired TB infections to active TB.[11] TB has been identified as a leading cause of mortality among people with HIV, and literature also reports that HIV infection is a significant predictor of TB infection and illness.[12] Considering the fact that active TB itself is assumed an HIV-defining disease and a clinical criteria to start ART therapy, the simultaneous diagnosis of both conditions is highly recommended to identify patients with co-infection.[13]
Data on prevalence and risk factors of co-infection of the human immunodeficiency virus (HIV) in TB cases are not widely available. The prevalence of HIV in TB cases ranges from 0.34%[14] to 32.8%.[15] Alarmingly, the incidence of TB is rising in many countries making it the largest infectious cause of mortality globally. The prevalence of MTB is increasing with time and HIV is considered one of its primary determinants. The co-infection of HIV and TB has more serious and life-threatening outcomes compared to the presence of any of these diseases alone.[16]
A number of studies have been conducted on the prevalence of TB and HIV separately, but a limited amount of data is available on HIV and TB co-infection and contains some disparities in reported results. Hence, this meta-analysis aims to review the available literature on HIV-TB co-infection and comprehensively presents pooled results about its prevalence.
Methods
Reporting method
A comprehensive research on the prevalence of HIV-TB co-infection that was openly accessible online was retrieved. Preferred Reporting Items for Systematic Review and Meta-Analysis Statement (PRISMA) guidelines were used to assist in reporting the findings of this research.
Study design
Meta-analysis.
Search strategy and selection criteria
The terms “co-infection, (HIV or acquired immunodeficiency syndrome [AIDS])” and (TB) were searched in PubMed and Google Scholar to find English publications on investigations of the prevalence of HIV/TB co-infection.
Inclusion and exclusion criteria
Inclusion criteria included any published research addressing the prevalence of HIV infection among diagnosed TB patients. Regardless of the diagnostic approach, investigations were included, although the majority were based on HIV blood testing and chest radiography for TB. Studies with concurrent TB infection in the HIV/AIDS group were disqualified. Moreover, review papers, articles with incomplete content or any payment or permission issues, and ones in any language other than English were also excluded from the study.
Flow chart of studies
We followed the PRISMA flow chart. The details are given in Figure 1.
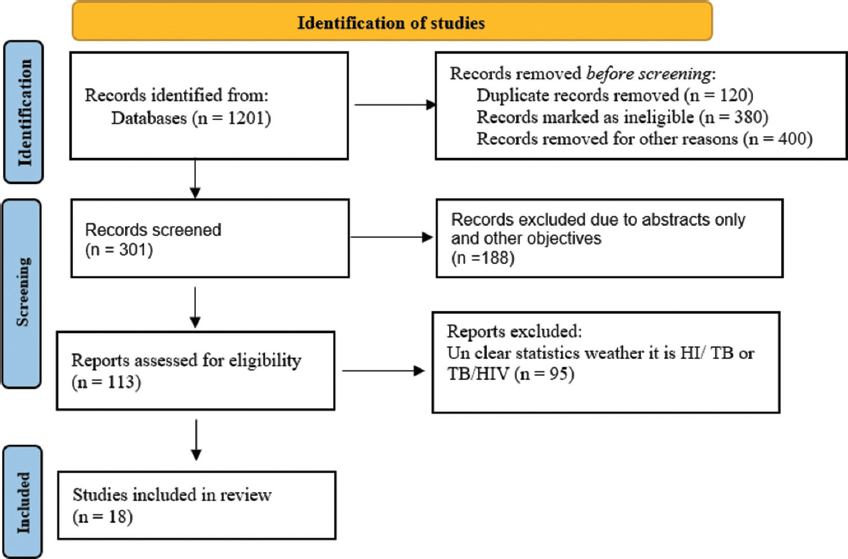
- PRISMA criteria for literature search and studies selection for meta-analysis
Data extraction technique
For the purpose of obtaining data from shortlisted studies, a data extraction form was created. The form included the first author, the year, the study design, the sample size, the prevalence, and risk factors. The information was gathered individually from the papers by two authors. A thorough discussion was done to get the papers double-checked and a solution for fixing any mismatch in the reported data was reached by both the authors together. The controversy or ambiguity in retrieved data was solved with discussion and the developing consensus.
Statistical analysis
A table for meta-analysis was created in Microsoft Word with the headers of the study, sample size, and prevalence. Using the med Calc program, the pooled prevalence (95% CI) was determined. We calculated the proportion of variance across trials that is attributable to heterogeneity rather than chance using Cochran’s Q (given as 2 and p values) and the I2 statistic.[17,18] I2> 75% considered high heterogeneity,[19] we applied random-effects models due to the high values of I2.[17,18]
Results
A total of 18 studies were included with a total sample size of 44943. The minimum sample size was 192[20] and the maximum sample size was taken as 18461.[14]
Prevalence of HIV in diagnosed TB patients
The minimum prevalence of HIV-TB was reported in a study from Pakistan as 0.29%[14] (95% CI = 0.22–0.38) and the maximum prevalence of HIV-TB was found in Nigeria, that is, 44.20%[21] (95% CI = 38.19–50.66) Table 1. The details for the prevalence of HIV-TB co-infection are given in Forest plot [Figure 2] and the details of consideration of publication bias are given in Figure 3.
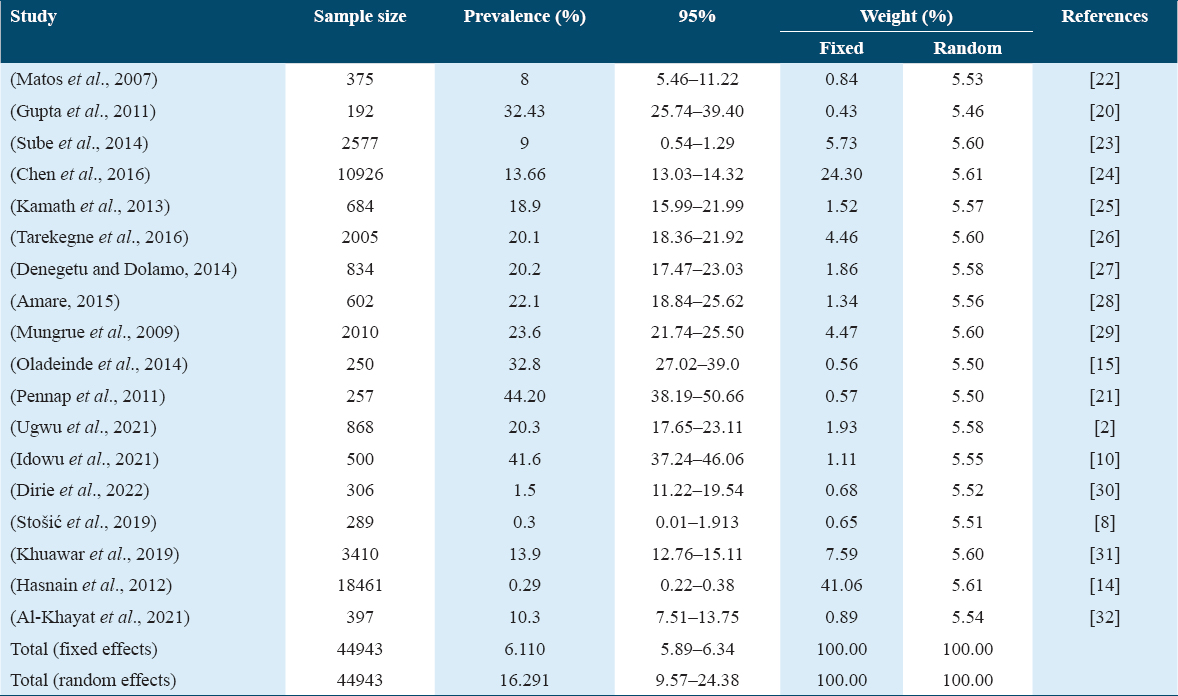
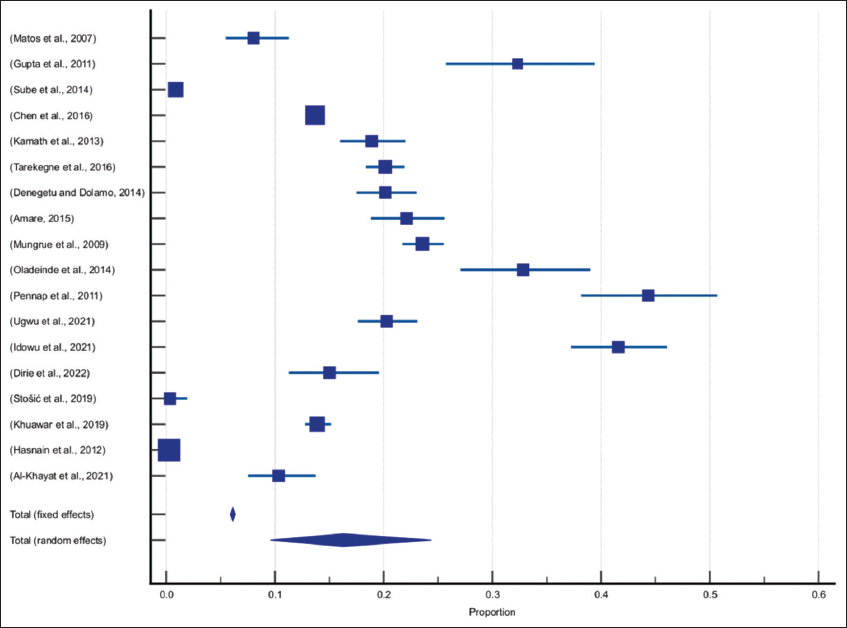
- Forest plot for the prevalence of HIV-TB co-infection
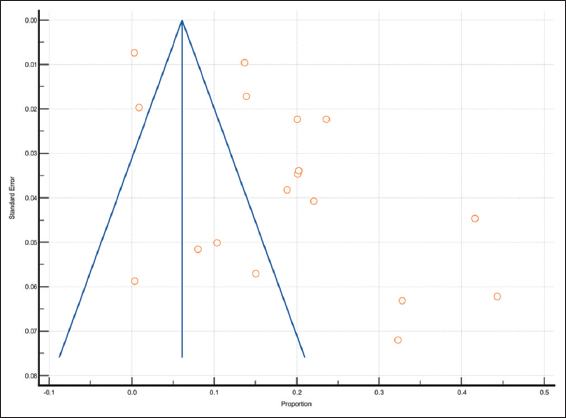
- Publication bias using Funnel plot
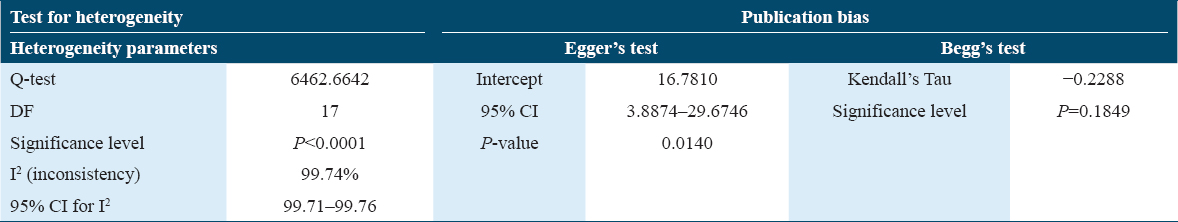
According to Egger’s test, there was publication bias in these studies while Begg’s test suggests that there was no publication bias. As Begg’s test is preferred over Egger’s test, hence we will consider that in these studies there was no publication bias. There is high heterogeneity among the studies, (Q-test = 6462.6642, P < 0.0001 and I2 = 99.74%, 95% CI for I2 99.71–99.76). Due to high heterogeneity among studies, random affect methods were used for pooled prevalence. Hence, the pooled prevalence of HIV/TB was 16.291% (95%; 9.57–24.38) using the random effect method Table 2.
Discussion
The co-infection of HIV and TB has been labeled as “the cursed duet” due to the high mortality and morbidity associated with these, especially when MTB is involved.[21] HIV and MTB co-infection have been reported as one of the major determinants of global mortality among all infectious causes.[21] The annual mortality rate due to HIV is 1 million and from TB is 1.3 million.[13] HIV almost diminishes the immunity making it easier for TB to spread way faster and cause organ failures or extreme damage, costing lives. Therefore, mortality in TB-diagnosed patients with HIV-positive status has higher mortality rates compared to HIV-negative patients. It is therefore important to diagnose both diseases together to identify cases with co-infection and work rigorously for their treatment.[33] Although several studies have published the prevalence of HIV and TB separately, there is limited data available on HIV-TB co-infection, their risk factors, and potential health outcomes. Therefore, this study aimed to review and conduct a meta-analysis on the prevalence of HIV-TB co-infection.
Various studies are done with different prevalences of HIV-TB confection, as a Pakistani study reported that the prevalence of HIV among pulmonary TB patients was 0.29% and among extrapulmonary TB patients was 0.48% (P = 0.09).[14]
In 2015 a study done in China, by Li et al. reported the prevalence of HIV in TB cases as 128 (4.8%) tested positive.[34] An Indian study reported the prevalence of HIV-TB as 8.9%.[20] Another Indian, study was done to evaluate the prevalence of HIV infection in patients with TB, so they reported out of 75, 9 (12%) patients were found to be HIV positive. The male-female ratio among HIV-positive cases was 2:1.[35] A Malaysian study was designed to describe the clinical manifestation of TB infection cases in Malaysia and to determine the individual risk factors for their occurrence. They reported that the provenance of HIV in TB patients was 12.5%.[36]
In 2015, Belay et al. from Ethiopia found that 105 (32.3%) of the 325 lung TB suspects had positive cultures and 44 (13.5%) had positive smear results. Five of the smear-positive patients had negative cultures, for a total of 110 (33.8%) suspected pulmonary TB patients with bacteriological confirmation. About 82 (28.5%) of 287 pulmonary TB suspects who underwent HIV testing were HIV positive.[37] Another research from Ethiopia looked at 602 instances of TB patients receiving treatment and found that 133 (22.1%) of them also had HIV, whereas 469 (77.9%) had TB as their sole diagnosis. They also came to the conclusion that there was a rising incidence of TB-HIV co-infection from 23.9% to 35% from 2009 to 2011 and a declining rate from 35% to 12% from 2011 to 2013.[28]
Oladeinde et al. from Nigeria found one of the highest prevalences of HIV among TB patients, that is, 32.8%.[15] In China, where the overall prevalence of HIV infection was 0.9% (0.6–1.4%) in 29 studies, it was determined that this group might be a feasible target for HIV screening.[38]
The current study found that the minimum prevalence of HIV-TB was reported in a study from Pakistan as 0.29% and the maximum prevalence of HIV-TB was found in Nigeria, that is, 44.20%. The pooled prevalence of HIV/TB co-infection was 16.291% (95%; 9.57–24.38) using the random effect method. This difference might be because people who live in urban areas differ from those who live in rural ones, and people in urban areas are more susceptible to dual infections. Moreover, high-risk groups may from commercial sex workers, military personnel, long-distance drivers, law enforcement officers, and others.[39] These groups are also unfairly distributed across the nation’s regions due to the inappropriate topography of the nation, which makes it difficult for them to access the few available health services, and they are also poorly monitored and evaluated.[39]
Conclusion
The study concludes that the pooled prevalence of HIV/TB was found to be 16.291% (95%; 9.57–24.38). A higher prevalence of HIV-TB co-infection may increase infectious-related mortality and hence, early screening and integrated health-care interventions should be considered on an urgent basis to cope with this situation.
Recommendations
HIV in diagnosed TB patients is fairly common and increases the risk of mortality among these patients. It is, therefore, imperative to timely rule out the possibility of any co-infection and manage such patients with extra cautiousness to minimize worse health outcomes. Hence, appropriate two-way preventive and control strategies should be developed for various TB patients. For instance, better information should be shared about TB and HIV infection, and blood transfusion monitoring has to be reinforced. Furthermore, to lower the rate of co-infection, individuals should be encouraged to follow safe sexual practices and have a better awareness of HIV prevention.
References
- Pulmonary tuberculosis due to Mycobacterium microti:A study of six recent cases in France. J Med Microbiol. 2010;59:984-9.
- [Google Scholar]
- Prevalence of tuberculosis, drug-resistant tuberculosis and HIV/tb co-infection in Enugu, Nigeria. Afr J Infect Dis. 2021;15:24-30.
- [Google Scholar]
- Mycobacteria. In:Review of Medical Microbiology and Immunology 2010:150-4.
- Mycobacterial outer membranes:In search of proteins. Trends Microbiol. 2010;18:109-16.
- [Google Scholar]
- Studying some hematological changes in patients with pulmonary tuberculosis in Babylon governorate. Med J Babylon. 2011;8:608-17.
- [Google Scholar]
- Reactive thrombocytosis and erythrocyte sedimentation rate in patients with pulmonary tuberculosis. J Med Lab Diagn. 2014;5:29-34.
- [Google Scholar]
- HIV infection-associated tuberculosis:The epidemiology and the response. Clin Infect Dis. 2010;50(Suppl 3):S201-7.
- [Google Scholar]
- HIV prevalence, knowledge and self-perceived risk of HIV infection among tuberculosis patients in Serbia. Cent Eur J Public Health. 2019;27:99-105.
- [Google Scholar]
- BHIVA Guidelines Subcommittee. British HIV association and British infection association guidelines for the treatment of opportunistic infection in HIV-seropositive individuals 2011. HIV Med. 2011;12(Suppl. 2):1-140.
- [Google Scholar]
- Prevalence and the risk factors associated with HIV-TB co-infection among clinic attendees in dots and art centres in Ibadan, Nigeria. Cent Asian J Med Nat Sci. 2021;2:73-87.
- [Google Scholar]
- TB/HIV co-infections and associated factors among patients on directly observed treatment short course in Northeastern Ethiopia:A 4 years retrospective study. BMC Res Notes. 2015;8:666.
- [Google Scholar]
- The prevalence of HIV among adults with pulmonary TB at a population level in Zambia. BMC Infect Dis. 2017;17:236.
- [Google Scholar]
- HIV screening among newly diagnosed TB patients:a cross sectional study in Lima, Peru. BMC Infect Dis. 2018;18:136.
- [Google Scholar]
- Screening for HIV among tuberculosis patients:A cross-sectional study in Sindh, Pakistan. BMJ Open. 2012;2:e001677.
- [Google Scholar]
- Prevalence of HIV infection among patients with pulmonary tuberculosis in a rural tertiary hospital in Nigeria. Niger J Exp Clin Biosci. 2014;2:90-4.
- [Google Scholar]
- Prevalence of tuberculosis and its impact on mortality among HIV infected patients in Chile. Rev Méd Chile. 2008;136:578-86.
- [Google Scholar]
- Prevalence of TB/HIV co-infection in countries except China:A systematic review and meta-analysis. PLoS One. 2013;8:e64915.
- [Google Scholar]
- Prevalence of preterm birth in Pakistan:A systematic review and meta-analysis. Ann King Edw Med Uni. 2017;23:229-35.
- [Google Scholar]
- A systematic review and meta-analysis on the efficacy of physiotherapy intervention in management of lumbar prolapsed intervertebral disc. Int J Health Sci (Qassim). 2021;15:49-57.
- [Google Scholar]
- Diabetes mellitus and HIV as co-morbidities in tuberculosis patients of rural south India. J Infect Public Health. 2011;4:140-4.
- [Google Scholar]
- Prevalence of HIV/AIDS among tuberculosis patients seen in a rural clinic in Nigeria. Trakia J Sci. 2011;9:40-4.
- [Google Scholar]
- Prevalence of HIV infection in patients hospitalized for tuberculosis in Bahia, Brazil. Braz J Infect Dis. 2007;11:208-11.
- [Google Scholar]
- HIV and TB co-infection in South Sudan:A three year retrospective study. S Sudan Med J. 2014;7:86-90.
- [Google Scholar]
- Prevalence and determinants of HIV in tuberculosis patients in Wuxi City, Jiangsu province, China:A cross-sectional study. Int J STD AIDS. 2016;27:1204-12.
- [Google Scholar]
- HIV-TB coinfection:Clinico-epidemiological determinants at an antiretroviral therapy center in Southern India. Lung India. 2013;30:302-6.
- [Google Scholar]
- Prevalence of human immunodeficiency virus infection in a cohort of tuberculosis patients at Metema Hospital, Northwest Ethiopia:A 3 years retrospective study. BMC Res Notes. 2016;9:192.
- [Google Scholar]
- HIV screening among TB patients and co-trimoxazole preventive therapy for TB/HIV patients in Addis Ababa:Facility based descriptive study. PLoS One. 2014;9:e86614.
- [Google Scholar]
- Tuberculosis and HIV Co-infection among patients on tuberculosis treatment at Fenote Selam district hospital, Amhara regional state, Northwest Ethiopia. Global J Med Res. 2015;15:8-13.
- [Google Scholar]
- Trends in HIV/TB coinfection in Trinidad and Tobago for the period 1998-2007. J Int Assoc Physicians AIDS Care (Chic). 2009;8:170-5.
- [Google Scholar]
- The prevalence of HIV among tuberculosis patients in Benadir, Somalia. Retrospective multi-center study. Ann Med Surg (Lond). 2022;78:103793.
- [Google Scholar]
- Prevalence of HIV infection among tuberculosis patients in Sindh, Pakistan. Nat Ed Advis Board. 2019;30:109.
- [Google Scholar]
- Prevalence of HIV among newly diagnosed tuberculosis patients in Erbil Governorate, Iraq. J Contemp Med Sci. 2021;7:102-7.
- [Google Scholar]
- Tuberculosis testing among populations with high HIV risk in Tijuana, Baja California, Mexico. Rev Panam Salud Publica. 2012;32:30-5.
- [Google Scholar]
- Epidemiology of HIV-associated tuberculosis in Urumqi, China. Transplant Proc. 2015;47:2456-9.
- [Google Scholar]
- Prevalence of HIV in clinically suspected cases of pulmonary tuberculosis. Nat J Lab Med. 2014;3:22-6.
- [Google Scholar]
- Clinical manifestation and risk factors of tuberculosis infection in Malaysia:Case study of a community clinic. Glob J Health Sci. 2015;7:110-20.
- [Google Scholar]
- Prevalence of tuberculosis, HIV, and TB-HIV co-infection among pulmonary tuberculosis suspects in a predominantly pastoralist area, northeast Ethiopia. Glob Health Action. 2015;8:27949.
- [Google Scholar]
- The twin epidemics:Prevalence of TB/HIV co-infection and its associated factors in Ethiopia;A systematic review and meta-analysis. PLoS One. 2018;13:e0203986.
- [Google Scholar]







