Translate this page into:
Risk factors for the systemic inflammatory response syndrome and sepsis following surgical management of acute intestinal obstruction
Address for correspondence: Rema Saad Almohanna, National Guard Health Affairs, King Saud bin Abdulaziz University for Health Sciences, King Abdulaziz Medical City, Riyadh 11426 – 22490, Riyadh 11481- 3660, Saudi Arabia. E-mail: almohanna186@ksau-hs.edu.sa
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
Infection is one of the major complications following intestinal obstruction surgery, yet predictors of its occurrence are not sufficiently reported. In this study, we examine the factors leading to postoperative inflammatory response syndrome (SIRS) and sepsis.
Methods:
The data of 213 patients who underwent intestinal obstruction surgery between 2015 to 2020 in King Abdulaziz Medical City, Riyadh, Saudi Arabia, were reviewed retrospectively. Patients’ demographic characteristics and preoperative, intraoperative, and 30-day postoperative data were compared between patients who had postoperative SIRS/sepsis and patients who had no complications.
Results:
Ninety-six patients (44%) developed SIRS/sepsis within 30 days after surgery. More than half of the patients were males (55.8%), and the mean age at operation was 56.7(SD=20.0)years. Preoperative high heart rate, low albumin levels, and postoperative intensive care unit (ICU) admission were independently and significantly associated with developing SIRS/sepsis post-operation. The mortality rate in this study was estimated to be 7.5%; of those, 93.8% had SIRS/sepsis.
Conclusion:
The 30-day mortality rate is considerably higher among patients who developed SIRS/sepsis after intestinal obstruction surgery. The independent risk factors of developing SIRS/sepsis after operation were elevated heart rate, low albumin levels preoperation, and ICU admission post-operation.
Keywords
Systemic inflammatory response syndrome
sepsis
intestinal obstruction
risk factors
postoperative systemic inflammatory response syndrome
post-operative sepsis
Introduction
Systemic inflammatory response syndrome (SIRS) is a defensive body response to nonspecific tissue insults caused by either infectious or noninfectious events (e.g., trauma, ischemia, or surgery).[1] If SIRS is accompanied by a microbial pathogenic insult resulting in acute organ dysfunction, it is clinically defined as sepsis.[2] It has been stated that among hospitalized patients, 15% met at least two SIRS criteria, in which higher mortality rates were reported.[1] Sepsis is also a major health concern with high morbidity and mortality. Several studies have demonstrated an increase in the incidence of sepsis over time, now occurring in 6% of all adult hospitalizations and 5% among surgical patients.[3,4]
Non-traumatic acute abdomen (NTAA) accounts for 30% of the surgical admissions, among which intestinal obstruction was one of the most common diagnoses (7.8%).[5] Among the patients who underwent abdominal surgery, 12% had at least one perioperative complication; of those, sepsis/septic shock accounted for 32%.[6]
A higher mortality rate was reported in patients diagnosed with intestinal obstruction accounting for 69% of the patients admitted with acute abdominal pain.[7] A study that was conducted on the pediatric population undergoing intestinal surgery has found that the presence of heart disease, kidney disease, intestinal obstruction, and parenteral nutrition dependence represents significant predictors of postoperative SIRS.[8] However, there have been no studies addressing predictors of postoperative SIRS/sepsis following intestinal obstruction surgery in adult populations.
This study aims to estimate the rate of SIRS and sepsis among patients who underwent intestinal obstruction surgery and to identify the perioperative risk factors leading to postoperative SIRS and sepsis.
Method
This is a retrospective cohort study conducted at King Abdulaziz Medical City (KAMC) in National Guard Health Affairs, Riyadh, Saudi Arabia. The computer database was searched for all patients aged 14 years and older with a diagnosis of intestinal obstruction between January 2015 and December 2020. Intestinal obstruction included small and large bowel, partial and complete obstruction, both mechanical and functional causes, and only patients who underwent intestinal obstruction surgery were included. We excluded patients who were preoperatively diagnosed with sepsis or septic shock and those who had the operation in other hospitals. The data was collected from KAMC using patients’ charts in the BEST Care system. Patients’ data included demographic characteristics (age, sex, and body mass index), preoperative, intraoperative, and 30-day postoperative data. We used the criteria of American College of Chest Physicians/Society of Critical Care Medicine, which state that SIRS is defined by the presence of two or more of the following: a body temperature <36°C or >38°C, heart rate >90 beats/min, respiratory rate >20 breaths/min, CO2 partial pressure of <32 mm Hg, or a white blood cell count >12,000/mm3, <4000/mm3, or >10% of band forms. Sepsis was defined as SIRS with additional clinical evidence of infection.[2,9] All preoperative clinical and laboratory measurements were defined as the last reported values taken before the operation, while postoperative measurements were defined as the reported values are taken 1 day after postoperation. We obtained ethical approval from the Institutional Review Board (IRB) at King Abdullah International Medical Research Center (KAIMRC).
Statistical analysis
The statistical analysis was implemented using Scientific Package for Social Science (PASW Statistics for Windows, Version 22.0, Chicago: SPSS Inc.). Continuous variables were tested for normality assumption using the Shapiro-Wilk test. Normally distributed variables were expressed as mean and standared deviation (SD), while non-normally distributed variables were reported using median (minimum-maximum). Categorical variables were expressed as frequency (percentage). The chi-squared or Fisher’s exact test was used for qualitative variables. Independent samples t-tests and Manne-Whitney U tests were used in the bivariate analysis between the continuous data and the complication status, according to normality. Variables with a high proportion of missing data were not included in the analysis. A multiple logistic regression using the backward stepwise method was applied. All preoperative and operative variables with a P < 0.1 or clinically important were included in the analysis. The model was evaluated using Hosmer-Lemeshow goodness-of-fit statistic (where P > 0.05 presents a good fit). The variables entered in the model were checked for multicollinearity. Odds ratios (OR) and 95% confidence intervals (CI) were estimated. A P < 0.05 was considered to be statistically significant.
Results
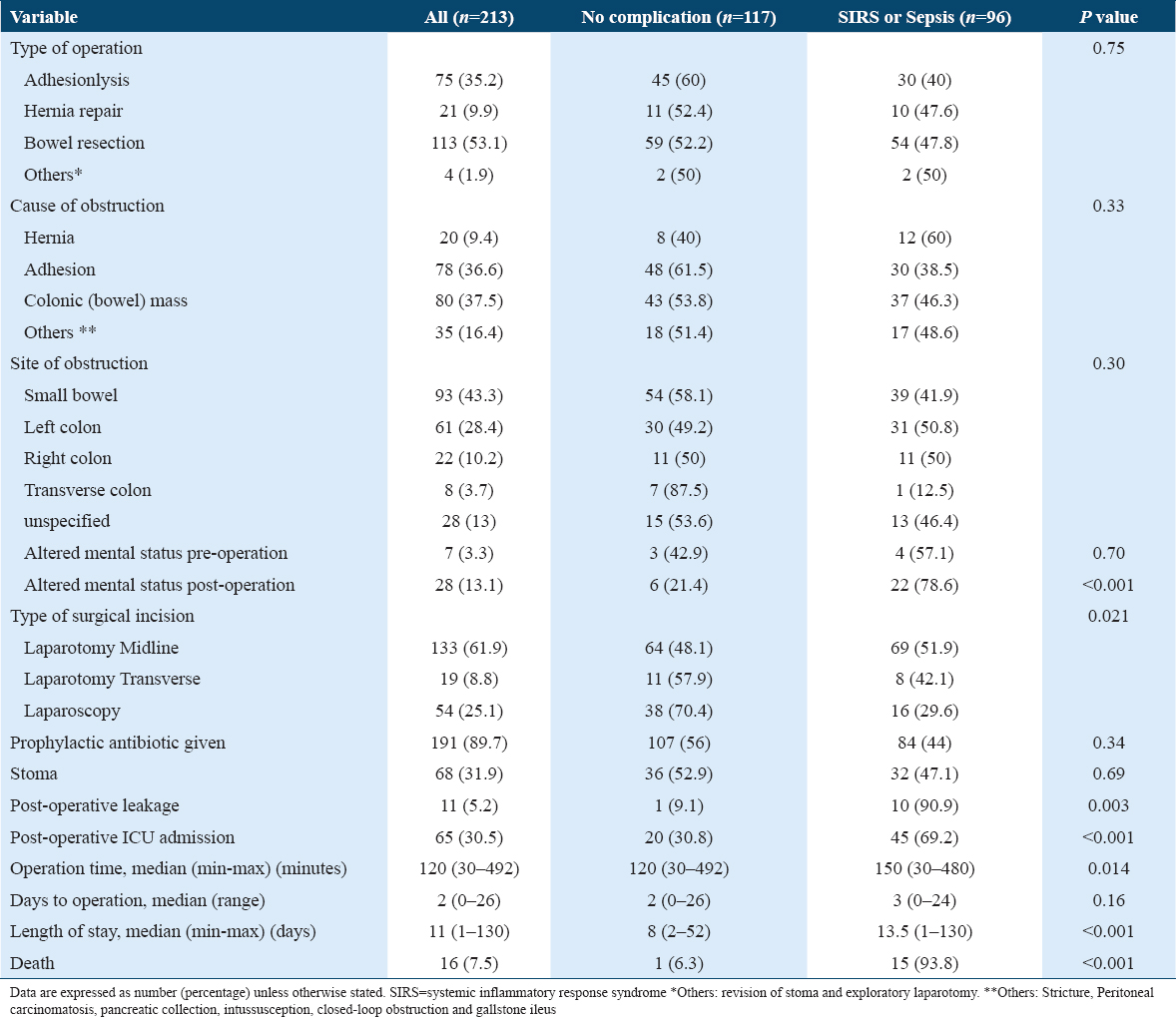
Four hundred eighty-four patients who underwent bowel obstruction surgery were recruited between January 2015 and December 2020. After applying our exclusion criteria, 213 patients remained. Of these, 119 were male (55.8%). The mean age at operation was 56.7 (SD = 20.03) years, and most patients (195 [91.5%]) were functionally independent. The most common comorbidities were hypertension (100 [46.9%]), followed by diabetes mellitus (86 [40.4%]) and cancer (66 [31%]) [Table 1]. Eighty patients had Colonic mass while 78 patients had adhesions accounting for 37.5% and 36.6% of the causes, respectively. Large percentage of the obstruction was at the small bowel (93 [43%]), followed by the left colon (61 [28.4%]), right colon (22 [10.2%]), and transverse colon (8 [3.7%]). Of all patients, 75 (35.2%) underwent adhesiolysis only, while 113 (53.1%) had a bowel resection, with the majority done through midline laparotomy (133 [61.9%]). Sixty-five of the study population (30%) were admitted to the intensive care unit (ICU) post-operatively. The median length of hospital stay was 11 days (range, 1–130 days), and the mortality rate was 7.5% [Table 2].
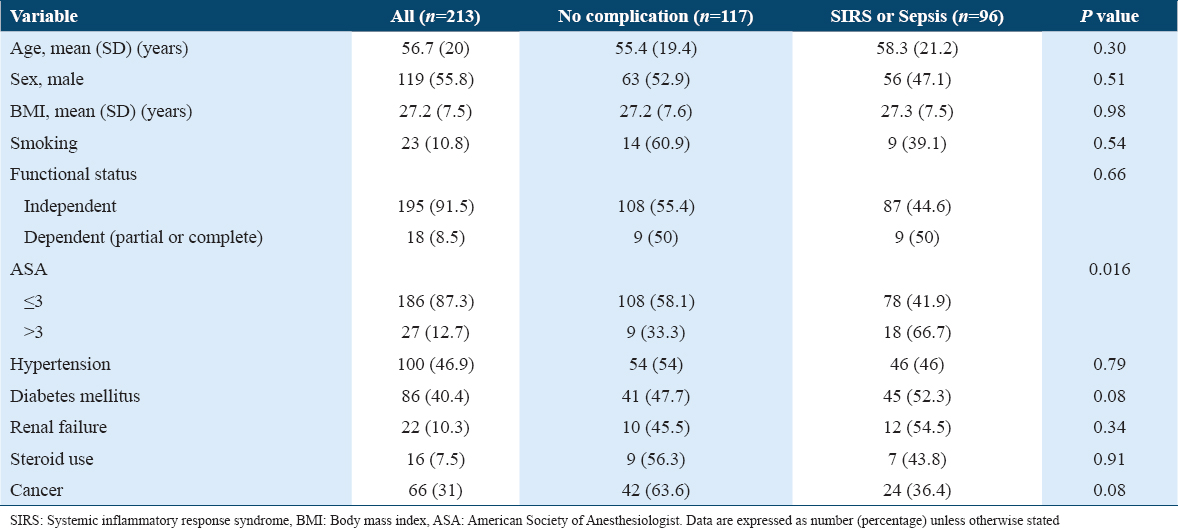
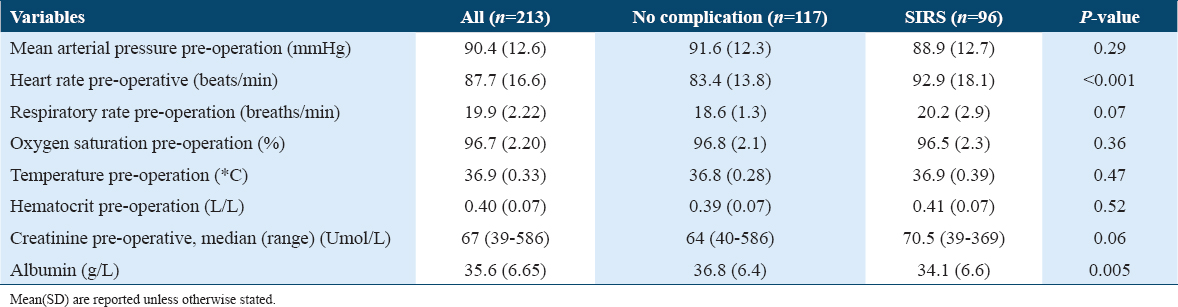
Overall, 96 of the patients (45%) developed postoperative SIRS/sepsis (53 [55%] SIRS; 43 [45%] sepsis). Patients with the American Society of Anesthesiologists Physical Status (ASA PS) Scores of >3 were more likely to have SIRS/sepsis (P = 0.016). Also, those who had increased heart rate (mean = 92.9, SD = 18.1 beats/min) and decreased albumin level (mean=34.1 g/L, SD=6.6 g/L) preoperatively had a significantly higher risk of developing SIRS/sepsis (P < 0.001, P = 0.005) [Tables 1 and 3].
Laparotomy midline incision (P = 0.021) was a significant factor associated with SIRS/sepsis. Patients with SIRS/sepsis had a median operation time significantly longer than those with no SIRS or sepsis (120 vs. 150 minutes, P=0.014). No significant association between no complications and SIRS/sepsis groups in terms of site of obstruction and stoma formation was found (P = 0.303 and 0.690 respectively) [Table 2].
Altered mental status post-operatively has a significant association with SIRS/Sepsis (P < 0.001). Increased heart rate readings (mean = 96.3, SD = 19.2 beats/min) and respiratory rate (mean = 20.7, SD = 4.3) post-operatively were associated with a higher risk of developing SIRS/Sepsis (P < 0.001, P = 0.004). Patients who developed SIRS/sepsis had significantly low hematocrit level (mean=0.36 L/L, SD=0.06 L/L) and high creatinine levels (median= 68 Umol/L; range, 34–446 Umol/L) postoperation (P = 0.022 and 0.011, respectively). Intestinal leakage, evident in Computer tomography (CT), and ICU admission were seen more with the SIRS/Sepsis group (P = 0.003 and < 0.001, respectively) [Tables 2 and 4].
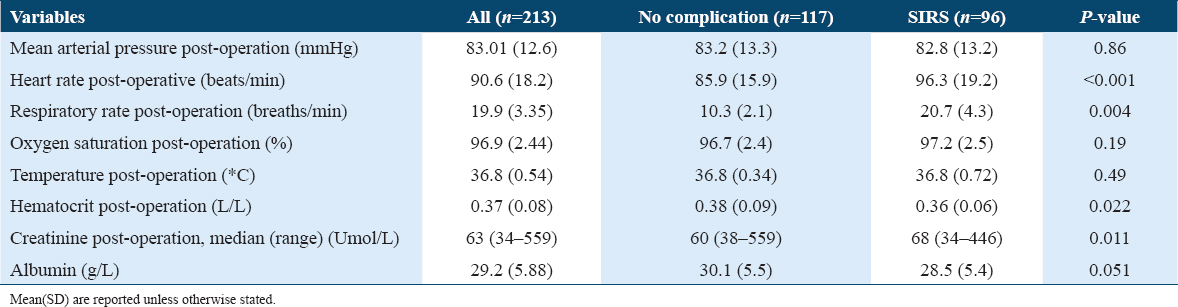
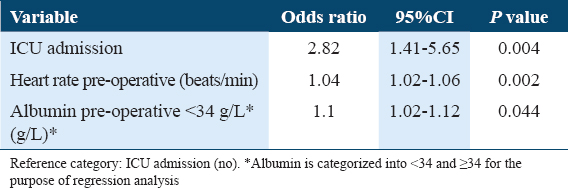
All variables significantly associated with SIRS/sepsis in the bivariate analysis were examined using a multiple logistic regression model. Both preoperative elevated heart rate and decreased albumin levels of < 34 were independently associated with developing SIRS/sepsis but odds ratios do not indicate strong associations (OR 1.04; P = 0.002 and OR 1.2, P = 0.044; respectively). ICU admission post-operation was also found to be an independent risk factor associated with SIRS/sepsis group (OR 2.82; P = 0.004) [Table 5].
The median number of days from surgery to developing SIRS/sepsis was 2 days (range, 0–25 days). Patients with postoperative SIRS/sepsis had a median hospital stay about 5 days longer than those who did not develop SIRS/sepsis (8 vs. 13.5 days, P < 0.001). Of deceased patients, 15 patients (93.8%) had SIRS/sepsis, compared with only one patient (6.3%) of those without SIRS/sepsis (P < 0.001).
Discussion
SIRS and sepsis are considered major health concerns, especially in surgical patients leading to high morbidity and mortality.[6] Knowing the risk factors leading to SIRS and sepsis is essential in early management. In our study, we identify the risk factors of postoperative SIRS/sepsis following intestinal obstruction surgery. We analyzed the data of 213 patients who underwent surgery for intestinal obstruction. Based on our data, we concluded that the incidence of developing postoperative SIRS/sepsis was 45%, with preoperative high heart rate and low albumin levels and admission to ICU as the significant predictors. The mortality rate in this study was estimated to be 7.5%; of those, 93.8% had SIRS/sepsis.
Gabriel et al. have reported that the incidence of sepsis and septic shock following acute abdominal surgery was 2%, with intestinal surgeries being one of the highest risk (OR 1.27; CI 1.12–1.44; P < 0.001).[10] Although it has been conducted in the pediatric population, another study has found that surgeries for intestinal obstruction have significantly increased the risk of postoperative SIRS.[8] This might explain the increased rate of postoperative SIRS/sepsis found in this study.
In this study, colonic mass was the most common cause of intestinal obstruction accounting for 37.5% of our population. This is in contrast with the findings of Khayat et al.[11] and Al-Mulhim,[5] where adhesion was the most common cause of bowel obstruction. The mean age in those studies was 47 and 27 years, respectively, while in our study, the mean age was 56.2 years.[5,11] This might explain the high numbers of colonic mass in our population since older patients (>50 years) are at higher risk of intestinal malignancy.[12]
It has been reported in previous studies that impaired autonomic and cardiovascular function are significantly related to the preoperative heart rate of more than 87 beats/min.[13] This might explain the association between elevated preoperative heart rate with a mean of 86 beats/min and the high risk of developing sirs/sepsis postoperatively found in this study. It has also been proposed that heart rate is a significant independent predictor for the overall survival in patients with septic shock.[14]
Using data from the National Veterans Administration Surgical Risk Study, Gibbs et al. identified low serum albumin level, among many other perioperative risk factors, as a significant predictor of postoperative morbidity and mortality. In addition, after the specific-complication analysis of multiple postoperative morbidities, the highest association was found in predicting systemic sepsis and infective complications.[15] These findings, along with the results of Kumar, are consistent with those reported here.[16] In this cohort, low serum albumin levels of less than 34 g\L preoperation were significantly linked with postoperative SIRS/sepsis as a risk factor.
Admission to ICU post-operation was a significant predictor for developing postoperative SIRS/sepsis. This might be attributed to the prolonged hospitalization of ICU admitted patients with a mean of 27 days, compared to non-ICU admitted patients with a mean of 12 days observed in this study. Therefore, this will make ICU-admitted patients more prone to develop nosocomial infections. These findings are supported by those of other studies, as surgical patients admitted to ICU have a higher incidence of sepsis and mortality.[4,17]
This study is subject to multiple limitations. It is an observational study, and the significant associations found between the different variables do not represent causality. The data were collected retrospectively, which makes it subject to selection and input bias. The variation in data documentation between different surgeons during the study period might have contributed to the unavailability of some measurements. This, together with the missing variables of some included cases, is another limitation. The study population predominantly included patients of older age, and this abnormal distribution might have inflated the overall incidence of SIRS and sepsis of this study.
Broader applicability of the study results might be limited owing to the different evolving definitions of systemic sepsis in clinical practices and previous studies. Another limitation was the variation of the time in which vital signs are taken. Some studies collected the last heart rate measurement before induction of anesthesia, while others considered the heart rate that is measured at the preoperative clinic visit.[18,19] The reported data of this study does not demonstrate the effect of nonoperative management of bowel obstruction, which can be considered as a limitation. Multiple additional variables, including preoperative C reactive protein and erythrocyte sedimentation rate values, preoperative showering, and preoperative shaving, could not be analyzed due to significantly insufficient data. Larger prospective future studies to stratify the results and identify causality are recommended.
Conclusion
The development of postoperative SIRS and sepsis among patients undergoing intestinal obstruction surgery is linked with a considerable increase in the 30-day mortality rate. The independent predictors of post-operative SIRS/sepsis were pre-operatively elevated heart rate, low albumin level, and admission to ICU post-operatively. Identifying modifiable risk factors will potentially minimize post-surgical complications and mortality. Furthermore, differentiating the patients according to those risk factors will help with their management. Consequently, predicting and evaluating ICU stay, hospital length of stay, economic costs, and clinical outcomes are more likely to be achieved.
Authors’ Declaration Statements
Ethics approval and consent to participate
Ethical approval was obtained from the IRB at KAIMRC.
Consent for Publication
Availability of data and material
The data used in this study are available and will be provided by the corresponding author on a reasonable request.
Competing Interests
All authors have no conflict of interest to report.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
ORCID link of the submitting author: https://orcid.org/0000-0002-3618-3297
References
- Systemic Inflammatory Response Syndrome. Treasure Island, FL: StatPearls; 2020.
- Incidence and trends of sepsis in us hospitals using clinical vs claims data, 2009-2014. JAMA. 2017;2017:311241.
- [Google Scholar]
- Incidence and risk factors for sepsis in surgical patients:A cohort study. J Crit Care. 2012;27:159-66.
- [Google Scholar]
- Emergency general admissions. Prospective institutional experience in nontraumatic acute abdomen:Implication for education, training and service. Saudi Med J. 2006;27:1674-9.
- [Google Scholar]
- Two-way interaction effects of perioperative complications on 30-day mortality in general surgery. World J Surg. 2018;42:2-11.
- [Google Scholar]
- Abdominal pain as a cause of acute admission to hospital. J R Coll Surg Edinb. 1992;37:389-93.
- [Google Scholar]
- Profound systemic inflammatory response syndrome following non-emergent intestinal surgery in children. J Pediatr Surg. 2013;48:1936-40.
- [Google Scholar]
- Crit Care Med. 1992;20:864-74.
- Risk factors for post-operative sepsis and septic shock in patients undergoing emergency surgery. Surg Infect (Larchmt). 2019;20:367-72.
- [Google Scholar]
- Incidence and causes of intestinal obstruction in Saudi adults:Tertiary care hospital study. Int Res J Med Sci. 2014;2:22-4.
- [Google Scholar]
- Presentation of cancer to hospital as “acute abdominal pain”. Br J Surg. 1980;67:413-6.
- [Google Scholar]
- Elevated preoperative heart rate associated with increased risk of cardiopulmonary complications after resection for lung cancer. BMC Anesthesiol. 2018;18:94.
- [Google Scholar]
- Serial cardiovascular variables in survivors and nonsurvivors of human septic shock. Crit Care Med. 1987;15:923-9.
- [Google Scholar]
- Preoperative serum albumin level as a predictor of operative mortality and morbidity. Arch Surg. 1999;134:36.
- [Google Scholar]
- A retrospective cohort study of perioperative prognostic factors associated with intra-abdominal sepsis. Anesth Essays Res. 2016;10:50.
- [Google Scholar]
- Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med. 2001;28:108-21.
- [Google Scholar]
- Preoperative fast heart rate:A harbinger of perioperative adverse cardiac events. Br J Anaesth. 2016;117:271-4.
- [Google Scholar]
- Elevated heart rate after noncardiac surgery:Post hoc analysis of a prospective observational cohort study. Br J Anaesth. 2020;124:207-8.
- [Google Scholar]







