Translate this page into:
Staged hip replacement for neglected bilateral Crowe’s Grade 4 dysplasia
Address for correspondence: Mohammed Lafi Al-Otaibi, Department of Orthopedic, College of Medicine, King Khalid University, Abha, Kingdom of Saudi Arabia, PO Box: 960-Postal Code: 61421. Phone: +966502211636. E-mail: mlalotaibi@kku.edu.sa
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Factors such as consanguinity, breech presentation, and family history have been attributed to the diagnosis of developmental dysplastic hip (DDH) in Saudi Arabia. The prevalence of DDH in Saudi Arabia is higher in females than in males, with 10.46 cases per 1000 live births. Cases with bilateral high hip dislocation rarely cause early symptoms and can easily be neglected; therefore, these cases present later in life with degenerative osteoarthritis requiring a challenging hip replacement. This report presents the case of a 54-year-old female with bilateral high dislocated dysplastic hip joints. A successful staged bilateral total hip replacement resulted in painless and stable hip joints. The surgery was conducted successfully by ensuring the availability of personnel with the necessary skills, equipment, and an experienced treatment team. Therefore, the results stress the need to utilize screening tests for the early diagnosis and treatment of developmental dysplastic hip.
Keywords
Crowe’s classification
developmental dysplastic hip
high hip dislocation
subtrochanteric osteotomy
total hip arthroplasty
Introduction
Developmental dysplasia of the hip has a well-known natural history. Treatment methods vary according to the age at which the diagnosis is established. The diagnosis of developmental dysplastic hip (DDH) is delayed in most Saudi patients,[1] which explains the late presentation in some patients. Parents’ consanguinity, positive family history, breech deliveries, and the use of swaddling have been shown to have a direct relationship with the increased incidence of DDH in the Saudi population in the past; however, this may have changed with improved screening protocols and public education. Failure to diagnose and treat DDH early results in delayed treatment, with serious complications such as secondary end-stage osteoarthritis in younger patients, leading to early total hip arthroplasty. Furthermore, late adult presentation of DDH with secondary degenerative osteoarthritis requires hip replacement with a height difficulty index that requires a specialized center and operating team equipped with the necessary skills and equipment for the best obtainable results.[2,3] Several studies have described the severity of hip dysplasia using Crowe’s classification[4] according to the height of the pelvis, medial head-neck junction in the affected hip, and inferior margin of the acetabulum (the teardrop) on anteroposterior radiographs of the pelvis. According to Crowe’s classification, hip subluxation is considered if ≥50% of the femur’s medial head-neck junction is situated above the reference line by at least 10% of the measured height of the pelvis. Considering these relative measurements, dysplastic hips are categorized into four classes based on the amount of subluxation: Class 1, <50% subluxation; Class 2, 50–75%; Class 3, 75–100%; and Class 4, >100%. This is the most widely used classification system for dysplastic hips in adult patients. Crowe’s classification has good reliability and is widely used in orthopedic literature.[5]
Case Description
Patient information
A 54-year-old woman presented with neglected bilateral hip dysplasia with a history of a limp and waddling gait since childhood. She was informed of this condition and was given the required information regarding the natural history of bilateral hip dysplasia with high dislocation. This information provided an explanation for her waddling gait, lumbar lordosis, and late-in-life groin pain, with the sclerotic bone evident in her radiographs of the false acetabulum. She presented with a gradual exacerbation of the right groin pain.
Clinical findings
The patient’s pain had worsened over a year and had markedly interfered with her activities of daily living. She had started to experience pain even at rest and analgesics that had previously provided pain relief were no longer effective. On observation, she had a waddling gait, used a walking frame, and had a lordotic lumbar spine. On examination, her right hip produced pain in all directions of passive movement, with a 0° range of movement of internal rotation. She had a 15° flexion deformity and 10o abduction deformity of the right hip. The left hip moved freely and pain was only produced at the end range of motion, with internal rotation provoking groin pain. There was no noted leg length discrepancy and her distal neurovascular status was intact.
Diagnostic assessment
A radiograph of the pelvis [Figure 1] showed osteoarthritis of the right hip with sclerotic changes in the false acetabulum indicating Crowe’s Class 4 hip dysplasia. Her left hip, with no observed sclerosis, was also considered to exhibit Crowe’s Class 4 hip dysplasia. A computed tomography (CT) scan of the pelvis was performed to evaluate the bone stock and degree of dysplasia [Figure 2]. The CT scan confirmed the severity of her condition and classification as a Type 4 dysplasia, with an approximately 5.5-cm superior migration of both femoral heads and advanced degenerative secondary osteoarthritis of the right hip. Conservative management strategies, such as the modification of activities, physiotherapy, and analgesia, were ineffective.

- Anteroposterior pelvic radiograph. R, right
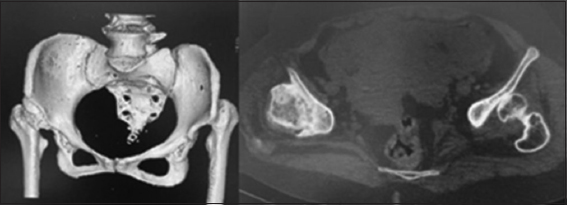
- Computed tomography scan demonstrating a high dislocation dysplasia and right false acetabular sclerosis
The patient was informed that her only option was a total hip replacement of the more symptomatic right hip, with an adaptation for the leg length discrepancy that would be created by the surgical restoration of the normal hip center (presumed to be 5–6 cm). The need for subtrochanteric osteotomy to avoid stretching of the sciatic nerve and all other possible complications of the procedure were also explained to the patient. Regarding the pre-operative workup for the right total hip replacement, her consultations on cardiology and anesthesiology as well as routine laboratory tests were normal.
Therapeutic intervention
The patient underwent a successful total right hip replacement under general anesthesia with the pre-operative use of tranexamic acid to minimize blood loss. She was positioned in the left lateral decubitus position for a modified anterolateral Hardinge hip approach. A curvilinear posterolateral skin incision of the subcutaneous tissue was made, followed by a split made between the proximal third and distal two-thirds of the gluteus medius. Bleeding vessels were cauterized and a careful tenotomy of the gluteus minimums tendon was performed to expose the stretched hip capsule over a severely dysplastic femoral head. The femoral head and arthritic false acetabulum were located approximately 5.5-cm superiorly to the normal anatomical position.
Once the dysplastic tissue had been cleared, the pulvinar, inverted labrum, and true acetabulum were found using the normal anatomical structures, namely, the remnant ligamentum teres, transverse acetabular ligament, and horseshoe of the acetabulum. Distally, the fascia lata and vastus lateralis were split in line with the femoral shaft. A Charnley retractor was inserted carefully to visualize the posterior edge of the acetabulum. The implants used for the total hip replacement were a Continuum shell, multi, 40 CC (Zimmer Biomet, Warsaw, IN, USA); cross-linked polyethylene 40-mm liner (Zimmer Biomet, Warsaw, IN, USA); 28 mm femoral head (Zimmer Biomet, Warsaw, IN, USA); and Wagner cone prosthesis 135/14 femoral stem (Zimmer Biomet, Warsaw, IN, USA). An intravenous injection of rocuronium was administered 1 min before a reduction of dosage to 0.9 mg/kg. The hip was reduced when combined with continuous strong traction of the affected limb with the patient in a position of hip and knee flexion. The hip was reduced without the need for a subtrochanteric femoral osteotomy, likely due to adequate release which was obtained by using the gluteus maximus route, IV rocuronium application, and reduction technique. The sciatic nerve was protected throughout the procedure to ensure that it was not taut or stretched. To protect the sciatic nerve, some of the tight gluteus maximus insertion tendons were resected and the femur was pulled distally. Intraoperative imaging was used to ensure that the acetabular cup and femoral stem were well placed and that no fractures occurred. Post-operative assessment in the supine position revealed that the operated right leg had gained 5.5 cm when compared to the left leg, and the limb was neurovascularly intact. A radiograph of the pelvis was then obtained [Figure 3]. The patient had an uneventful post-operative recovery and she ambulated on day 1 postoperatively with a walking frame and the use of a left shoe raise to correct the leg length discrepancy.

- Post-operative anteroposterior pelvic and right femoral radiographs. R, right
Follow-up
The post-operative follow-up intervals were 2 weeks, 6 weeks, and 3 months. At 12 weeks postoperatively, the patient stated that she was satisfied with her surgery and requested surgery for the left hip which had become increasingly painful. She further complained that her leg length discrepancy was causing her discomfort, due to the high shoe raise. Her recovery at 3-month postoperatively was complete without complication.
Second therapeutic intervention
As a result of Crowe’s Class 4 high dislocation hip dysplasia on the left side, a total left hip replacement was planned and was done at 3-month duration interval from the right hip replacement. The preparation before the second surgery was the same and utilized same radiological tests such as CT of the pelvis, the only difference between the preoperative right and left hips was that the false acetabulum of the left hip was less sclerotic than that of the right. The goal of the surgery was to correct the leg length discrepancy that resulted from the right hip replacement by correcting the center of rotation.
The radiograph obtained in traction confirmed the high dislocation of the left hip. The patient then underwent a successful total left hip replacement performed by the same surgeon with the same setup. The need to correct the leg length discrepancy in the weak dysplastic bone was considered; however, despite using the same technique with the intravenous injection of rocuronium, subtrochanteric osteotomy could not be avoided. The osteotomy was performed after careful pre-operative templating [Figure 4]. The highly dysplastic left hip was templated by measuring the femoral superior migration, which exceeded 5.5 cm. The osteotomy level and length of the femoral segment to be removed were also preoperatively templated. This procedure was performed using the Wagner cone stem implant, which is proven to be suitable for subtrochanteric osteotomy in dysplastic hips due to its stability and versatility for rotation correction. The extremely soft dysplastic acetabulum required the cup-cage technique. The acetabulum was prepared for the trial cup, which was then fixated superiorly and inferiorly with the ic-reinforcement cage (implantcast, Germany). The cage was bent to adapt to the patient’s anatomy, impacted with the patient’s morselized bone graft, and fixed with screws, after which the final cup was inserted. Intraoperative images were used to ensure the correct positioning of all components and the osteotomy level and to prevent potential associated fractures.
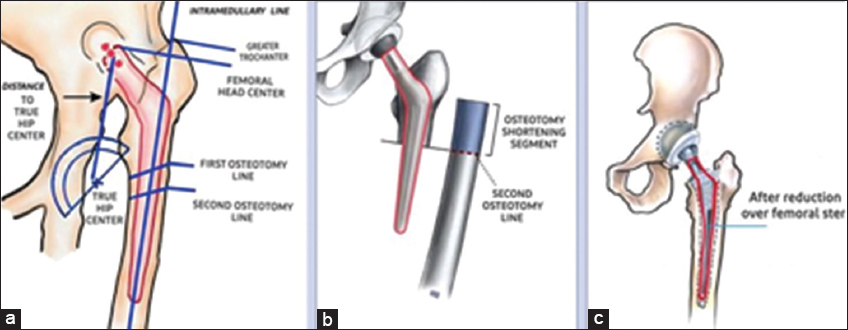
- Post-operative templating for subtrochanteric osteotomy. Templating the Wagner cone size and offset (a); the osteotomy level and segment of femur shortening (b); and final template after procedure completion (c)
Second intervention follow-up
Post-operative assessment of the patient showed equal leg length since the removed bone segment was <1 cm and the left hip was higher preoperatively. Her post-operative pelvic radiograph confirmed the success of the staged bilateral total hip replacements for Crowe’s Type 4 hip dysplasia. After the second surgery, she had an uneventful post-operative recovery and was discharged on post-operative day 5 in good condition, ambulating with a walking frame. She followed the same post-operative visits as for the first operation at 2 weeks, 6 weeks, and 3 months. The patient was able to bear full weight on the right hip on the 1st day postoperatively and partial weight on the left hip for 6 weeks. Her distal neurovascular status was bilaterally intact.
Further follow-ups for both hips took place at 6-month postoperatively, with routine consultations annually for 3 years. At the last visit, her radiograph showed two well-ingrown and fixed hip implants [Figure 5]. She was walking with no complaints of pain, no need for additional analgesia, and minimal assistance of a walking cane as a walking aid.

- Anteroposterior radiographs at 3-year post-operative follow-up
Case outcome
Considering the difficulty factor, we regarded this case as having an excellent outcome. During the 3 years of follow-up, the patient was pain-free, no longer used potentially harmful analgesics, and had recovered functional independence to perform her activities of daily living and mobilize without troublesome walking aids such as walking frames and wheelchairs. The author and patient were aware of all possible complications, such as prolonged surgical time, potential fractures, and osteotomy non-union.[6]
Discussion
Knowledge of the spectrum of anatomical changes in DDH is important when surgical intervention is offered to patients with neglected hip dysplasia. The femur and acetabulum both have a range of changes responsible for the secondary loss of joint endurance required for normal daily activities over time. These changes depend on the degree of dysplasia, age at diagnosis, and type of management offered to the diagnosed patients. Neglected hip joint dysplasia will ultimately require a hip replacement, with unpredictable outcomes due to the associated difficulty.[7] Complications from hip replacement surgeries for neglected DDH were higher than those for primary osteoarthritis. Hip replacements for DDH are considered to have positive outcomes. Hip replacement for neglected hip dysplasia must be performed at specialized centers. For the surgeon to be prepared for any complications during a difficult surgery, the centers should be equipped with a full armamentarium including a wide variety of implants such as modular femoral stem implants, cages, and acetabulum cup sizes.[8] The previous studies have reported that low outcomes should not deter surgeons with the appropriate skills and specialized centers with the appropriate equipment from offering total hip replacements to patients suffering from neglected DDH with a high Crowe’s classification class. More recently, the higher survival rates of these procedures reflect the improvement in surgical skills and implant technology.[9] The results depicted in this case report confirm that good outcomes can be achieved in difficult hip replacements for DDH.[10]
Conclusion
Total hip replacement is an effective and reproducible procedure for a neglected developmental dysplasia of the hip with a higher Crowe’s classification. Careful patient selection and preparation for dealing with potential challenges are crucial to avoid complications. Avoiding subtrochanteric osteotomy may not always be possible, but when necessary, it should be performed to avoid complications such as stretching of the sciatic nerve or a resultant high center of rotation of the hip.
Author’s Declaration Statements
Patients consent
Written informed consent has been taken from the studied patient.
Availability of data statement
The data used in this study are available and will be provided by the corresponding author on a reasonable request.
Conflicts of interests
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflicts of interest.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for-profit sectors.
Ethics approval
Ethical Clearance Certificate Approval No. ECM#2021-5907 on November 23, 2021 by Research Ethical Research Ethics Committee at King Khalid University (HAPO-06-B-001), Abha, Kingdom of Saudi Arabia. Informed consent was obtained.
Acknowledgments
The author would like to thank Editage (www.editage.com) for their writing support and English language editing.
References
- Developmental dysplasia of hip:Perspectives in genetic screening. Med Sci (Basel). 2019;7:59.
- [Google Scholar]
- Developmental dysplasia of the hip (DDH) in Saudi Arabia:Time to wake up. A systematic review (1980-2018) Open J Epidemiol. 2020;10:125-31.
- [Google Scholar]
- Arthroplasty for neglected high developmental dysplasia of the hip. Hip specialist or general orthopedic surgeon. Asian J Arthroplast. 2017;2:37-43.
- [Google Scholar]
- Is pseudoacetabulum an important factor determining SSTO application in total hip arthroplasty for Crowe IV hips?A retrospective cohort study. J Orthop Surg Res. 2019;14:201.
- [Google Scholar]
- Total hip replacement in developmental hip dysplasia:A narrative review. Cureus. 2021;13:e14763.
- [Google Scholar]
- Total hip arthroplasty for crowe Type IV hip dysplasia:Surgical techniques and postoperative complications. Orthop Surg. 2019;11:966-73.
- [Google Scholar]
- Current concepts in developmental dysplasia of the hip and total hip arthroplasty. Arthroplasty. 2019;1:2.
- [Google Scholar]
- Survival rates and reasons for revision of different stem designs in total hip arthroplasty for developmental dysplasia:A regional registry study. J Orthop Traumatol. 2021;22:29.
- [Google Scholar]
- Implant survival after primary total hip arthroplasty due to childhood hip disorders:Results from the Danish Hip Arthroplasty Registry. Acta Orthop. 2008;79:769-76.
- [Google Scholar]
- A reduction technique of arthroplasty without subtrochanteric femoral shortening osteotomy for the treatment of developmental high dislocation of hip:A case series of 28 hips. J Arthroplasty. 2014;29:2289-93.
- [Google Scholar]







