Translate this page into:
Synergy between psychological impact and biochemical manifestation of stress among the COVID-19 pandemic-affected population
Address for correspondence: Aisha Farhana, Department of Clinical Laboratory Sciences, College of Applied Medical Sciences, Jouf University, Al-Jouf, Saudi Arabia. E-mail: afarhana@ju.edu.sa
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
ABSTRACT
Objective:
Due to the COVID-19 pandemic, many countries around the world experienced an unprecedented increase in stress in the general population. Even after normal life has been reestablished, the new normal is punctuated by severely impacted vulnerable groups. Stress-associated symptoms display an intricate relationship with biochemical modulations, which coordinate the stress response. Identifying these biochemical factors is inherent to deciphering the mode of treatment needed to diminish the health-care gap resulting from the pandemic.
Methods:
We applied psychological measures using the perceived stress (PS) and COVID-19 anxiety (CA) scales and preventive health behavior (PHB) to evaluate stress in the general population. Biochemical markers of stress, that is, total antioxidant capacity (TAC), thiobarbituric acid reactive substances (TBARS), cortisol, and C-reactive protein (CRP) were tested in the serum samples of the participants. Statistical analysis was carried out using SPSS version 22.0.
Results:
Stress scores for PS, CA, and PHB indicate the prevalence of moderate-to-high stress among participants, and a correlation between psychological stress and biochemical correlates, TAC, TBARS, cortisol, and CRP. Serum concentrations of TBARS, Cortisol, and CRP were found to be significantly increased, while the TAC was decreased across all stress types and levels. Our findings demonstrate a positive correlation between PS, CA, PHB TBARS, cortisol, and CRP and a strong negative correlation with TAC.
Conclusion:
The results of this study will help in tailoring targeted interventions and preventive regimes to mitigate COVID-19-associated anxiety and stress disorders prevailing even after the actual pandemic has subsided.
Keywords
Antioxidants
anxiety
cortisol
COVID-19
C-reactive protein
perceived stress
preventive health
thiobarbiturate reactive substance
Introduction
Globally, COVID-19 pandemic has reverberating consequences that led to the prevalence and persistence of anxiety, distress, and worry among populations. The stress associated with the fear of contracting the virus, family becoming sickened, isolation and quarantine measures, distress about separation from the family members, and the fear of long-term impacts of the global disruption served as a ground for the development of many physical and emotional disease conditions. Although the effect of the pandemic on the general population has been quite heterogeneous, with sporadic reports of stress resilience or no effect in some people, largely, the pandemic reflected a constant mental battle for a majority of people across the globe. In India, from January 2020 to September 06, 2023, there have been 44,997,326 confirmed cases of COVID-19 with 532,023 deaths. WHO (2023) attributing COVID-19 as a major health crisis, threatening people’s lives and affecting their mental health leading to stress, anxiety, and depression.[1-3] The WHO reported that during the first year of the pandemic, the prevalence of anxiety and depression demonstrated a 25% increase worldwide,[4] which increased to 27.8% in 2023. Many studies demonstrated an impairment of cognitive functions and psychiatric disorders associated with the COVID-19 pandemic.[5-8]
The persistence of stressful conditions induces the body to follow an array of biochemical modulations aimed at correcting the imbalances and coordinating the stress response. A series of stress mediators are released within different temporal compartments of the body in a pattern specific to the type of stress and the level of individual resilience. This generates a diverse degree of susceptibility and resistance patterns. Relentless stress depletes the body’s ability to counter diseases and infections and affects the social aspects of a healthy life. In connection to the COVID-19 pandemic, two main features affecting mental health have been identified; the first relates to the fear of contagion, which may increase the perceived threat, causing panic, behavioral contagion, and an emotional epidemic.[9-11] The second relates to multiple and rapid changes to social, work-related, and familial habits due to social distancing measures.[12-14] The diagnosis involves the characterization of mental illnesses with qualitative and subjective measures of stress. However, these indices often lead to misdiagnosis and relatively imprecise insight into the severity of the condition. Furthermore, social stigmatization encompassing mental health is also a cause of non-compliance to the therapy or hesitation in seeking medical aid.
Psychiatric assessments for mental illness, when combined with laboratory investigation, may provide insights into the factors that determine the initiation and progress of prolonged psychological diseases. Studies have demonstrated an association between persistent psychological stress and an imbalance in oxidant-antioxidant homeostasis. An uncontrolled increase in oxidative stress identified by total antioxidant capacity (TAC) and thiobarbituric acid reactive substances (TBARS) triggers a multimodal stress response involving the neuroinflammatory, neuroendocrine, and metabolic junctions.[15] The neuroinflammatory processes hold significance in the manifestation of psychological stress, wherein the normal function of the immune system is negatively impacted. An alteration in the body’s TAC is associated with sleep disorders, depression, anxiety, and the development of neuropsychiatric disorders.[16]
The effect of stress manifested through the neuroinflammatory axis can be determined through C-reactive protein (CRP). The elevation in the CRP level is an indicator of chronic stress and may contribute to linking stress to low-grade inflammation and associated diseases. Many studies have demonstrated a correlation of CRP with the severity of disease in COVID-19 patients. CRP is also shown to be a good indicator of clinical outcome in many diseases.[17,18] Similarly, cortisol, a major player in the modulation of psychological and physical stress response is an indicator of the persistence of stress.[19] Cortisol significantly impacts metabolic functions as a response to stress.[20] Being a major regulator of neuroendocrine axis, an increased level of cortisol can lead to an increase in blood sugar, alterations in blood pressure, and suppression of the immune effectors.[21] Understanding the specific biomarkers and manifestation of psychiatric symptomologies can help in identifying the severity and extent of stress. Subsequently, this can provide insights into the critical mechanisms needed for the development of potential therapeutic and preventive interventions.
This study integrates the psychological indicators of stress with serum biochemical markers, providing a foothold in understanding the level of stress and associated mechanisms. Such information can help practitioner to identify stress and determine the course of treatment, and policymakers to develop mechanisms for restoring and promoting psychological health in the population.
Materials and Methods
Participation and sampling
This study was conducted from August 2021 to December 2022. The participants were informed about the study and a written consent was obtained from all participants. This cross-sectional study included 207 participants who were negative for COVID-19 quantitative polymerase chain reaction and have not had any episode of COVID-19 before or during the study. The study population prospectively included those attending the general medicine of the outpatient clinic of Era’s Lucknow Medical College and Hospital, India. To meet the objectives of the current study, four measures namely: COVID-19 anxiety scale (CAS); perceived stress scale (PSS); preventive health behavior (PHB) scale, and demographic information bank (DIB) were used. The participant was given access to the online Google forms to complete the surveys, which also included information regarding the research objectives, confidentiality of the data, freedom to withdraw, and contact of the responsible researcher. The questionnaire starts with the informed consent to participate in this study. Participants can access the questionnaire only if they consented and agreed to participate in the study. The questionnaire took approximately 15–20 min to fill. The completion of questionnaires was tracked and the date and time of the survey were noted. The participation in the study was solely on a voluntary basis and no compensation or incentive was offered. The instructions in the study indicated that; participation in the study was anonymous answering questions was voluntary and the participants can withdraw anytime. The data collected through this study are for research purposes only. The exclusion criteria were age, and only adults (above 18 years) were included in this study. Participants who had any episode of COVID-19 infection previously or during the study were excluded from the study.
Measures
Sociodemographic information blank
DIB includes information regarding age, gender, education level, marital status, personal monthly income, residential area, occupation and history of COVID-19 infection or disease, or other illness, and overall health index, of the respondents. The data were obtained through questionnaires, with a total of 207 respondents, wherein, 57 questionnaires were incomplete and were excluded from the study. Finally, a total of 150 participants 75 females and 75 males were included in the study.
The CAS; Silva et al. 2020
The 7-item CAS was used to measure anxiety. In CAS, the participants indicated how much each item reflected their behavior in the last months, regarding COVID-19. A 4-point scale (0 = not applicable to me and 3 = very applicable to me) was used. The level of anxiety was measured by averaging the participants’ scores. The overall score ranged between 0 and 21. The higher the average, the greater the anxiety of the individual regarding COVID-19. Cronbach’s alpha score on the scale was 0.89 and for the current sample, it was 0.861.
PSS; 10-item version (PSS10; Cohen et al., 1983)
The PSS10 is used to assess the respondents’ perceived stress (PS) due to the COVID-19 pandemic. This scale was originally compiled as a global 14-item based measure to evaluate the degree of stress caused by factors considered to be unpredictable, uncontrollable, or overwhelming.[22,23] The 10-item version of the PSS was used in this study. Items were rated on a five-point Likert scale ranging from 1 (not at all) to 5 (very much). Participants have to respond according to their feelings or thoughts of COVID-19 for the past month. Of the total, four items (PS4, PS5, PS6, and PS7) were reverse items. The higher the score, the more stressful will be for the respondents. The PSS10 demonstrated good internal consistency (α = 0.801). In the current sample, it was 0.756.
PHB; Brug et al. 2004
COVID-19-related PHB was measured by adapting items from the study of Brug et al., who assessed SARS-related precautionary behaviors.[24] There were 16 items on the scale, four items specific to COVID-19 were added, with a total of 20 items. The scale has a total of 20 items rated on a 5-point Likert scale (5 = “always” and 1 = “never”); a higher score implied a better degree of practice of preventive behaviors. A higher score presents greater engagement in PHB against COVID-19. The Cronbach’s alpha reliability of the scale in this study was 0.890.
Overall physical health (Ware and Sherbourne, 1992)
The Rand 36-item health survey (SF-36) integrates eight concepts of health including physical functioning, body pain, physical health problems, personal/emotional problem-related limitation, emotional well-being, social functioning, energy/fatigue, and general health perceptions. In addition, one item-based indication of perceived change is associated with health. The 36 items in SF-36 are adapted from extensive instruments filled by participants in the Medical Outcomes Study (Hays and Shapiro, 1992; Stewart, Sherbourne, Hays, et al., 1992).[25] The height and weight were obtained by trained personnel with a Tanita brand scale (model bc-533) and a measuring tape attached to the wall, which was used to calculate the body mass index (BMI). The hip and waist circumferences were also obtained by trained personnel using a measuring tape, and these measurements were used to calculate the waist-to-hip ratio.
Blood collection and laboratory investigations
Early morning blood samples (8 mL) were collected after 8–10-h fasting, in a blood collecting tube (Vacuum II, Villfend Corporation). Sampling was carried out by a phlebotomist, and the sample was transferred to the laboratory. The serum was separated by centrifugation and stored at −80°C until further analysis. Before sampling, the participants were informed about the sampling and protocols of the study in a simple and common language. Participants who agreed were asked to fill an informed consent form before sample collection.
Measurement of TAC
The serum TAC of the samples was assessed by ferric-reducing antioxidant power (FRAP) assay.[26] The method follows a simple, quantitative, and automated colorimetric assay to determine the TAC for biological fluids by their ability to reduce ferric compounds. On reduction of ferric tripyridyltriazine complex to its ferrous form, the intense blue color of the complex is changed. This change is measurable through spectrophotometric assessment, and the difference in the absorbance is used to calculate TAC. The FRAP assay was carried out using a TAC kit (Merck, MAK187), according to the manufacturer’s protocol. The result is considered statistically significant when P < 0.05.
TBARS assay
The assay was carried out in serum using the TBARS (TAC Method; Assay Kit Item No. 700870, Cayman Chemicals). This assay allows indirect estimation of lipid hydroperoxide in human serum. The measurement was done according to the manufacturer’s protocol, using malondialdehyde as a standard. The reaction with TBARS analyzed the level of lipid peroxidation at 37°C at 535 nm and a molar extinction coefficient of 1.56 × 105/M/cm. The results were expressed as nM TBARS/min/mg.
Cortisol assay
Serum cortisol was measured in the serum sample using the enzyme-linked immunosorbent assay (ELISA), with absorbance at 450 nm (Cortisol ELISA Kit -ab108665, Cambridge, UK) in the serum samples, in accordance with the manufacturer’s instructions. The samples and standards were run in triplicate. The detection limit for cortisol was 0.1 μg/dL with inter- and intra-assay variations of <5.6% and 7.2%. The sensitivity of the test method was 96% and specificity was 93%. The kit demonstrates no cross-reactivity.
CRP testing
The serum samples were tested for CRP using the human CRP ELISA Kit (CRP - ab260058, Abcam), according to the manufacturer’s protocol. Briefly, the protocol was based on the colorimetric assessment using the sandwich ELISA method. The sensitivity of the method was 5.36 pg/mL and covered a range between 18.75 pg/mL and 1200 pg/mL. The test assay has a 100% sensitivity 94% specificity and 0% cross reactivity.
Statistical testing
The data were statistically analyzed using SPSS, v24 (IBM SPSS Software, Chicago, IL, USA). The results are presented as bars and scatter dots with information about the mean and SD. All relevant statistical information is presented in the figure legends. Spearman’s correlation coefficients (r) were used to evaluate the association between the variables. The values of “r” between 0.2 and 0.39 were considered as weak, between 0.4 and 0.59 as moderate, and between 0.6 and 0.79 as a strong association between the tested variables. The P < 0.05 were considered statistically significant.
Ethical statement
The study protocol was approved by the Institutional Ethics Committee with the reference number ELMC & H/20 21R-cell/178. The study was conducted with full consideration regarding participant well-being amidst pandemic-related stress, as mentioned in the participation and sampling section (Section 2.1).
Results
Sociodemographic characteristics
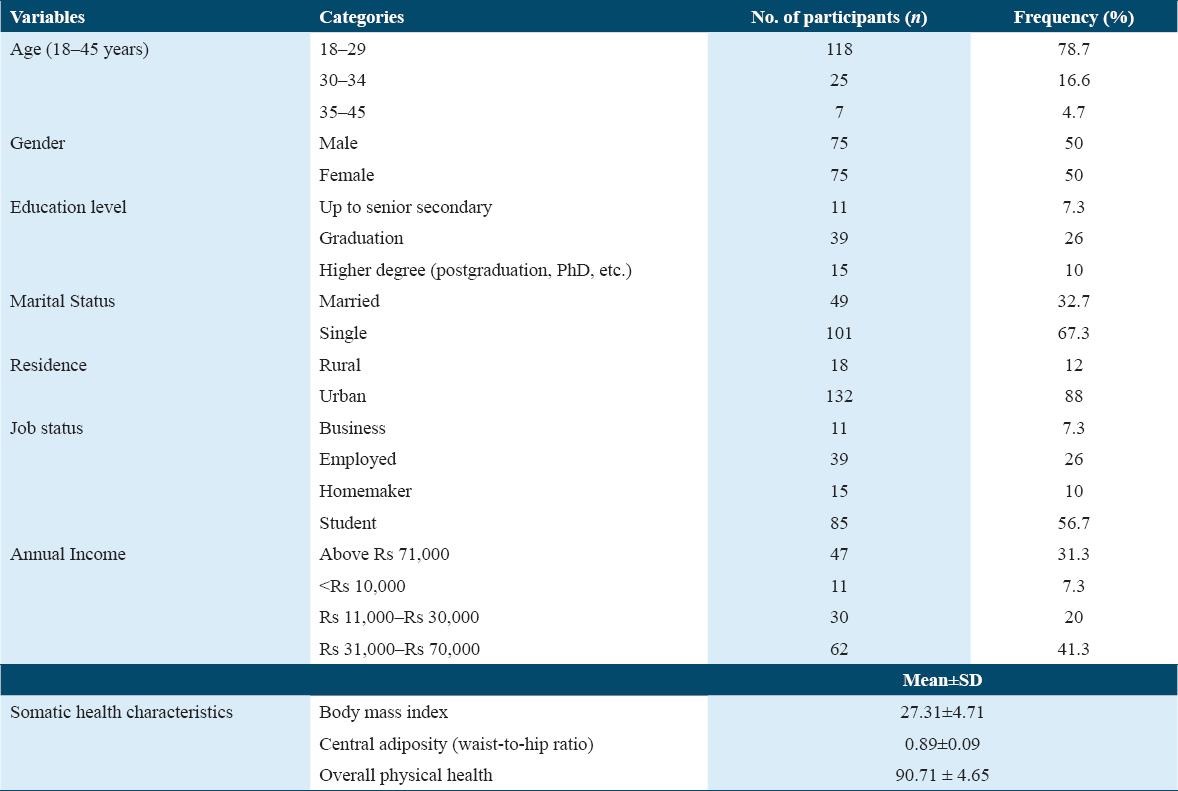
Table 1 depicts that majority of the participants 118 (78.7%) were in the age group of 18–29 years, 25 (16.7%) were between 30 and 34 years, and 7 (4.7%) were between 35 and 45 years. The gender information shows that male and female respondents included in the study were equal 75 (50%). The information for the educational profile indicates that 7 (4.7%) were educated up to a certificate course or a diploma, 54 (36.0%) were graduates, 80 (53.3%) were post-graduates or PhD, 9 (6.0%) were educated up to intermediate, and 3 (2%) were educated up to high school. The educational profile reflects that most of the people in the study were highly educated up to post-graduation or PhD. The marital status of the group shows that 49 (32.7%) were married and remaining 101 (67.3%) were unmarried (single, widowed, or divorced). With regards to the job status of the respondents, data indicate that 11 (7.3) of them were businessmen, 39 (26%) were employed, 4 (2.7%) were homemaker, 85 (56.7%) were students, and 11 (7.3%) were unemployed. Hence, the overall profile indicates that most of the respondents were students. The income profile of the study population shows that 47 (31.3%) have a monthly income above 71,000 INR, 11 (7.3%) have an income <10,000 INR, 30 (20%) people have an income within the range of 11,000–30,000 INR, 35 (23.3%) have an income within the range of 31,000–50,000 INR and 27 (18%) of the participants have an income between 51,000 and 70,000 INR. Overall, the monthly income of the respondents was over 71,000 INR. The residential status shows that 18 (12.0%) people belonged to the rural area whereas 132 (88%) belonged to the urban area indicating that most of the respondents were from the urban area. The physical health characteristics showed a BMI with a mean ± SD of 27.31 ± 4.71, a central adiposity of 0.69 ± 0.09 (mean ± SD), and an overall physical health index of 90.71 ± 4.65 (mean ± SD), which reflects that most of the respondents were in good health condition. A total of 207 questionnaires were received, however, incomplete responses, participants with any chronic health conditions such as diabetes, heart problems, and respiratory conditions were excluded from the study. The total number of participants after the exclusion of incomplete questionnaires, and people with chronic disease was 150.
Psychological distress
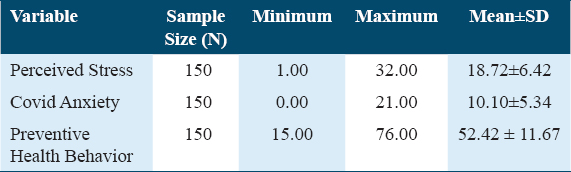
Table 2 demonstrates that the mean and SD of PS was 18.72 ± 6.42, with minimum and maximum values being 1.00 and 32.00. Similarly, the mean and SD of COVID-19 anxiety (CA) was 10.10 ± 5.34, with 0.00 and 21.00 as minimum and maximum values. The mean value and SD of PHB were 52.42 ± 11.66, with 15.00 and 76.00 being the minimum and maximum values. Table 3 and Figure 1 demonstrate the level of stress for each variable, indicating the prevalence frequency of low, moderate, and high stress levels. The range was low at ≤7.00 for CA, ≤17.0 for the PS, and ≤49.00 for PHB. The stress was considered moderate within the range of 8.00–13.00 for CA, 18.00–21.00 for PS, and 50.00–58.00 for PHB. A score of >22.00 for PS, >14.00 for CA, and >59.00 for PHB was considered high. Of the total, 64 (42.7%) of participants experienced low levels of stress, 39 (26.0%) had moderate, and 47 (31.3%) experienced high levels of stress. The majority of adults, 86 (57.3%), had moderate-to-high levels of stress. In addition, 68 (45.3%) respondents had a low level of anxiety, 36 (24.0%) had moderate, and 46 (30.7%) had a high level of anxiety. More than half of the adults, 82 (54.7%), experienced moderate to high levels of CA stress. Furthermore, Table 4 demonstrates a significant difference between males and females was observed in PS (P = 0.003) and CA (P = 0.000). In contrast, no significant difference was present between male and female participants in PHB (P = 0.143).
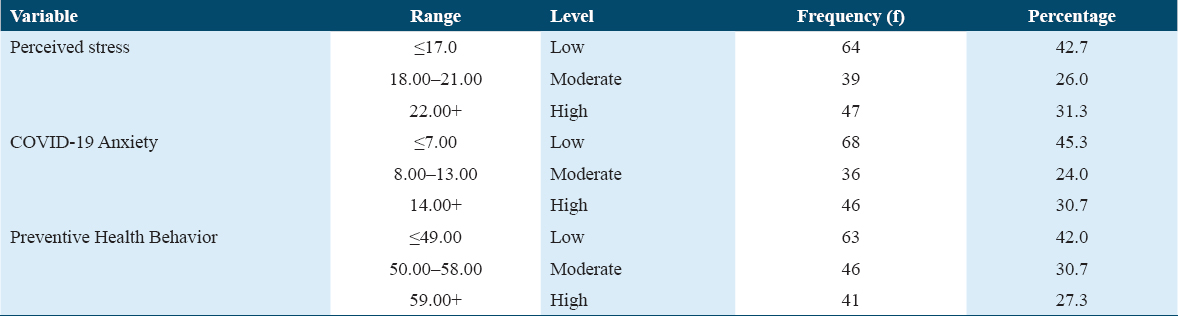
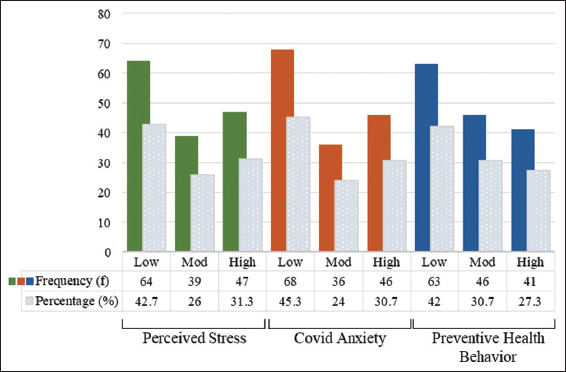
- The distribution of low, moderate, and high-stress levels in different stress conditions. The colored bars represent the frequency at which each stress is prevalent in the study population. The green is representative of low, high, and moderate stress in the perceived stress category, orange for COVID-19 anxiety, and blue for preventive health behavior. Grey bars represent the percentage reflecting the frequency for each group (low, moderate, and high)
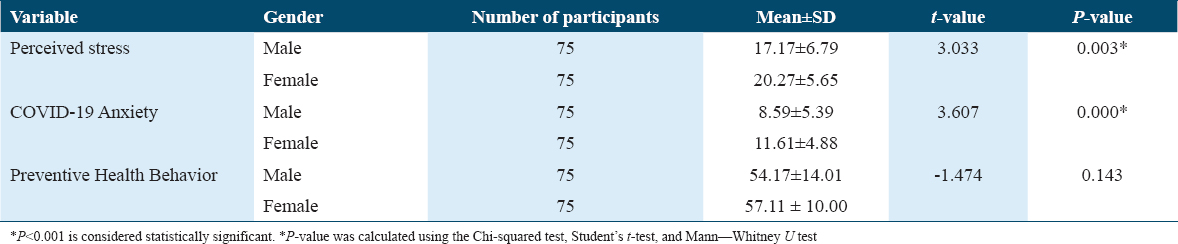
An independent t-test was performed to compare the mean scores of male and female adults on PS, CA, and PHB. As shown in Table 4, the mean score for PS for males (M = 17.1733, SD = 2.787) and the mean score for females (M = 20.273, SD = 1.623) was similar. The mean difference of 3.033 was significant at P < 0.01 (t = 3.033, P = 0.003). For CAS, there was a significant difference in the mean score for males (M = 8.5867, SD = 2.387) and females (M = 11.613, SD = 2.876; t = 3.607, P = 0.000). Moreover, the difference in the mean score of PHB for males (M = 54.173, SD = 14.014) and females was not significant (M = 57.106, SD = 10.003; t = 1.474, P = 0.143).
We observe a prevalence of moderate-to-high levels of stress and anxiety among the participants in general and women in particular. In addition, adherence to the recommended PHBs, such as wearing masks and maintaining social distancing was inadequate. The results further revealed different levels of stress, anxiety, and health behavior significantly linked with an elevated level of biochemical indices such as serum cortisol, TAC, TBARS, and CRP (Figure 3). The increased level of these biomarkers adversely affects the health parameters. The results emphasize the need that special attention should be given to the mental health problems of the population in general and women in particular, as they are more susceptible to stress and anxiety.
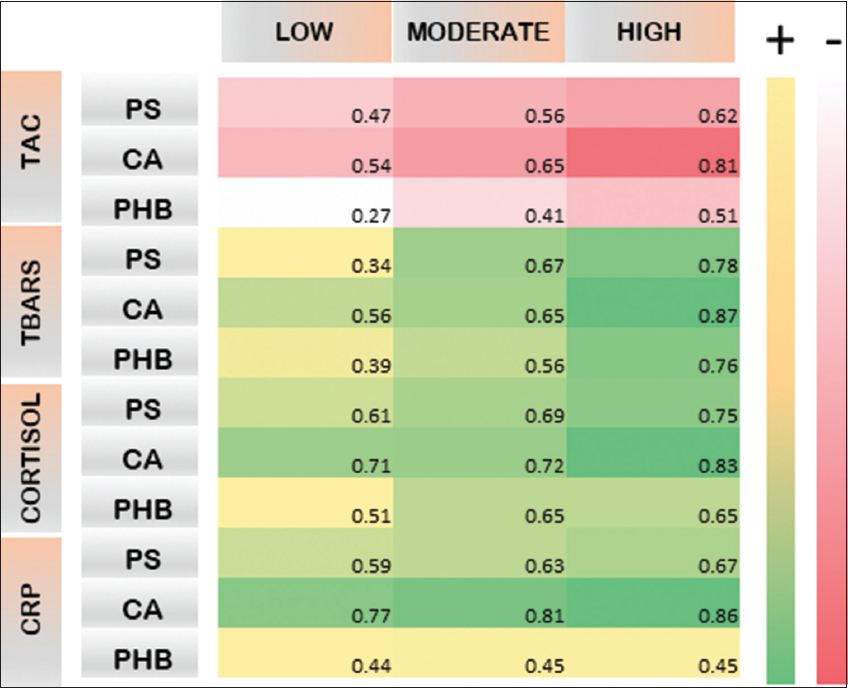
- Heat map of correlation between biochemical markers and low, moderate, and high stress within PS, CA, and PHB categories. The heat map demonstrates the degree of correlation between stress levels (low, moderate, and high) and the four metabolites (TAC, TBARS, Cortisol, and CRP), which were found to be significantly altered in serum in stress conditions. The heat map is generated for all three stress categories: PS, CA, and PHB. The adjusted P-values are set at P < 0.05. The red bars indicate a negative (-) correlation, and the green bars indicate a positive (+) correlation. PS: Perceived stress, CA: COVID-19 anxiety, PHB: Preventive health behavior, TAC: Total antioxidant capacity, TBARS: Thiobarbituric acid reactive species, CRP: C-reactive protein, “+” represents positive correlation, and “-” represents negative correlation
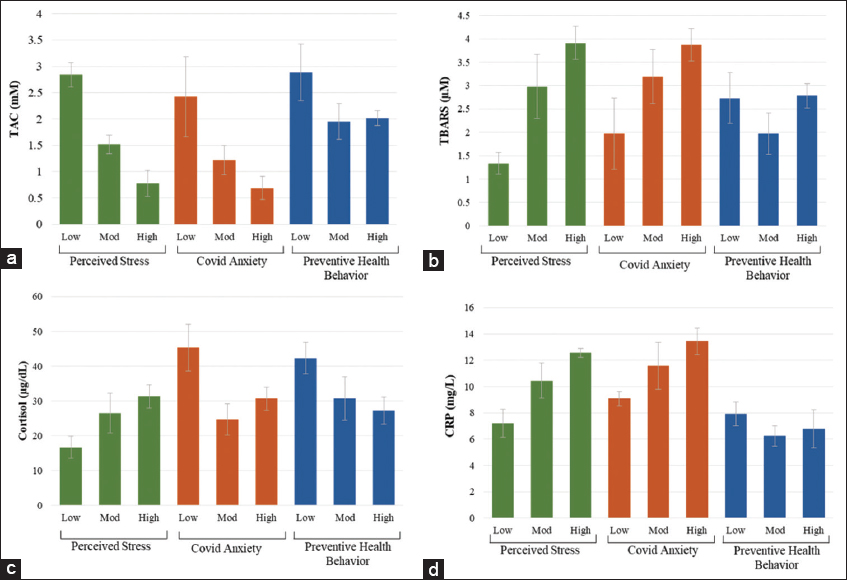
- The effect of low, moderate (mod), and high levels of stress on biochemical indices of (a) Total antioxidant capacity, (b) Thiobarbituric acid reactive substances, (c) cortisol, and (d) C-reactive protein. The data indicate the difference between each biomarker at different stress levels in three subsets: perceived stress, COVID-19 anxiety, and preventive health behavior. Each stress is color coded with green for perceived stress, orange for COVID-19 anxiety, and blue for preventive health behavior
Psychological distress associated biochemical alterations
Table 5 and Figure 3 indicates that psychological stress is correlated with significant changes in the blood biochemistry, and these alterations arbitrate the level of stress. A decrease in TAC was observed in PS, with a mean ± SD of 2.84 ± 0.29 in low stress, 1.02 ± 0.56 in moderate stress, 0.78 ± 0.29 in high stress. There was a significant difference in TAC concentrations between high- and low-stress levels, while no significant change was observed between moderate and high-stress values. The results indicate the presence of low total antioxidant status in the participants. To further assess the oxidative profile of participants, TBARS was measured in the same serum samples. TBARS measures lipid peroxidation indicating oxidative damage. TBARS was found to be higher in high level of stress in PS category as well as CAS and PHB categories. The svalues were significantly higher in PS, ranging 1.34 ± 0.33 in low, 2.98 ± 1.01 in moderate, and 3.91 ± 1.21 in high stress. Similarly, the CAS group also demonstrated a high concentration of TBARS equal to 1.97 ± 0.98 in low, 3.19 ± 0.76 in moderate, and 3.87 ± 0.91 in high stress. In PHB, the level of TBARS was 2.73 ± 1.26 in low, 1.97 ± 1.14 in moderate, and 2.78 ± 1.15 in high stress. The difference between the low and high stress was non-significant.
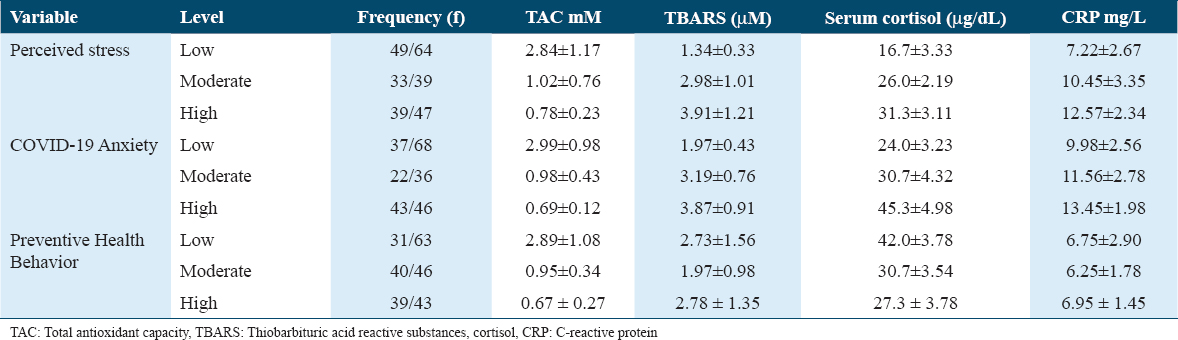
To evaluate the neuroendocrine axis of stress, we determined the serum cortisol concentrations in the participants. High concentration of cortisol was found to be associated with high levels of stress and as a cause for a range of physical and mental health disorders. In the PS category, low stress was 16.7 ± 3.33, moderate stress 26.0 ± 2.19, and high stress 31.3 ± 3.11, respectively. In the CA category, serum cortisol values were 24.0 ± 3.23 in low stress, 30.7 ± 4.32 in moderate stress, and 45.3 ± 4.98 in high-stress groups. In the PHB category, low stress was associated with a serum cortisol of 27.3 ± 3.78, moderate stress with a serum cortisol concentration of 30.7 ± 3.54, and high stress with a serum cortisol concentration of 42.0 ± 3.78. We observed that high stress correlates with a high concentration of cortisol in all three categories. Furthermore, the range of increase in cortisol is higher in CA and PHB than in PS.
We also assessed the neuroinflammatory axis of stress transduction by analyzing serum CRP. Being a non-specific indicator of inflammation, even a slight to moderate increase in CRP can be used as an early indicator of the production of cytokines. Our study observed that in the PS category, CRP was 7.22 ± 2.67 in the low-stress group, 10.45 ± 3.35 in moderate-stress group, and 12.57 ± 2.34 in the high-stress group. In the CA category, CRP was 9.98 ± 2.56 in low stress, 11.56 ± 2.78 in moderate stress, and 13.45 ± 1.98 in high stress. However, the level of CRP was 6.75 ± 2.90 in low, 6.25 ± 1.78 in moderate, and 6.95 ± 1.45 in high-stress groups in the PHB category. Overall, the values of CRP were considerably close to the normal range in low, moderate, and high stress in the PHB category.
A link has been demonstrated between chronic psychosocial stress and CRP, which can subsequently lead to the development of diseases associated with low-grade inflammation; CRP may be an important indicator of stress with a propensity for disease progression in patients.
Correlation between psychological stress level and biochemical markers
To ascertain the correlation between stress and its biochemical effectors, we carried out Spearman’s rank correlation analysis, with the p-value for each correlation set at P < 0.05. As shown in Figure 2, the results indicate a negative correlation of serum TAC with the three categories of stress (PS, CA, and PHB). Contrarily, TBARS, cortisol, and CRP show a positive correlation with stress in all the categories. In our analyses, we observed that increased stress demonstrated a higher correlation with all biomarkers. High-stress levels show a strong negative correlation with plasma TAC levels. Specifically, a higher negative correlation was observed in CA (with −0.54, −0.65, and −0.81) as compared to PS (−0.47, −0.65, and −0.62) and PHB (−0.27, −0.41, and 0.51). We observed that an increase in serum TBARS showed a positive correlation with the three categories of stress, PS (0.34, 0.67, and 0.78), CA (0.56, 0.65, and 0.87), and PHB (0.39, 0.56, and 0.76). Similarly, cortisol was strongly positively correlated with PS (0.61, 0.69, and 0.75), CA (0.71, 0.72, and 0.83), and PHB (0.51, 0.65, and 0.65). Furthermore, CRP also showed a strong positive correlation with PS (0.59, 0.63, and 0.67) and CA (0.77, 0.81, and 0.86) and a moderate correlation with PHB (0.44, 0.45, and 0.45). Notably, no difference was observed in the correlation between CRP and the level of stress in the PHB category). We ascertain that correlation analysis demonstrated that the psychological component of well-being is connected with the four biomarkers tested in this study.
Discussion
The COVID-19 pandemic was closely associated with stress, anxiety, and depression in the population vis-à-vis the pathological outcomes of the disease.[27,28] Stress impacted almost everyone globally to varying degrees and extents.[29-31] The sudden and unprecedented changes in life due to the COVID-19 virus outbreak were overwhelming, significantly affecting the prevalence of the stress, anxiety, and health behavior among the people.[31] Hence, assessing psychological indices is imperative in restoring psychosocial and physical health stability in the post-COVID-19 era.[31,32] From the therapeutic perspective, empirical assessment of psychological measures mandates understanding biochemical parameters that can directly indicate the extent and type of stress. The current study is one of the few to address psychological variables and associated biochemical markers in the Indian population during the COVID-19 pandemic.
The results indicate the prevalence of moderate to high stress among the studied population in general and women in particular (Table 4). According to various reports from different regions of the world, similar levels of stress have been observed. Women and younger people were the most disproportionately affected, and multifactorial stress was observed to be exacerbated among women.[33] Female caregivers and women who were pregnant during this time comprise the most stressed group among the female population.[34,35] Many reports specifically demonstrate a higher PS and CA in women associated with an increased compliance with the PHB, similar to our study [Table 4]. Several studies consistently report that men’s compliance to several PHB measures is lower than females.[36,37] An important reason for this disparity may be due to the higher agreeableness and conscientious inclination of women than men, which subsequently leads to a willingness to comply more to PHB.[38]
This study provides evidence for the prevalence of stress and anxiety among the respondents (Figure 1). More than half of the adults reported having moderate to high levels of stress (57.3%) and covid-related anxiety (54.7%) in their day-to-day life while living with the COVID-19 crisis. The result is consistent with the study conducted by Verma and Mishra (2020), who reported a 25%, 28%, and 11.6% prevalence of depression, anxiety, and stress, respectively, among the Indian population during the lockdown.[29] The level was moderate to extremely severe. Similarly, Roy et al. also reported high levels of anxiety among Indians during the COVID-19 era.[39] In another study, Rehman et al. (2020) reported mild-to-moderate levels of psychological distress during the lockdown. A study by Wang et al. found severe psychological distress (anxiety, stress, and depression) during COVID-19 among Chinese nationals.[11]
PS is pivotal to the overall psychological and physical dimensions of health, contributing to physical functioning and healthcare, and a predictor of morbidity and mortality.[40,41] PS contributes to the development of considerable mental stress and well-being. We observed a negative correlation between PS and serum levels of TAC and a positive correlation with TBARS, cortisol, and CRP associated with an increase in PS (Figure 2). PS is a subjective indicator and harbors a relevance in many health conditions including cancers and has been demonstrated as a predictor of survival.[42] We can conjecture that improving health management can buffer the harmful effect of PS on psychological and physical health.
A low-to-moderate level of compliance with preventive health guidelines was observed in the present study. PHB is of utmost importance in combating the spread of the virus, and the low-to-moderate compliance observed in our study was alarming. It is, therefore, crucial to identify the key factors influencing individual compliance with the required health behavior. Understanding people’s perceptions and behavior during and after the pandemic could guide the practice of preventive health measures for current and future pandemics or similar situations. The findings of the study underscore the need to use the health belief model, as an effective framework for identifying a wide range of PHBs. The biochemical reflection of adherence to PHB varying from low to high can be observed in a decrease in the TAC (2.02± in high, and 1.22± in low) as the adherence reduced from high to low [Figure 3a]. Similarly, high adherence to PHB is associated with lower levels of TBARS and cortisol compared to moderate and low adherence to PHB [Figure 3b and c]. The results indicate a direct correlation between PHB adherence and reduction in the biochemical indicators of stress; however, combatively low changes were observed in CRP values [Figure 3d]. CRP was significantly higher in low PHB adherence than in moderate and high adherence, with no significant difference between moderate and high PHB adherence. This could be addressed based on the possibility of high exposure to stressors when low PHB was observed. Contrarily, comparatively higher levels of CRP in the high PHB adherence category may be due to psychological stress inherent in the behavior that leads a person to practice extreme caution and strictly follow PHB. Nonetheless, the COVID-19 pandemic inflicts a range of stress to intrinsically persuade stress-susceptible individuals toward high PHB practice.
The assessment of serum samples for each stress category identified low TAC concentration, which strongly correlates with psychological stress in individuals with low, moderate, or high levels [Figure 3]. This alteration is inversely proportional to the stress level, wherein an increase in stress levels is linked to a decrease in the TAC. Our results coincide with previous studies that psychological stress related to job, academic, or personal life is related to imbalances in the oxidative hemostasis, which can subsequently lead to the development of oxidative stress.[43,44] In disease conditions, an increase in pro-oxidants usually precedes immune activation and inflammation processes associated with the development of numerous diseases and disorders. Nonetheless, in the absence of any disease, an increase in oxidative stress may be directly linked to psychological stress. On the other hand, low blood TAC values have the potential to induce psychological disturbances. Studies have demonstrated a link between low dietary TAC and the subsequent development of stress, sleep disorders, depression, and anxiety. Numerous studies have shown a clear relationship between suicidal tendencies and oxidative and nitrosative stress.[45-47] Unipolar and bipolar psychiatric disease patients have been associated with the high oxidant load observed in large-scale studies.[48,49] Hence, a clear connection has been established between TAC and stress, depression, and anxiety states. Although the current researches reveal that low TAC can be a cause or an effect of stress, we conjecture that the intense stress generated due to disease spread and preventive measures during the COVID-19 pandemic, a reduction in the TAC may be an effect of stress. The reduced antioxidant potential and the generation of oxidative stress can become an initiating node for a cascade of effectors spanning metabolic, neuroinflammatory, and neuroendocrine axes. The current study also found elevated cortisol levels, normally induced as a response to stress. Studies have identified an increase in cortisol as an important biomarker for assessing the probability of onset and the severity of mental illnesses. During the pandemic phase, cortisol is of significant relevance when a general increase in the prevalence of mental symptoms was observed, associated with preventive measures and infection spread.[21] It is known that exposure to stress and perceptions of stress lead to the modulation of systemic inflammation.[50,51] Most studies have identified a correlation between diurnal cortisol slope changes and psychosocial stress, demonstrating a direct association with inflammation, that is, CRP, interleukin-6, fibrinogen, etc. In our study, we observed a distinct increase in cortisol levels in the PS category, wherein an increase is proportional to an increase in stress levels. However, low stress showed the highest cortisol levels in the CA category and comparatively lower in the moderate- and high-stress categories. This could be reflective of the allosteric load in people with significant chronic stress. Low cortisol in high-stress indicates adrenal fatigue, which can lead to chronic inflammation. As indicated by our analyses, we observe increased CRP levels in people who reported CA. The CRP is significantly increased in a low-stress group compared to moderate and high-stress groups. Long-term exposure to stress has shown prominent repercussions in the immune axis, with an increase in the risk for hypertension, diabetes, gastrointestinal disorders, and immunosuppression.[52-54] In a longitudinal cohort on women’s health, moderate and high levels of PS were identified to increase the risk for diabetes.[54,55] Our results are also supported by the outcome of animal studies demonstrating structural and functional deficits as a result of social isolation and learned helplessness.[56,57] This was directly associated with increased cortisol in animal models.[58] Studies on human and animal models indicate a direct correlation between altered functionality of the brain that reflects qualitatively in the behavior associated with depression. Our results align with the allostatic load model of psychosomatic health, wherein cortisol plays a central role in integrating stress exposure to PS and anxiety with immune functioning.[59-61]
Conclusion
The findings of the present study indicate the prevalence of moderate to high stress and anxiety among literate Indian adults during the COVID-19 pandemic. Corroborated with the biochemical markers, namely, TAC, TBARS, cortisol, and CRP, the study affirms the presence of stress in the study population. The results emphasize the need for special attention should be given to the mental and physical health problems of the population in general and women in particular, as they are more susceptible to stress and anxiety. The adherence to COVID-19 PHB was found to be poor to moderate among the people. Comparatively, a limited proportion of people strictly follow the COVID-19 preventive guidelines. Given the vital role of PHBs in reducing the spread of diseases, there is a need to enforce preventive health measures in public and take necessary steps for compliance. Furthermore, the presence of chronic psychological stress influenced an increase in the levels of serum TBARS, the marker of lipid peroxidation, cortisol, and CRP levels, and the overall antioxidant capacity. Hence, a decrease is observed in the serum TAC. It is therefore evident that long-term stress, as observed in the COVID-19 pandemic times, could subsequently alter oxidative homeostasis by its effect on neuroinflammatory, neuroendocrine, and metabolic junctions, affecting the overall immune functioning of an individual. The general COVID-19-associated anxiety demonstrates a high score in our study. This study underlines the importance of biochemical indices and psychological measures synergistically enhancing the health-care ability to prognosticate stress levels in the population specifically. Despite its limitations, this research significantly contributes to the current global stress management need. The government and other agencies can use it to tackle the adverse psychological effects of COVID-19-related stressors among literate Indian adults.
Ethics Approval and Consent to Participate
The authors certify that the participant recruitment in the study was solely voluntary and was in accordance with the guidelines of the Biomedical Ethics Committee of the Era’s, Lucknow Medical College and Hospital. Participation, filling questionnaire, sampling, and experimentation were performed according to the guidelines of the Biomedical Ethics Research Committee (Reference No. ELMC & H/20 21R-cell/178) of Era’s Lucknow Medical College and Hospital. Jointly, the authors approved the publication of this manuscript.
Availability of Data and Material
The data supporting the findings of this study are available in the article. More detailed data used to support the findings of the current study are available from the corresponding author on reasonable request.
Competing Interests
All the authors declared that there was no conflict and/or competing interests.
Funding Statement
The authors extend their appreciation to the Deputyship of Research and Innovation, Ministry of Education in Saudi Arabia for funding this research through project number 223202.
Authors’ Contributions
Yusuf Saleem Khan; investigation, conceptualization, data curation, formal analysis, methodology. Abdullah Alsrhani; investigation, methodology, and project administration. Salma Kaneez; investigation, conceptualization, writing, reviewing, and proofreading. Mahvish Fatima; conceptualization, formal analysis, methodology, validation, and writing the original draft. Khalid Iqbal; investigation, methodology, and resources. Muharib Alruwaili; Investigation, methodology, proofreading. Aisha Farhana; conceptualization, formal analysis, writing original draft, project administration. All authors have read and agreed to the published version of the manuscript.
Acknowledgment
We would like to thank the participants of the study, and hospital staff for their help in sampling and completion of this work.
References
- COVID-19 mental health impact and responses in low-income and middle-income countries:Reimagining global mental health. Lancet Psychiatry. 2021;8:535-50.
- [Google Scholar]
- The use of telepsychiatry during COVID-19 and beyond. Ir J Psychol Med. 2020;37:250-5.
- [Google Scholar]
- 2023. Number of COVID-19 cases reported to WHO, India. Available from: https://data.who.int/dashboards/covid19/cases?m49=356&n=c
- Impact of COVID-19 in the mental health in elderly:Psychological and biological updates. Mol Neurobiol. 2021;58:1905-16.
- [Google Scholar]
- A systematic review and meta-analysis of symptoms of anxiety, depression, and insomnia in Spain in the COVID-19 crisis. Int J Environ Res Public Health. 2022;19:1018.
- [Google Scholar]
- Prevalence of depressive and anxiety symptoms among Chinese older adults during the COVID-19 pandemic:A systematic review and meta-analysis. J Geriatr Psychiatry Neurol. 2022;35:182-95.
- [Google Scholar]
- Depression and anxiety during the COVID-19 pandemic:Epidemiology, mechanism, and treatment. Neurosci Bull. 2023;39:675-84.
- [Google Scholar]
- Psychiatry of Pandemics:A Mental Health Response to Infection Outbreak. Germany: Springer; 2019.
- The impacts of a COVID-19 epidemic focus and general belief in a just world on individual emotions. Personal Individ Dif. 2021;168:110349.
- [Google Scholar]
- Depression, anxiety and stress among Indians in times of Covid-19 lockdown. Community Ment Health J. 2021;57:42-8.
- [Google Scholar]
- The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. 2020;87:49-50.
- [Google Scholar]
- Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228-9.
- [Google Scholar]
- Perceived psychological stress and associated factors in the early stages of the coronavirus disease 2019 (COVID-19) epidemic:Evidence from the general Chinese population. PLoS One. 2020;15:e0243605.
- [Google Scholar]
- Oxidative stress:A potential link between emotional wellbeing and immune response. Curr Opin Pharmacol. 2016;29:70-6.
- [Google Scholar]
- Association of dietary total antioxidant capacity with depression, anxiety, and sleep disorders:A systematic review of observational studies. J Clin Transl Res. 2021;7:631-40.
- [Google Scholar]
- Does inflammation link stress to poor COVID-19 outcome? Stress Health. 2021;37:401-14.
- [Google Scholar]
- Oxidative stress and inflammatory biomarkers for the prediction of severity and ICU admission in unselected patients hospitalized with COVID-19. Int J Mol Sci. 2021;22:7462.
- [Google Scholar]
- Stress, the cortisol awakening response and cognitive function. Int Rev Neurobiol. 2020;150:187-217.
- [Google Scholar]
- Measuring stress:A review of the current cortisol and dehydroepiandrosterone (DHEA) measurement techniques and considerations for the future of mental health monitoring. Stress 2023. ;26:29-42.
- [Google Scholar]
- Perceived stress scale. In: In:Measuring Stress:A Guide for Health and Social Scientists. Vol 10. United Kingdom: Oxford University Press; 1994. p. :1-2.
- [Google Scholar]
- SARS risk perception, knowledge, precautions, and information sources, the Netherlands. Emerg Infect Dis. 2004;10:1486.
- [Google Scholar]
- An overview of generic health-related quality of life measures for HIV research. In: Qual Life Res. Vol 1. 1992. p. :91-7. (b) Steward AL, Sherbourne CD, Ware JE, Hayes RD, Wells KB, Berry SH, et al. Summary and Discussion of MOS Measures. In: Stewart AL, Ware JE, editors. Measuring Functioning and Well-Being: The Medical Outcome Study Approach. Durham, NC: Duke University Press; 1992. p. 345-71.
- [Google Scholar]
- Ferric reducing capacity versus ferric reducing antioxidant power for measuring total antioxidant capacity. Lab Med. 2013;44:51-5.
- [Google Scholar]
- Prevalence of depression, anxiety, and stress during COVID-19 pandemic. J Neurosci Rural Pract. 2020;11:519-25.
- [Google Scholar]
- Anxiety, depression and stress during the COVID-19 pandemic:Results from a cross-sectional survey. J Psychiatr Res. 2021;137:96-103.
- [Google Scholar]
- Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int J Soc Psychiatry. 2020;66:756-62.
- [Google Scholar]
- Exposure to COVID-19 pandemic stress:Associations with depression and anxiety in emerging adults in the United States. Depress Anxiety. 2020;37:1280-8.
- [Google Scholar]
- Who is the most stressed during the COVID-19 pandemic?Data from 26 countries and areas. Appl Psychol Health Well Being. 2020;12:946-66.
- [Google Scholar]
- Personality and perceived stress during COVID-19 pandemic:Testing the mediating role of perceived threat and efficacy. Pers Individ Dif. 2021;168:110351.
- [Google Scholar]
- Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic:A review. Soc Sci Med. 2020;266:113364.
- [Google Scholar]
- Vulnerability and resilience to pandemic-related stress among US women pregnant at the start of the COVID-19 pandemic. Soc Sci Med. 2020;266:113348.
- [Google Scholar]
- Stress and anxiety levels in pregnant and post-partum women during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:9450.
- [Google Scholar]
- Gender differences in COVID-19 attitudes and behavior:Panel evidence from eight countries. Proc Natl Acad Sci. 2020;117:27285-91.
- [Google Scholar]
- Gender differences in fear and risk perception during the COVID-19 pandemic. Front Psychol. 2021;12:689467.
- [Google Scholar]
- Pandemic prevention and personality psychology:Gender differences in preventive health behaviors during COVID-19 and the roles of agreeableness and conscientiousness. J Saf Sci Resilience. 2022;3:87-91.
- [Google Scholar]
- Study of knowledge, attitude, anxiety and perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatry. 2020;51:102083.
- [Google Scholar]
- Health perceptions and survival:Do global evaluations of health status really predict mortality? J Gerontol. 1991;46:S55-65.
- [Google Scholar]
- Association between perceived health and adherence to treatment after percutaneous coronary intervention:A long-term follow-up study. J Adv Nurs. 2022;78:1653-64.
- [Google Scholar]
- Predicting the survival of patients with cancer from their initial oncology consultation document using natural language processing. JAMA Network Open. 2023;6:e230813.
- [Google Scholar]
- The association of major depressive disorder with activation of NLRP3 inflammasome, lipid peroxidation, and total antioxidant capacity. J Mol Neurosci. 2020;70:65-70.
- [Google Scholar]
- Investigating the relationship between job stress, workload and oxidative stress in nurses. Int J Occup Saf Ergon. 2022;28:1176-82.
- [Google Scholar]
- The relationship between suicide and oxidative stress in a group of psychiatric inpatients. J Clin Med. 2020;9:3462.
- [Google Scholar]
- Inflammation and nitro-oxidative stress in current suicidal attempts and current suicidal ideation:A systematic review and meta-analysis. Mol Psychiatry. 2022;27:1350-61.
- [Google Scholar]
- Potential inflammatory biomarkers for major depressive disorder related to suicidal behaviors:A systematic review. Int J Mol Sci. 2023;24:13907.
- [Google Scholar]
- Oxidative stress parameters and antioxidants in patients with bipolar disorder:Results from a meta-analysis comparing patients, including stratification by polarity and euthymic status, with healthy controls. Bipolar Disord. 2021;23:117-29.
- [Google Scholar]
- Systemic inflammation and oxidative stress markers in patients with unipolar and bipolar depression:A large-scale study. J Affect Disord. 2024;346:154-66.
- [Google Scholar]
- Perceived stress is linked to heightened biomarkers of inflammation via diurnal cortisol in a national sample of adults. Brain Behav Immun. 2021;93:206-13.
- [Google Scholar]
- Diagnosis and stratification of COVID-19 infections using differential plasma levels of D-dimer:A two-center study from Saudi Arabia. Microbiol Res. 2023;14:67-76.
- [Google Scholar]
- Prevalence of PTSD and common mental disorders amongst ambulance personnel:A systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2018;53:897-909.
- [Google Scholar]
- Biomarkers in stress related diseases/disorders:Diagnostic, prognostic, and therapeutic values. Front Mol Biosci. 2019;6:91.
- [Google Scholar]
- How exposure to chronic stress contributes to the development of type 2 diabetes:A complexity science approach. Front Neuroendocrinol. 2022;65:100972.
- [Google Scholar]
- Stress increases the risk of type 2 diabetes onset in women:A 12-year longitudinal study using causal modelling. PLoS One. 2017;12:e0172126.
- [Google Scholar]
- Animal models of major depression:Drawbacks and challenges. J Neural Transm (Vienna). 2019;126:1383-408.
- [Google Scholar]
- Animal models of depression:What can they teach us about the human disease? Diagnostics (Basel). 2021;11:123.
- [Google Scholar]
- Cortisol and major depressive disorder-translating findings from humans to animal models and back. Front Psychiatry. 2020;10:974.
- [Google Scholar]
- A clinical allostatic load index is associated with burnout symptoms and hypocortisolemic profiles in healthy workers. Psychoneuroendocrinology. 2011;36:797-805.
- [Google Scholar]
- Allostatic load and its impact on health:A systematic review. Psychother Psychosom. 2020;90:11-27.
- [Google Scholar]







