Translate this page into:
The performance of physiotherapeutic conducts in oncology patients interned in a pediatric intensive care unit: A systematic review
Address for correspondence: Suellen Cristina Roussenq, Physiotherapist and Master’s Degree of Science in Human Movement, State University of Santa Catarina, Center of Health and Sport Sciences, Florianópolis, Brazil. Phone: +55 48 996731731. E-mail: suca_sc@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The intervention of physical therapy in pediatric oncology is currently transmuting from a view based on the restriction of physical stress to an approach that advocates the practice of cardiorespiratory and motor interventions that provide a better prognosis for the patient. The objective of this study is to carry out a systematic review and to identify studies that address the performance of physical therapeutic practices in pediatric cancer patients admitted to an intensive care unit (ICU).
Methods:
The stage of identification and selection of articles were carried out according to what was recommended by Preferred Reporting Items for Systematic Review and Meta-analyzes, on PubMed, Medline, and Scopus platforms, based on the PICO acronym, and were classified by the PeDRO quality scale.
Results:
A total of 19,820 articles were found and six were acceptable according to the inclusion and exclusion criteria of the study, accounting for a total of 634 patients evaluated in the respective study.
Conclusion:
There is a scarcity of studies that show the reality of physical therapy practice in pediatric and neonatal ICU, with a focus on cancer patients. Most of the articles found emphasize the physiotherapeutic approach in the management of ventilation in these patients. Within this context, they show positive outcomes with the highest number of discharges, reduced mortality, increased survival, and treatment of respiratory failure. In addition, the application of non-invasive ventilation modalities proved to be more prevalent and important, both in the variables mentioned above and in the prevention of complications, such as a lower rate of patients undergoing orotracheal intubation.
Keywords
Cancer
oncology
pediatric intensive care unit
pediatric
physical therapy
rehabilitation
Introduction
Pediatric cancer in Brazil is responsible for 2–3% of all types of cancer registered.[1] It manifests itself in a chronic form with a higher mortality rate in the age group from 0 to 19 years and it’s estimated that for the year 2020, there will be 8.460 new cases of cancer in the pediatric population.[1]
In developed countries, 5-year survival rates exceed 80% for the 45,000 children, whereas in the underdeveloped countries, these rates are below 30% for the 384,000 patients. The differences in survival rates, in these different contexts, are justified by the type of care for patients living in high-income countries.[2] The global survival goal recently set by the World Health Organization is that there will be 60% survival for all children with cancer by 2030, since each year, about 429,000 children and adolescents aged 0–19 develop cancer worldwide.[1]
Improved mortality rates in pediatric intensive care can come at the cost of increased morbidity. The objectives of the modern pediatric intensive care unit (PICU) should focus on restoring the long-term function of survivors of chronic pediatric disease.[3] With that said, mortality rates in the PICU of patients with pediatric cancer are also much higher when compared to the current mortality rates of the general population of the PICU. This is because, in advanced cancer therapy, intensified multidisciplinary treatment protocols, advanced stratification, and support were initiated.[4] Within this context, multidisciplinary research shows that treatment for children in low- and middle-income countries can be improved with more effective therapies to local resources and clinical needs.[1] Likewise, rehabilitation specialists are also an integral part in the neonatal ICU (NICU) team. New approaches to the practice of rehabilitation at the NICU have evolved in the last decade, with the aim of promoting child health and development.[5]
With regard to physical therapy in pediatric oncology, it is currently transmuting from a scientific view based on the restriction of physical stress to an approach that advocates the practice of motor activities that provide a better prognosis for the patient being treated.[6] This is mainly related to the reduction of osteo-neuro-muscular and cardiorespiratory repercussions, when comparing the practice of targeted exercises and immobilization.
A review conducted by Braam et al. (2016) analyzed trials of intervention programs that included at least one home exercise program guided by a therapist at the treating clinic to optimize physical fitness. Results showed more improvements in outcomes in the intervention group than in the control group. Specifically, when assessing outcomes such as cardiorespiratory adaptation, body composition, flexibility, muscle strength.[7] In addition, other studies show that therapeutic exercises show benefits for managing the side effects of cancer treatment in general, increasing tolerance, and improving functional results for this population.[8]
Likewise, in the approach of chest physiotherapy, the preference for less invasive modalities (NIV) in choosing the ventilatory treatment has guaranteed pediatric oncology patients a lower rate of pneumonia. When it comes to positive pressure ventilation (PPV), a protective strategy for the lungs, the use of low volumes, permissive hypercapnia, adequate positioning, conservative fluid control, and new conventional ventilation modes present better results in most ICUs that provide care to cancer patients.[9]
Considering the above mentioned, the objective of this study is to identify, evaluate, and summarize the results of all individual studies that address the performance of physical therapy practices in pediatric cancer patients admitted to an ICU, making this evidence more available and accessible to the clinical practice of these professionals and others who are part of the multidisciplinary team.
Methods
Identification and selection of articles
This systematic review followed the recommendations of Preferred Reporting Items for Systematic Review and Meta-analyzes. Complete, observational cohort, cross-sectional, and case–control articles were included, investigating the topic of physiotherapy in the ICU, oncology and pediatrics, regardless of whether it was evaluated as an exposure or outcome variable. The age group considered was from 0 to 19 years. The articles were published in Portuguese, English, or Spanish.
Selection/eligibility
The following inclusion criteria were established: (1) Studies limited to humans of any study of ethnic origin and gender, (2) texts written in Portuguese, Spanish, and English, (3) experimental studies, (4) sample composed of humans aged from 0 to 18 years old may vary according to hospital institutions, and (5) related to the treatment or physical therapy evaluation in pediatric cancer patients in the ICU.
As for exclusion criteria: (1) Dissertations, (2) theses, (3) studies with an emphasis on diseases other than childhood cancer, and (4) studies that bring pediatric patients over 18 years old were excluded from the study.
Search strategy
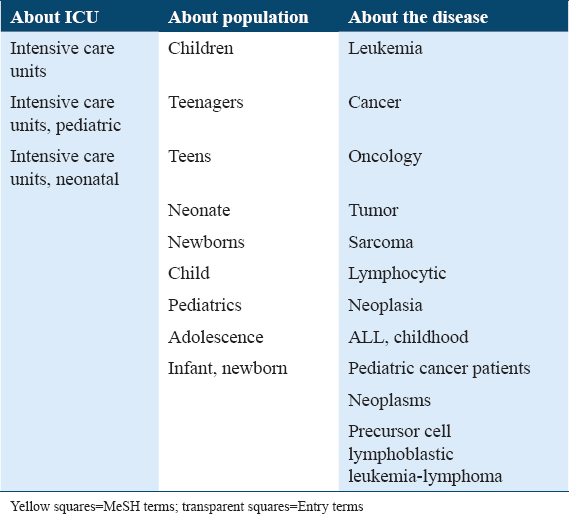
Electronic searches were used in the Scopus, Medline, and PubMed databases. Electronic searches were performed in the databases Scopus, Medline, and PubMed using the controlled descriptors MeSH Terms/MeSH Heading and the corresponding search terms, and the descriptors of the health sciences (DeCS). The terms chosen were in accordance with the study and were divided into three blocks, the first block was about the study site, according to population and the third diagnosis [Table 1]. Boolean operators were used between terms and between blocks. The search was carried out in June 2017 and updated in September 2019.
Selection of studies and data extraction
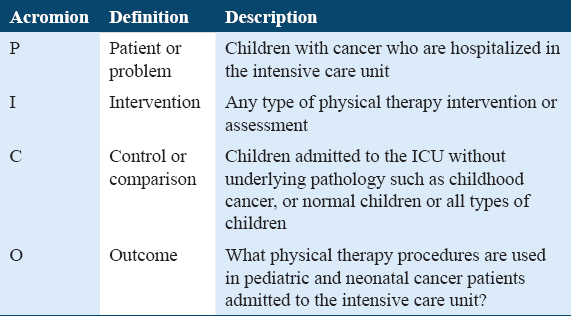
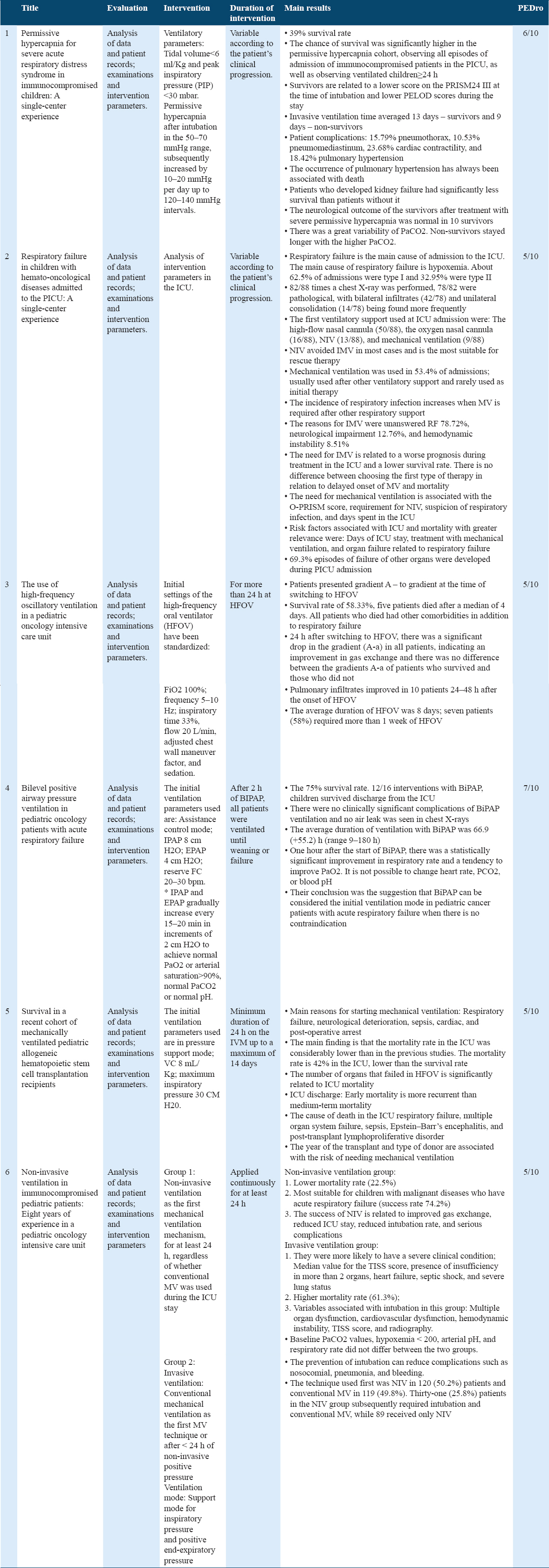
For the selection and extraction of articles, the researchers used the acronym Population, Intervention, Comparators, Outcomes, and Study [Table 2]. The search was carried out by a main researcher and two independent reviewers, who searched and analyzed all potentially relevant articles. The work followed the sequence of reading titles and abstracts. After the first selection, the full articles were read, excluding those that did not meet the inclusion and exclusion criteria. In cases where there was no consensus, a fourth evaluator was consulted to decide on the study’s eligibility [Figure 1].
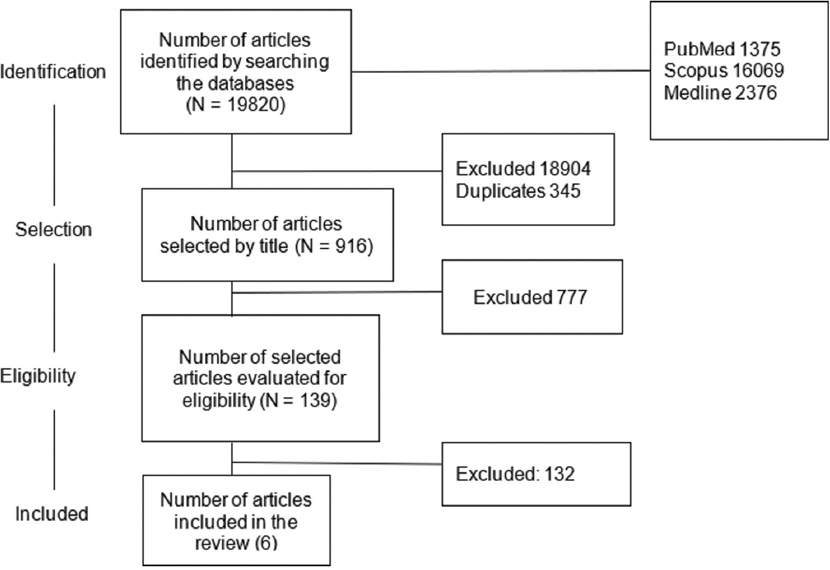
- Flowchart of studies included in the systematic review. Legend: Articles that did not talk about cancer patients, patients who were not in the intensive care unit, patients who were not pediatrics, or even those that did not talk about measures performed by the physiotherapy team were excluded
The articles were accessed in full by the online search platforms. For those who were not available, a formal request was made through email to the authors. Studies with a focus on other diseases were excluded with the exception of childhood cancer, and studies that did not use any physiotherapeutic approaches. A search time limit was not established since the study wanted to make a timeline of studies on the topic.
Methodological Evaluation
The PEDro[10] scale was used to assess the quality of the studies included in this systematic review, the score being extracted from the PEDro database.
This scale was elaborated based on the Delphi scale of Verhagen and collaborators, where it is divided into 11 items, from items 2 to 11 being computed for a final score from 0 to 10. External validity (item 11), on the other hand, analyzes the capacity of the study to be generalized to the population or not, however, this item is not calculated in the final score.
Results
Selection of studies
There were 19,820 articles initially identified. Subsequently, the title screening phase and the exclusion of duplicate studies (in a total of 345 articles) were carried out, afterward, the abstracts screening phase was completed and, finally, full reading of the articles. In all, 19,681 articles were excluded, reaching the final number of six articles to include in this SR [Figure 1].
Quality analysis of articles
As for the scores obtained, the articles obtained a score between 5 and 7 out of 10. As recommended by Moseley et al.,[11] studies are of good methodological quality if they obtain five or more points.
The “Results of physical therapy procedures in the neonatal and pediatric ICU”, it is necessary to join with the paragraph in front to show that it is a subtitle, increase the letter and leave it in bold according to the others.
Analyzing the results obtained by the search strategies, studies published between 2008 and 2017 were observed, with no publications meeting the criteria from 2017 onward. All the analyzed articles are retrospective cohort studies. The methodological data of the articles are shown in Table 3 and summary of the interventions found in Table 4.
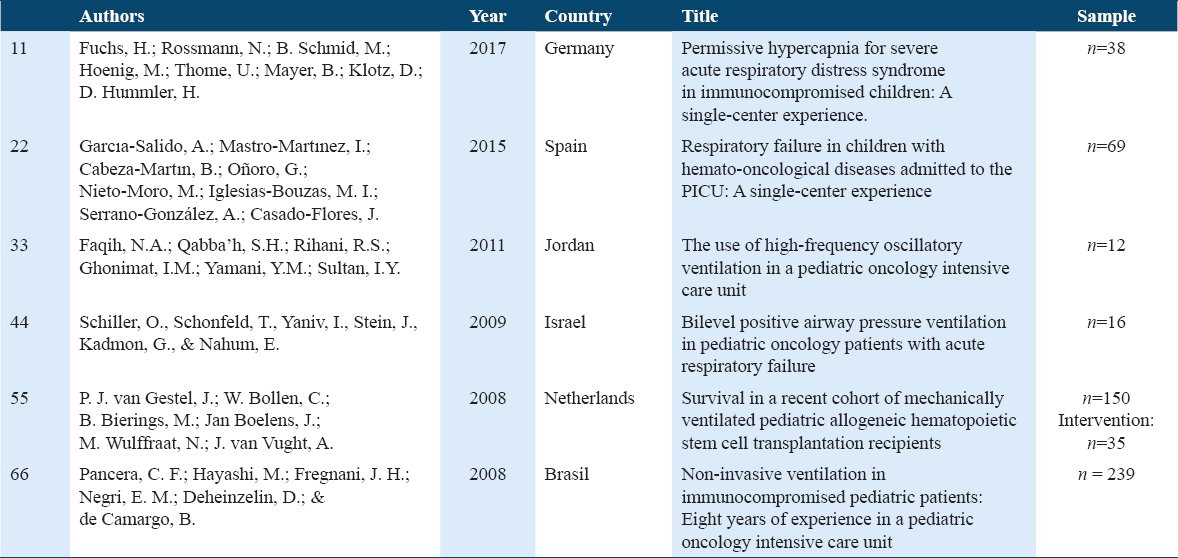
The studies used a sample of 12–150 subjects, with the exception of the research by Pancera et al. (2008),[12] which used a sample with 239 participants.[13-17] The age group remained between 0.4 and 22 years in the total of 409 individuals investigated in the studies.[12,14-17]
As for the most recurrent primary diagnoses of cancer in this population, they were acute lymphoid leukemia, solid tumor, and acute myeloid leukemia, the most common deficiency being immunodeficiency.[12-14,16] Garcia-Salido et al. (2015)[13] and Schiller et al. (2009)[14] showed the consistency of bone marrow transplantation before admission to the ICU.[13,14]
In addition, regarding the diagnosis, the study data were also observed. The radiographic findings in the chest X-rays were found in five of six articles included in the study, bringing bilateral infiltrates, lobar consolidation or unilateral lobar mass, pleural effusion as the most found, pulmonary congestion, atelectasis, and pneumothorax were the most common radiological findings in routine hospital examinations.[12,13,15,16]
All studies involved mechanical ventilation as the main physiotherapeutic approach.[13-17] Bearing in mind that half of the studies analyzed types of ventilatory support and benefits of permissive hypercapnia in respiratory failure.[13-15]
Of these, three studies mentioned that the main reason for starting ventilatory support in the ICU is respiratory failure due to hypoxemia.[13,14,16] Other reasons would be neurological deterioration, sepsis, cardiac arrest, post-operative, respiratory distress, respiratory failure due to hypercapnia, and other serious respiratory events.
Regarding the duration of ventilatory support, Garcia-Salido et al. (2015)[13] observed a stay of 2.5–12.2 days[13] and Fuchs et al. (2017)[15] an average of 13 days for surviving patients and 9 days for non-surviving patients.[15] Regarding the parameters, Faqih et al. (2011)[16] found an average of 8 days on high-frequency oral ventilation (HFOV) and 2 days on VMC before switching to HFOV in their study.[16] Schiller et al. (2009)[14] noted the average duration of 66.9 h on ventilation with BIPAP.[14]
The outcome of arterial carbon dioxide pressure (PaCO2) was observed by Pancera et al. (2008),[12] in which his study found that there was no significant difference in PaCO2 between invasive and non-invasive ventilation in immunocompromised children.[12] Fuchs et al. (2017)[15] when observing permissive hypercapnia (PaO2 >60 mmHg) in patients with acute respiratory distress syndrome (ARDS) determined that the interval desired by the clinical team was 120–140 mmHg where the largest number of surviving patients remained.[15] In this study, the neurological outcome of the survivors after treatment for permissive hypercapnia was normal in 10 survivors, mild learning difficulties were found in two patients, and three had moderate or severe mental impairment.[15]
Regarding the mortality and survival of patients in the pediatric and NICU, Fuchs et al. (2017)[15] stated a significantly longer survival in the permissive court of hypercapnia. Survival is related to a lower score on the PRISM24 III at the time of intubation and lower PELOD scores during the stay.[15] In this study, mortality has always been associated with pulmonary hypertension.[15] Van Gestel et al. (2008)[17] claimed that the mortality rate (42%) in the ICU after bone marrow transplantation is lower than that of survival, as the cause of death is respiratory failure, multiple organ failure, sepsis, Epstein’s encephalitis Barr, and post-transplant lymphoproliferative disease.[17] The number of organs that failed during IMV and HFOV are significantly related to ICU mortality.[17] Faqih et al. (2012)[16] also analyzed HFOV, where he states that the gradient (A-a) is an important predictor of survival, where patients who survived had a lower gradient (A-a) after switching to HFOV than those who died.[16] Five patients died after the median of 4 days (2–33 days), they had other comorbidities in addition to respiratory failure at the time of switching ventilation to HFOV.[16] Two of the five patients who died received an allogeneic hematopoietic stem cell transplant.[16] The seven surviving patients were weaned from HFOV after a median of 9 days (range between 3 and 40 days) and placed on IMV for a median of 10 days (4–21 days). They were discharged from the ICU to the floor, without the need for oxygen.[16]
Schiller et al. (2009)[14] reported that non-invasive ventilation (NIV) is the most indicated in the intervention of children with malignant disease and acute respiratory insufficiency (ARI) due to the high survival rate (80%). The results are consistent with those reported in the medical literature for invasive mechanical ventilation.[13] The success of non-invasive mechanical ventilation (NIV) is related to improved gas exchange, reduced ICU stay, reduced intubation rate, and serious complications.[13]
In line with this result, Pancera et al. (2008)[12] stated that the highest mortality rate (61.3%) is in invasive mechanical ventilation when compared to non-invasive mechanical ventilation. As well as, Garcia-Salido et al. (2015)[13] who stated that mechanical ventilation is related to the worst prognosis during treatment in the ICU and the lowest survival rate.[13] The risks associated with ICU and mortality with greater relevance in this study are days in the ICU, treatment with mechanical ventilation, and organ failure related to respiratory failure.[13]
In the same study, Garcia-Salido et al. (2015)[13] find results on organ failure, showing that 69.3% of them were developed during admission to the ICU. Moreover, Pancera et al. (2008)[12] stated that failure in more than 2 organs is related to the greater probability of severe clinical condition in the group of invasive mechanical ventilation, together with the TISS score, heart failure, septic shock, and pulmonary status severe (chest X-ray with more than 2 findings).[12]
Discussion
In this analysis, all the studies found on the physical therapy performance, in the treatment of pediatric cancer patients admitted to the ICU, are related to the ventilatory management of these patients. Within this context, the finding of a reduction in the mortality rate of these individuals stands out, when respiratory support is accompanied by physical therapists.[12-15] Regarding the causes of mortality and complications, a 4-year review of cancer patients admitted to the pediatric ICU by Barking et al., 2020,[18] made the assessment of prognostic factors that can correlate with the results mentioned above.
Regarding the survival of pediatric oncology patients, we can relate that in children and adolescents, the neoplasm usually affects the cells of the blood system and supporting tissues. Tumors in childhood cancers grow faster than those in adults and become invasive, but respond better to treatment. However, it is important that parents and family members know how to identify the signs and symptoms of the disease, which are very similar to those of common childhood diseases. This is a confounding factor in cancer diagnosis, leading to late diagnosis and decreasing the child’s chances of survival.
It is known, however, that several factors can interfere in the probabilities of survival from childhood cancer, this factor has been attributed to a possible delay in the establishment of the diagnosis and beginning of the treatment of this child. The delay in seeking medical care, in turn, may be due to several variables of a socioeconomic nature, such as lower access to health services, cultural barriers that make it difficult to perceive the possibility of curing cancer, and even language barriers.
We can cite several complications and diseases faced by pediatric cancer patients admitted to the ICU, such as: (1) Sepsis or septic shock, due to immunological weakness; (2) hemodynamic instability, due to cardiotoxicity or sepsis; (3) arrhythmias or cardiorespiratory arrest, caused by severe hydroelectrolytic and metabolic disorders; (4) seizures, generated by drug toxicity, CNS tumor infiltration, or metabolic disturbances; (5) apnea, due to hemorrhage, ICH, cerebrospinal fluid infiltration, and brainstem tumors; (6) neurological symptoms, due to spinal cord compression, CNS tumor, or stroke; (7) renal failure, caused by nephrotoxicity, sepsis, infiltration, compartment syndrome, and abdominal masses (hypoperfusion); (8) intestinal obstruction, by compression; (9) upper mediastinal syndrome; (10) leukostasis; (11) spontaneous tumor lysis syndrome; and (12) pre- and post-operative tumor resection surgeries.
Respiratory rehabilitation aims to improve ventilation patterns, in addition to providing comfort and ease in the global work of breathing. In some more severe cases, when there is a need for oxygen therapy, artificial airway, non-invasive ventilation or invasive ventilation, and the patient is bedridden, clearing maneuvers are necessary to also favor airway permeability and/or airway clearance. Mediastinal masses, febrile neutropenia (allowing infections), bacterial infections (viral and fungal), infections by contiguity, and pulmonary metastases can be reported as causes of pulmonary complications. Therefore, in these cases, the physical therapist recommends: (1) Helping the maintenance of vital functions through the prevention and control of pulmonary diseases; (2) reduce the complications of the underlying disease itself; (3) promoting the preservation of pulmonary oxygenation and ventilation; (4) keep the airways clear and patent; (5) decreased work of breathing; (6) respiratory muscle training; (7) patient-ventilator synchronization; and (8) pulmonary rehabilitation.
As a result of the immobility in bed, due to the treatment, these patients have a decrease in the movement of the costovertebral, costochondral, and diaphragmatic joints, leading to a decrease in vital capacity and functional residual capacity and, finally, a decrease in the ability to expectorate, which may lead to atelectasis and pneumonia. Due to the aforementioned, the physiotherapeutic respiratory treatment focuses on: (1) Prevention of respiratory complications (dyspnea and atelectasis, among others); (2) bronchial clearance; (3) pulmonary re-expansion; (4) assessment of work of breathing; (5) respiratory muscle training; (6) use of non-invasive ventilation when necessary; and (7) support and wean from invasive ventilation when needed.
It is necessary to remember that it is extremely important to choose the correct technique for the proposed objective, taking into account the patient’s age, level of understanding and collaboration, and respecting the patient’s limits, complaints, and moments of indisposition. Due to the risk of bleeding, it is necessary to assess this patient’s platelet levels before treating him. In patients with an artificial airway, care should always be maintained, evaluating the need for aspiration and its risk-benefit to the patient.
In our study, we also found a comparison between the use of NIV and IMV, identifying a correlation between the reduction in the mortality rate in patients who used NIV.[12,14-16] Inclusive, according to García-Salido et al. (2015), the majority of patients who used NIV did not need IMV, demonstrating, therefore, the prevention of orotracheal intubation (OTI) and consequently complications associated with this invasive procedure, also reducing the length of ICU stay.[13] In addition, the success of NIV is related to the improvement of gas exchange and the reduction of serious complications.[12]
Another important aspect found in one of the studies in this review is that NIV fits as the best measure for rescue protocols in respiratory failure.[16] It is relevant to observe the increase in the number of discharges and greater survival of childhood cancer patients with acute respiratory failure attended by physiotherapy.[12,14-16] In one of the studies that analyzed PPV modalities, it was observed that 1 h after the beginning of BiPAP, there was a statistically significant improvement in respiratory rate and a tendency to improve PaO2.[14] In this same study, BiPAP proved to be difficult to implement for children under 3 years of age, due to the cooperation with the placement and secretion of masks. There were no clinically significant complications of BiPAP ventilation and no air leaks were observed in the chest X-rays.[14]
According to the before mentioned, a 2017 multicenter study reviewed data from 1004 patients of patients with neoplasms, affected by ARI, where NIV was used even for the most severe patients, in 387 of the sample, and there was failure in 71% of cases, therefore associated with mortality. In view of this, some factors such as ARDS related to lung infection were associated with NIV failure.[19]
However, in this context of severity, a risk factor related to ARI is organ failure, which is proportional to the days of ICU stay and prolonged use of IMV.[16] Corroborating this finding, a retrospective study of 2015, analyzed cases of children affected by hematological cancer with ARI admitted to the ICU and showed a relationship between organ failure, mortality, and use of HFOV[13] In contrast, in this study, it was seen that HFOV was successful in saving patients with high risk of mortality, including children who underwent allogeneic BMT.[13] In addition, the transition to HFOV, within 2 days after the onset of IMV, resulted in a 76% decrease in the chances of death compared to those who made the transition to HFOV subsequently NIV, similar to the finding in one of the researches found in the review.[13]
The effectiveness of HFOV in the treatment of hematological cancer in children with ARDS is also questioned in the literature. A study with pediatric allogeneic BMT patients who had ARI, requiring IMV for severe pediatric ARDS, found that early use of HFOV was associated with improved survival compared to late implementation of HFOV. Therefore, when dealing with the pediatric population submitted to BMT with ARDS, IMV has a significant difference in the prognosis and mortality of these patients. Moreover, the year of the transplant and type of donor are associated with the risk of the need for IMV.[12]
In line with the above, it is important to highlight the possibility of a difference in relation to the type of cancer treated in the ICU and its management. Immunodeficiency is a pre-existing condition for several complications, the most serious of which is septicemia and organ failure. Thus, it consequently becomes a risk factor for ARDS mortality. Research shows that the time of invasive mechanical ventilation, the length of stay in the PICU, and mortality increased as the severity of ARDS in children worsened.[19] In addition, ALL and acute myeloblastic leukemia are among the most recurrent primary diagnoses in this population, both report the precedence of BMT before ICU admission.
The risks associated with ICU and mortality with greater relevance in this study are days of ICU stay, treatment with IMV, and organ failure related to ARI.[13] Another consequence noted in studies of IMV use in ARI is cardiovascular dysfunction and hemodynamic instability.[14] The hemodynamic changes are closely related to the ongoing risk of septicemia and septic shock. Another factor is that patients who developed kidney failure had significantly less survival than those without previous kidney failure.[15]
Another issue addressed by the studies found is the use of permissive hypercapnia, as there are still insufficient clinical data for which levels of PCO2 can be safely allowed and there are no data available if this strategy translates into a survival benefit.[20] Despite this, the current guidelines recommend the concept of ventilation with low tidal volume and permissive hypercapnia for patients with sepsis, ARDS, or acute with chronic respiratory failure, which we call protective ventilation and tolerating an increase in PCO2 beyond the limits established by the literature.[20]
However, only one of the studies analyzed in this work, has a lower mortality rate, associated with the use of the permissive hypercapnia technique.[15] A historical cohort showed that the use of this strategy increased the survival rate of immunocompromised children who required mechanical ventilation for more than 24 hours from 32% to 48%.[15]
Among the studies included in this review, we found some limitations, such as the timeliness of the studies, being temporarily limited until the year 2017, demonstrating that there are few publications within the criteria of this study in recent years. In addition, all studies found in this review are in the retrospective category, bringing the harm of information bias and the inability to control confounding variables such as lack of information, showing the need for more prospective studies.
Furthermore, there was also a literary range on hematological cancer, which may be because it is the cancer with the greatest complications due to its treatment and is the most common in this population, however, there is a need for studies with other types of cancer such as of central nervous system and solid tumors. In the same context, there is a need for more research that brings a better methodological quality, with a more significant sample and that considers the specificity of physical therapy treatment in this population within the ICU.
Few studies have been found with cancer patients and, mainly, of those pediatric patients in an ICU. Therefore, this research suggests that further studies are carried out in this area to better cover the care of these patients, being more effective and bringing better literary evidence.
Conclusion
When comparing the effectiveness of approaches in the ventilatory management of pediatric cancer patients admitted to the ICU, it is understood that the use of NIV and the prevention of OTI are important factors that contribute to the prevention of complications, which can lead to better survival. Therefore, in cases of mild-to-moderate respiratory failure, NIV should be prioritized as a fundamental tool. However, in clinical cases of severe respiratory failure and ARDS, the use of early IMV allows for a better prognosis and less mortality. This is also related to the type of cancer and the immunological aggressiveness of the treatment to which they are submitted. In this case, the physiotherapeutic performance in the follow-up of the clinical picture and constant ventilatory management of these patients is essential in view of the prevention of complications, reduction of mortality/longer survival, and better prognosis.
Authors’ Declaration Statements
Ethics approval and consent to participate
This study does not need an ethics committee.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding statement
No funding was received to produce this paper.
Authors’ Contributions
All authors contributed to the study conception and design. Material preparation, data collection, analysis, and manuscript drafting were performed by all authors. All authors read and approved the final manuscript.
Acknowledgment
We would like to thank our team who gave me a golden opportunity to work on this project. We’d also like to express our gratitude to laboratory of research who gave us such an opportunity to explore this subject.
References
- Estimativa 2018:Incidência de Câncer No Brasil (1st ed). Rio de Janeiro: Instituto Nacional de Câncer; 2017.
- Long-term morbidities in children with critical illness:Gaps and opportunities. Ann Acad Med Singapore. 2018;47:291-337.
- [Google Scholar]
- PICU mortality of children with cancer admitted to pediatric intensive care unit a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2019;142:153-63.
- [Google Scholar]
- The role of rehabilitation specialists in canadian NICUs:A 21st century perspective. Phys Occup Ther Pediatr. 2019;39:33-47.
- [Google Scholar]
- Effects of a combined physical and psychosocial training for children with cancer:A randomized controlled trial. BMC Cancer. 2018;18:1-12.
- [Google Scholar]
- Physical exercise training interventions for children and young adults during and after treatment for childhood cancer. Cochrane Collab. 2016;4:1-50.
- [Google Scholar]
- A systematic review of exercise systematic reviews in the cancer literature. PM R. 2017;9:S347-84.
- [Google Scholar]
- Respiratory care considerations in the childhood cancer patient. Respir Care. 2017;62:765-75.
- [Google Scholar]
- PEDro:A base de dados de evidências em fisioterapia. Fisioter Em Mov. 2011;24:523-33.
- [Google Scholar]
- Evidence for physiotherapy practice:A survey of the physiotherapy evidence database (PEDro) Aust J Physiother. 2002;48:43-9.
- [Google Scholar]
- Noninvasive ventilation in immunocompromised pediatric patients:Eight years of experience in a pediatric oncology intensive care unit. J Pediatr Hematol Oncol. 2008;30:533-8.
- [Google Scholar]
- Respiratory failure in children with hemato-oncological diseases admitted to the PICU:A single-center experience. J Pediatr Hematol Oncol. 2015;37:449-54.
- [Google Scholar]
- Bi-level positive airway pressure ventilation in pediatric oncology patients with acute respiratory failure. J Intensive Care Med. 2009;24:383-8.
- [Google Scholar]
- Permissive hypercapnia for severe acute respiratory distress syndrome in immunocompromised children:A single center experience. PLoS One. 2017;12:1-14.
- [Google Scholar]
- The use of high frequency oscillatory ventilation in a pediatric oncology intensive care unit. Pediatr Blood Cancer. 2012;58:384-9.
- [Google Scholar]
- Survival in a recent cohort of mechanically ventilated pediatric allogeneic hematopoietic stem cell transplantation recipients. Biol Blood Marrow Transplant. 2008;14:1385-93.
- [Google Scholar]
- Treatment of children with cancer and/or hematopoietic stem cell transplantation in the intensive care unit:Experience at a Large European pediatric cancer center. J Pediatr Hematol Oncol. 2020;42:e583-8.
- [Google Scholar]
- Noninvasive ventilation during acute respiratory distress syndrome in patients with cancer:Trends in use and outcome. J Crit Care. 2017;38:295-9.
- [Google Scholar]
- Pediatric acute respiratory distress syndrome:Consensus recommendations from the pediatric acute lung injury consensus conference. Pediatr Crit Care Med. 2015;16:428-39.
- [Google Scholar]







