Translate this page into:
Urinary tissue inhibitor of metalloproteinase-2 as an early predictor for acute kidney injury in critically ill children
Address for correspondence: Maha A. Abouhadid, Arrowe Park Road, Upton, Birkenhead, Wirral, CH49 5PE. Phone: +447946222783. E-mail: maha.abouhadid@nhs.net
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Qassim Uninversity and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
Acute kidney injury (AKI) is one of the most devastating complications of critical illness in children. Serum creatinine (Scr) is considered the gold standard for AKI diagnosis yet noted to be late and inaccurate. This raises the need for an early and accurate biochemical parameter for the early detection of AKI. This research aimed to explore the role of urinary tissue inhibitor metalloproteinase 2 (TIMP-2) in the early prediction of AKI, compared to standard biomarkers, in critically ill children admitted to pediatric intensive care unit (PICU). Urine TIMP2 was previously explored in multiple adult studies and showed promising results; however, the study of its role in pediatric population was limited.
Methods:
This study was a prospective cohort study including 42 critically ill children who are at increased risk of AKI. Cases were recruited from the PICU in the Children’s Hospital of Ain-Shams University, Cairo – Egypt over 10 months’ duration. Urine samples were collected to measure urinary TIMP-2 and blood samples were taken to measure the levels of Scr, creatinine clearance, and blood urea nitrogen. Urine output in 24 h was also calculated.
Results:
Urinary TIMP-2 showed considerably higher levels in AKI compared to non-AKI patients as early as day 1, whereas increased levels of Scr and decreased urine output were noticed later (day 3 and day 5, respectively). A notable correlation existed between TIMP-2 at day 1 and creatinine at day 3.
Conclusion:
The present study revealed that urinary TIMP-2 could have an important role in the early prediction of AKI before the increase in Scr and more deterioration in kidney functions.
Keywords
TIMP-2
Acute Kidney Injury
Critically- Ill Children
Introduction
Acute kidney injury (AKI) is more likely to occur in critically ill children. AKI can be linked to a variety of short-term and long-term kidney impairment as well as higher likelihood of morbidity and mortality in the intensive care unit (ICU). Following admission to pediatric ICU (PICU), the incidence of AKI varies from 4.5 to 31%, being much higher in children who are requiring invasive mechanical ventilation or patients with sepsis or septic shock and those on vasopressor medications. The process of kidney injury takes place before any change in kidney functions could be detected. The early prediction of AKI particularly in critically ill patients is mandatory because it can allow early management procedures which will prevent further deterioration of the patient’s condition. These interventions include conservative measures such as stopping nephrotoxic drugs and performing an accurate fluid and electrolyte balance which can avoid the need for short-term or even lifelong dialysis.[1,2]
Serum creatinine (Scr) is still considered the basic diagnostic tool for AKI patients.[3,4] However, Scr levels increase above normal values only when 25–50% of the renal function has been impaired. Therefore, there may be a dissociation between deterioration of kidney functions and Scr levels.[5] Many biomarkers for the early prediction of AKI have been previously identified including NGAL, KIM-1, cystatin-C, L-FABP, and interleukin-18.[2,6] When AKI is associated with severe sepsis, certain markers including NGAL may have decreased predictive performance.[7] More recently, a new test has been investigated that relies on the measurement of the level of cell cycle arrest biomarkers, such as tissue inhibitor metalloproteinase 2 (TIMP-2) for the early detection of AKI cases.[1-8]
Tissue inhibitor of metalloproteinase-2 is a 21-kilo Dalton protein of the TIMP family. It is an inhibitor of metalloproteinase endogenous activities.[9] It is released during the cell cycle arrest (G1) in the early phases of cellular injury. During this early phase of renal injury following ischemia, the cells of the renal tubules enter short periods of G1 cell cycle arrest during which this marker is released. Therefore, an increased TIMP-2 level is assumed to occur early in the process of AKI.[10,11]
The Kidney Disease Improving Global Outcomes (KDIGO) criteria suggested that urine TIMP-2 outperforms the other markers available till now in the early prediction of moderate and severe AKI in adult patients. Furthermore, some studies showed that the higher the level of TIMP-2, the higher the morbidity and mortality in AKI patients.[12] The previous research considered it as a marker for the early detection of AKI, especially in the critically sick patients who have concomitant sepsis.[8,13,14] However, this marker is not fully investigated in pediatric population.
The patients who develop AKI have significantly higher mortality risk and the survivors are at higher risk of short-term and long-term complications.[11] The available treatment modalities for AKI are mainly supportive including stopping any nephrotoxic agents and/or renal dialysis. However, there is no definitive treatment for these patients yet. Therefore, a proper risk assessment for patients with AKI is highly advised because this will help in early management and better outcomes.[15,16] The present research aimed to study the frequency of occurrence of AKI in a busy PICU and to assess the contribution of urinary TIMP-2 in the early prediction of AKI in critically ill children.
Methods
Subjects and methodology
This is a prospective cohort study which included 42 critically ill children admitted to PICU, Children’s Hospital, Ain-Shams University, Cairo-Egypt for 10 months’ duration from August 2016 to May 2017. Their age ranged from 2 months to 5 years old with a median interquartile range (IQR) age of 0.50 (0.25–1.50) years. Cases were recruited using consecutive sampling technique. Sample size was limited to the study budget and time frame of the study taking into consideration that the number of recruited cases is statistically appropriate. Inclusion criteria: Critically ill infants and children who are at increased risk of AKI were included in the study. The primary diagnosis included sepsis/septic shock post major surgeries and children needing vasopressor or inotropic support. Sepsis was defined according to Pediatric Sepsis Consensus Conference (PSCC) 2005 as systemic inflammatory response syndrome (SIRS) in the presence of, or as a result of, suspected or proven infection, whereby SIRS comprises temperature dysregulation (defined as core body temperature >38.5 or <36°C); tachycardia (defined as a mean heart rate >2 SD above normal for age), bradycardia (defined as a mean heart rate <10% for age), and respiratory rate dysregulation (defined as a mean respiratory rate >2 SD above normal for age or mechanical ventilation for an acute process not related to underlying neuromuscular disease or the receipt of general anesthesia); and leucocyte count elevated or depressed for age, or >10% immature neutrophils. (Ref) Septic shock was defined as presence of sepsis and cardiovascular organ dysfunction in the PSCC definition.[17] AKI was defined as any of the following based on KDIGO criteria: Increase in S.Cr by ×0.3 mg/dL (×26.5 lmol/L) within 48 h; or increase in S.Cr to × 1.5 times baseline, which is known or presumed to have occurred within the prior 7 days; or urine volume of 0.5 mL/kg/h for 6 h.[18] Exclusion criteria: Age <1 month and more than 5 years old and those with chronic kidney diseases were excluded from the study.
Patients were subjected to full medical history including age, sex, cause of PICU admission, days of PICU stay, and outcome. Assessment of the degree of critical illness using sequential organ failure assessment (SOFA) and pediatric risk of mortality (PRISM) scores: the sepsis-related organ failure assessment score (SOFA score) is used to monitor a person’s status in an ICU to identify the extent of their organ function.[19]
PRISM score is used for PICU mortality risk assessment with score 0 indicating 0% mortality risk and a score 76 indicating 100% mortality risk.[20] SOFA score provides a mean of quantitatively and objectively describes the degree of organ failure over time in critically ill patients, through the assessment of six systems: Respiratory, coagulation, hepatic, cardiovascular, central nervous system, and renal. A score of 0 is given for normal function through to 4 for most abnormal, and the worst values on each day are recorded.[19]
Laboratory investigations
Urine samples: 10 mL of urine were collected under complete aseptic conditions in a sterile container at days 1 and 3 after PICU admission to measure urinary TIMP-2. Samples were immediately centrifuged to remove particulate matter and stored in aliquot at ≤−80°C until assay by ELISA technique (Human TIMP-2 Quantikine ELISA kit- R&D systems, Inc. Minneapolis, MN55413 USA).
Blood samples
3 ml of blood were collected from each patient at days 1, 3, and 5 to measure Scr by spectrophotometric method as per routine PICU procedures using Cobas 6000 Roche. A kinetic colorimetric assay based on the Jaffe method. In alkaline solution, creatinine forms a yellow-orange complex with picrate. The rate of dye formation is proportional to the creatinine concentration in the specimen. The essay uses “rate- blanking” to minimize interference by bilirubin.
Ethical consent
Ethical approval from the Ethical Committees of the Faculty of Postgraduate Childhood Studies and the National Research Center was taken, with commitment to the ethical considerations. Informed consents were obtained from the parents or caregivers after explanation of the aim of the study and its possible benefits for early detection of AKI.
Statistical analysis
All the statistical calculations were done using computer programs and Statistical Package for the Social Sciences version 16. Data were presented and suitable analysis was done according to the type of data obtained for each parameter.
The mean ± standard deviation was used for the parametric and numerical data, while the median and IQR were used for non-parametric numerical data. The frequency and percentage were a measure of non-numerical data. On the other hand, student t-test was used to assess the statistical significance of the difference between the means of two study groups. The Pearson’s correlation analysis was used to assess the strength of association between two quantitative variables. The correlation coefficient was denoted symbolically as “r.” Finally, Paired t-test was used to assess statistical significance of the difference between two means that are measured twice for the same study group. The Mann–Whitney U-test was used to compare differences between two independent groups when the dependent variable is either ordinal or continuous, but not normally distributed. P-value was considered significant at <0.05 and highly significant at <0.001.
Results
Demographic data of the studied group
Demographic data of studied patients is shown in Table 1.
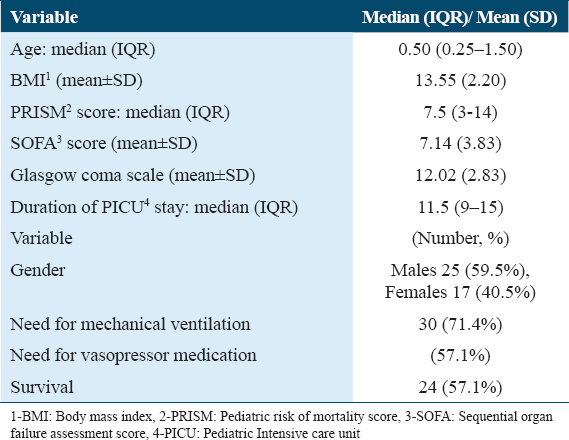
The patients’ age ranged from 2 months to 5 years and their body weight ranged from 3 to 21 kg. The most common diagnoses in our studied cohort were sepsis and septic shock (33.3%), post-operative patients (26%), and chest infection (24%) [Figure 1]. The mean SOFA score in the studied population was around 7 with values ranging from (2 to 14). PRISM score ranged from 2 to 23 in the studied population with a median value 7.5 [Table 1].
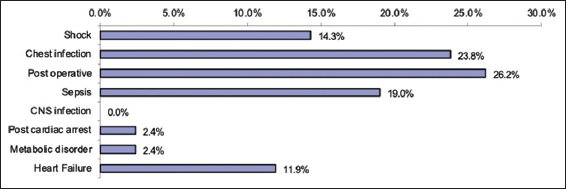
- Diagnosis of the studied patients
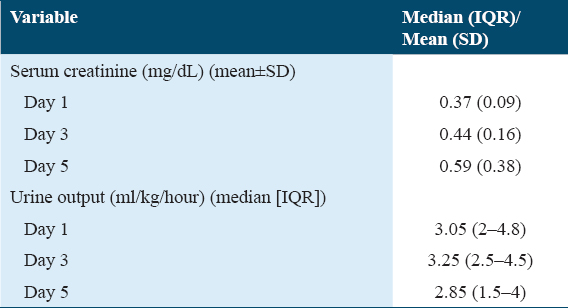
Levels of Scr and urine output at day 1, day 3, and day 5
Table 2 shows the median (IQR) levels of Scr, and urinary output at days 1, 3, and 5. Mean Scr at day 1 was 0.37 (0.09). This was increased to 0.59 (0.38) at day 5. The median (IQR) levels of urine output in contrast were gradually decreasing being 3.05 (2–4.8) at day 1 and 2.85 (1.5–4) at day 5.
Patient subgroups and comparative data
AKI was diagnosed according to KDIGO criteria and accordingly studied cases were divided into AKI group (13, 31%), and non-AKI group (29, 69%). The age of the studied group was substantially lower in patients with AKI compared to patients who did not have AKI (P = 0.031).
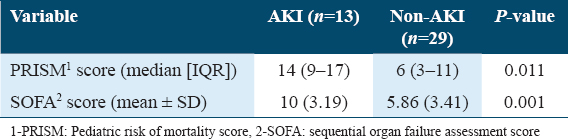
Table 3 shows the comparison of PICU scores PRISM and SOFA between AKI and non-AKI cohorts where both showed significantly higher levels in AKI group.
As regards kidney function tests including Scr, blood urea nitrogen (BUN), and creatinine clearance [Table 4], AKI patients did not show a significant increase in creatinine levels until day 3, whereas significant decrease in urine output was recorded at day 5, with median (IQR) values 1 (0.6–1.5) versus 3.5 (2.8–5), respectively. On the other hand, urinary TIMP-2 levels were significantly higher in AKI group starting from day 1.
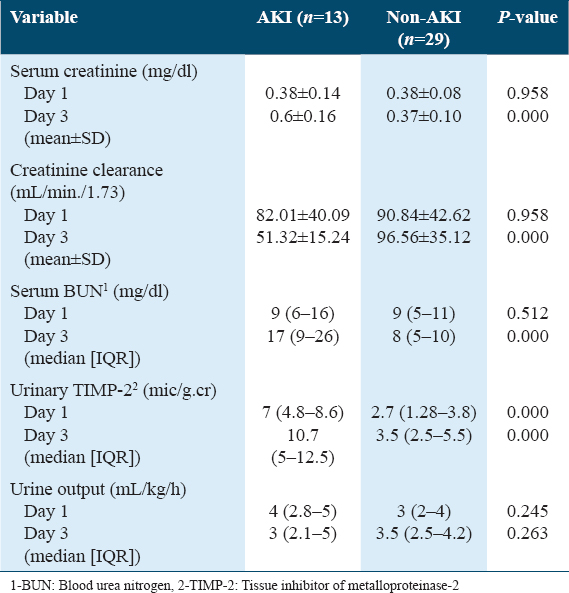
Follow-up of different studied parameters
By follow-up of the measured parameters on days 1, 3, and 5, it was found that both serum BUN and urine TIMP-2 levels showed highly significant difference in AKI group between day 1 and day 3 [Table 4]. Similarly, both Scr and creatinine clearance showed highly significant differences in AKI group between day 1 and day 3. Urine output levels decreased significantly in AKI group from day 1 to day 5 with median (IQR) values 4 (2.8–5) versus 1 (0.6–1.5) mL/kg/h, respectively. On the other hand, urine TIMP-2 levels showed a high statistically significant difference in non-AKI group between day 1 and day 3; however, levels remained within normal range in this category.
Causes of PICU admissions and outcome in both study groups
Sepsis and septic shock are the two major causes of admission in AKI patients compared to non-AKI, where post-operative and chest infection cases were more prominent. A highly significant statistical difference was found between the outcomes in both groups, with a mortality of around 77% in AKI patients. The duration of PICU stay was not statistically significant between the two groups in our studied population.
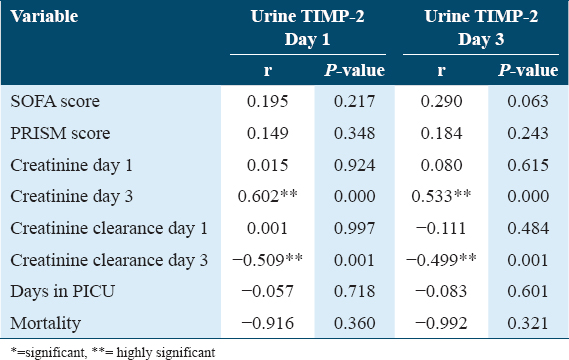
Correlation of data
Table 5 and Figure 2 show different correlations of the study. There was a positive correlation between urinary TIMP-2 at day 1 and Scr/creatinine clearance at day 3. A positive correlation was also found between urinary TIMP-2 at day 3 and Scr/creatinine clearance at day 1 and day 3. Urinary TIMP-2 levels at day 1 and day 3 were not correlated to the duration of PICU stay or patients’ outcome.
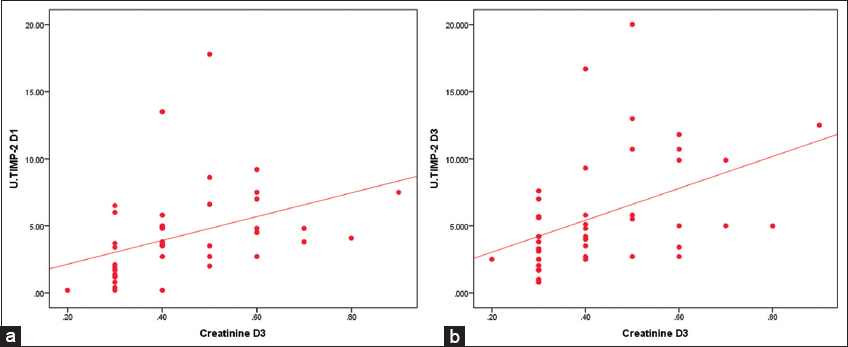
- (a) Correlation between urine TIMP2 at day 1 and serum creatinine at day 3. (b) Correlation between urine TIMP2 and serum creatinine at day 3
Discussion
Children with critical illness are highly vulnerable to developing AKI. AKI can lead to increased risk of morbidity and mortality in the ICU. It is also linked to a variety of short-term and long-term complications. AKI is a process that takes place long before it is evident in laboratory markers, and till present, there is no available definitive treatment for AKI apart from different supportive modalities. Hence, it is mandatory to early predict the patients who have high risk of developing AKI and to take steps to prevent it, such as stopping nephrotoxic medicines and taking other precautions.[1,2,12]
In the present study, the most prevalent cause of PICU admission in our cohort was sepsis and septic shock (33.3%) [Figure 1]. This was in accordance with Westhoff et al.[11] who found in their work that the most common reasons of ICU admission were sepsis and septic shock (45.6%). Ferrari and co-workers[6] found that the most frequent cause of admission to PICU was trauma (20.60%), followed by sepsis (18.32%).
In the present study, 31% of our studied patients developed AKI. This percent was higher than that reported by Bell et al.[21] where only 20% of their patients developed AKI. The higher frequency of AKI in our work could be justified by the poor general condition of included patients as one-third of them had sepsis, and as indicated by high PRISM and SOFA scores. In agreement with our results, the previous research stated that AKI occurred in around 30-50% of ICU patients.[6,22,23] Esmeijer et al.[3] affirmed that ICU patients and particularly those undergoing cardiac operations are more vulnerable to develop AKI.
In the current research, AKI was substantially higher in the younger age group, with median (IQR) age in AKI group 0.25 (0.2–0.7) years compared to 0.7 (0.4–2) years in non-AKI group. In accordance with our study, Gupta et al. found that AKI was more common in the younger age group compared to non-AKI.[24] On the other hand, other studies did not relate AKI to a particular age group.[11,16,23]
The major primary diagnosis in the AKI group was sepsis and septic shock (69.3%). This was in accordance with two previous studies who found that in the AKI patients, sepsis was the most common cause (45.6% and 41.8%), respectively.[11,12] Moreover, the in previous research completed by Omar et al.[23] who recruited 232 sepsis patients in their study, 40 patients (17%) developed AKI within 12 h.
Critical illness scores, SOFA and PRISM scores, were substantially higher in AKI group compared to non-AKI [Table 3]. This was in concordance with a previous study[25] which found that most of their AKI patients (60%) had high critical illness scores due to concomitant severe chest infection and sepsis/septic shock. Moreover, Gogia and Koreti[26] found that AKI was found to be positively correlated to higher SOFA score and mortality with a mean SOFA score (10.48 ± 2.5) in those who did not survive and (8.41 ± 3.39) in the survivors. Furthermore, Xie et al.[10] found that SOFA score was higher in AKI group.
Kidney function tests did not rise in the patients developing AKI until day 3 of PICU admission [Table 4]. This indicates that although Scr is an accurate marker for diagnosing AKI, it is a late one. This was affirmed by Andreoli[27] who mentioned that Scr concentration is a late marker of impaired kidney function after AKI. Moreover, Ashraf et al.[28] stated that diagnosing pediatric AKI with rising Scr is not an accurate marker during acute kidney impairment as Scr would not rise until the glomerular filtration rate (GFR) has decreased moderately (about 40 mL/min/1.73 m2). Moreover, Scr is deemed non-specific indicator for GFR changes as it cannot explain the exact cause and place of kidney impairment (e.g., prerenal, or intrinsic renal; ischemic or nephrotoxic). Furthermore, the extent of damage to the kidneys is not accurately reflected by Scr concentrations.[23]
As regards urine output [Table 4], there was no significant decrease in UOP in AKI group till day 5, which is not usually expected in these cases, as oliguria is usually an earlier sign of AKI; this can be explained by early fluid resuscitation in those critically ill patients which maintained renal blood flow. This was stated by Moussa et al., who found that improvement in the kidney perfusion and increased urine output was seen in response to administration of fluid, even if no change blood pressure and renal blood flow were seen.[29]
On the other hand, urinary TIMP-2 median levels were substantially higher in patients with AKI compared to others who did not develop AKI [Table 4] in days 1 and 3. Furthermore, we elicited a significant positive association between urinary TIMP-2 at day 1 and Scr/creatinine clearance at day 3 [Table 5 and Figure 2a and b]. This addresses TIMP-2 as promising marker for the early detection of AKI. Gunnerson et al.[30] found that the measurement of urinary TIMP-2 performed well in detecting moderate to severe AKI. This was observed in many studies performed on critically ill adults, where Pajenda et al.[31] noticed a brisk increase in urinary TIMP-2 after renal tubular insult in most cases who developed AKI, and that a significant decrease indicated the improvement of kidney functions. Furthermore, Omar et al.[23] in their study on post-operative cardiac patients, pre- and post-operative measurements of urine TIPM2 levels were deemed significantly higher in the AKI cohort compared to non-AKI group. Similar results were reported by Westhoff et al.,[11] Cuartero et al.,[32] and Yamashita et al.[12]
AKI is known to cause increased mortality in PICU patients.[33] In the studied population, highly significant statistical difference was found between the outcomes of both groups, with a mortality of 76.9% in the AKI, and only 27.6% in the non-AKI patients. Higher mortality in AKI group could be attributed to different factors, as the add-on insult of AKI on the initial condition, leads to acid base disturbance, electrolyte derangement, and volume overload. Similar results were reported in different studies where AKI impacted higher mortality risk.[10,30,34] However, no significant difference in length of stay in PICU was noticed in both groups.
Conclusions and Recommendations
AKI is common in the critically ill children especially in patients admitted with sepsis and septic shock. Urinary TIMP-2 could have a role in early prediction of AKI before rise in Scr and more deterioration in kidney functions. The early detection of AKI must be considered in all children admitted in the ICU. This can be done by markers like urinary TIMP-2 as this will help in the early management and better prognosis. Further studies on a larger scale are recommended to validate the effectiveness of urinary TIMP-2 as an early predictor of AKI in the pediatric population.
Ethics Approval and Consent to Participate
Ethical approval from the Ethical Committee of the National Research Center as well as the Faculty of Postgraduate Childhood Studies was taken, with a commitment to ethical considerations. Parents provided verbal informed consent after an explanation of the aim of the study and the potential benefits for AKI early detection.
Consent for Publication
Not Applicable – No patient identifiable information included.
Availability of Data and Material
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Funding Statement
The practical part of this work has been funded by the National Research Center (NRC), Dokki, Giza, Egypt.
Authors’ Contributions
MA gathered data, analyzed results, and wrote the manuscript. AA revised and approved the final the manuscript. NA performed the laboratory tests and all authors contributed since the beginning of the research in review, ideas, and approval of the manuscript.
Acknowledgments
Authors wish to express their gratitude to NRC for funding the practical part of this work and thanks to caregivers of patients for their co-operation.
References
- Tissue inhibitor metalloproteinase 2 (TIMP-2) and insulin-like growth factor binding protein 7 (IGFBP7) best predicts the development of acute kidney injury. Heliyon. 2021;7:e07960.
- [Google Scholar]
- Towards a biomarker panel for the assessment of AKI in children receiving intensive care. Pediatr Nephrol. 2015;30:1861-71.
- [Google Scholar]
- The predictive value of TIMP-2 and IGFBP7 for kidney failure and 30-day mortality after elective cardiac surgery. Sci Rep. 2021;11:1071.
- [Google Scholar]
- Renal angina:An emerging paradigm to identify children at risk for acute kidney injury. Pediatr Nephrol. 2012;27:1067-78.
- [Google Scholar]
- Acute kidney injury in critically ill newborns:What do we know?What do we need to learn? Pediatr Nephrol. 2009;24:265-74.
- [Google Scholar]
- Routine adoption of urinary [IGFBP7] [TIMP-2] to assess acute kidney injury at any stage 12 hours after intensive care unit admission:A prospective cohort study. Sci Rep. 2019;9:16484.
- [Google Scholar]
- Predictive value of plasma neutrophil gelatinase-associated lipocalin for acute renal failure in patients with severe sepsis. J Chin Med Assoc. 2016;79:428-34.
- [Google Scholar]
- Renal replacement therapy in acute kidney injury:Controversy and consensus. Crit Care. 2015;19:146.
- [Google Scholar]
- Biomarkers of acute kidney injury:The pathway from discovery to clinical adoption. Clin Chem Lab Med. 2017;55:1074-89.
- [Google Scholar]
- Tissue inhibitor metalloproteinase-2 (TIMP-2) IGF-binding protein-7 (IGFBP7) levels are associated with adverse outcomes in patients in the intensive care unit with acute kidney injury. Kidney Int. 2019;95:1486-93.
- [Google Scholar]
- Evaluation of urinary tissue inhibitor of metalloproteinase-2 in acute kidney injury:A prospective observational study. Crit Care. 2014;18:716.
- [Google Scholar]
- Tissue inhibitor metalloproteinase-2 (TIMP-2). IGF-binding protein-7 (IGFBP7) levels are associated with adverse long-term outcomes in patients with AKI. J Am Soc Nephrol. 2015;26:1747-54.
- [Google Scholar]
- Urinary tissue inhibitor of metalloproteinase-2 (TIMP-2) insulin-like growth factor-binding protein 7 (IGFBP7) predicts adverse outcome in pediatric acute kidney injury. PLoS One. 2015;10:e0143628.
- [Google Scholar]
- Urinary TIMP2 and IGFBP7 identifies high risk patients of short-term progression from mild and moderate to severe acute kidney injury during septic shock:A prospective cohort study. Dis Markers. 2019;2019:3471215.
- [Google Scholar]
- Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care. 2013;17:R25.
- [Google Scholar]
- Urinary TIMP-2 and IGFBP7 as early biomarkers of acute kidney injury and renal recovery following cardiac surgery. PLoS One. 2014;9:e93460.
- [Google Scholar]
- International Consensus Conference on Pediatric Sepsis International pediatric sepsis consensus conference:Definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6:2-8.
- [Google Scholar]
- Kidney disease:Improving global outcomes (KDIGO)- clinical practice guideline for acute kidney injury Kidney Int. 2012;2:1-138.
- Acute renal failure in the ICU:Risk factors and outcome evaluated by the SOFA score. Intensive Care Med. 2000;26:915-21.
- [Google Scholar]
- Managing the Internal Evaluation Process. In: The Business of Critical Care:A Textbook for Clinicians who Manage Special Care Units. Netherlands: Elsevier; 1996. p. :167.
- [Google Scholar]
- Assessment of cell-cycle arrest biomarkers to predict early and delayed acute kidney injury. Dis Markers. 2015;2015:158658.
- [Google Scholar]
- Urinary biomarkers TIMP-2 and IGFBP7 early predict acute kidney injury after major surgery. PLoS One. 2015;10:e0120863.
- [Google Scholar]
- Urinary tissue inhibitor of metalloproteinases-2 as early biomarker of acute kidney injury after cardiac surgery. Eur J Mol Clin Med. 2021;8:2515-8260.
- [Google Scholar]
- Acute kidney injury in Pediatric Intensive Care Unit:Incidence, risk factors, and outcome. Indian J Crit Care Med. 2016;20:526-9.
- [Google Scholar]
- Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007;71:1028-35.
- [Google Scholar]
- SOFA (Sequential organ failure assessment) and PELOD (Pediatric logistic organ dysfunction) Sch J App Med Sci. 2015;3:1645-8.
- [Google Scholar]
- Pediatric acute kidney injury:A syndrome under paradigm shift. Indian J Crit Care Med. 2014;18:518-26.
- [Google Scholar]
- Effects of fluid administration on renal perfusion in critically ill patients. Crit Care. 2015;19:250.
- [Google Scholar]
- TIMP2 IGFBP7 biomarker panel accurately predicts acute kidney injury in high-risk surgical patients. J Trauma Acute Care Surg. 2016;80:243.
- [Google Scholar]
- NephroCheck data compared to serum creatinine in various clinical settings. BMC Nephrol. 2015;16:206.
- [Google Scholar]
- Cell-cycle arrest biomarkers in urine to predict acute kidney injury in septic and non-septic critically ill patients. Ann Intensive Care. 2017;7:92.
- [Google Scholar]
- An integrative view of the pathophysiological events leading to cisplatin nephrotoxicity. Crit Rev Toxicol. 2011;41:803-21.
- [Google Scholar]
- Validation of cell-cycle arrest biomarkers for acute kidney injury using clinical adjudication. Am J Respir Crit Care Med. 2014;189:932-9.
- [Google Scholar]







